![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
152 Cards in this Set
- Front
- Back
|
In a patient with cold agglutinin disease what RBC index is still reliable?
|
Hemoglobin
|
|
|
Hemiglobin cyanide (HiCN) is measured at what wavelength ?
It measures what types of hgb? It does not measure? |
540 nm
Measures Oxyhgb, Deoxyhgb, Carboxyhgb, and methemoglobin (Hi) Does NOT measure Sulfhgb |
|
|
corrected retic count = ?
Absolute retic count = ? Retic production index = ? |
CRC = % retics x Hct/45
Abs retic count = % retics x RBC count RPI = CRC x 1/correction factor CF = 1.0 when Hct is normal, 2.0 when Hct is 30 and 3.0 when Hct is 15 |
|
Increased LDH, decreased haptoglobin increased free Hgb, hemoglobinuria, no splenomegaly
|
Intravascular hemolysis
|
|
increased LDH, decreased haptoglobin, increased indirect bili, increased fecal and urine urobilinogen, splenomegaly
|
Extravascular hemolysis
|
|
|
+ for any spherocytes present
|
Osmotic fragility test
|
|
|
Differential for spherocytosis/extravascular hemolysis?
How to differentiate them? |
Autoimmune hemolytic anemia (AIHA):
DAT+, low MCV Hereditary spherocytosis (HS): DAT(-), normal MCV, autohemolysis test + |
|
|
Hereditary Spherocytosis inheritance pattern?
defect? Which RBC index is most consistently abnormal/increased? |
AD
ANKYRIN (most common), band 3, protein 4.2 or spectrin MCHC |
|
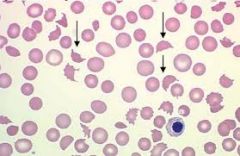
Differential?
|
Iron deficiency anemia -pencil cells can rule this in.
Hereditary elliptocytosis B12/Folate deficiency myelodysplasia myelophthisis |
|
|
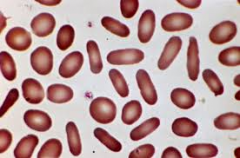
Definition of Hereditary elliptocytosis
|
>25% elliptocytes
cell must be 2x longer than wide |
|
|
Hereditary elliptocytosis - stomatocytic type protects against which malarial organism?
|
P. vivax
|
|
|
defect in Hereditary elliptocytosis?
|
SPECTRIN alpha or beta (most common)
protein 4.1 glycophorin C |
|
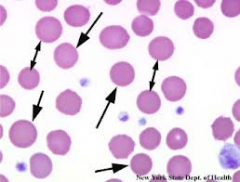
Differential?
|
Rh null
Phenothiazine Alcohol Liver disease Hereditary stomatocytosis |
|
|
Most common etiology in Hereditary stomatocytosis?
|
Abnormal Na/K permeability
|
|
|
Patient with extravascular hemolysis and thrombosis after splenectomy. What will PBS most likely contain?
|
stomatocytes
Hereditary stomatocytosis |
|
differential for Heinz bodies, blister cells, and bite cells?
|
G6PD deficiency
Unstable hemoglobins Sulfhemoglobinemia Hb H Hb Barts Heinz bodies are denatured hemoglobin |
|
|
Heinz bodies are evidence of?
|
oxidized hemoglobin
|
|
|
G6PD inheritance?
|
X-linked recessive
|
|
|
What is the best time to perform diagnostic testing for G6PD deficiency? Why?
|
3 months post hemolytic crisis
False negative may result directly after hemolysis |
|
|
NADPH and NADH aborbs light at what wavelength?
|
340 nm
|
|
|
Which RBC indices are measured directly?
Which are calculated? |
RBC, MCV, and RDW measured directly
Hct, MCH, MCHC |
|
|
Hct =
MCHC = |
Hct = MCV x RBC
MHCH = Hb/Hct x 100 |
|
|
prekeratocyte
associated with iron-deficiency anemia |
|
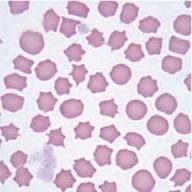
Burr cells/echinocytes/dessicocytes differential? pointy ends
|
Artifact
Uremia burns PK deficiency |
|
|
Pyruvate kinase deficiency inheritance?
Associated with what populations? |
AR
Northern European, Pennsylvania Amish |
|
Acanthocytes/spur cells differential?
clubbed ends |
Liver dz
Abetalipoproteinemia Mcleod phenotype Post-splenectomy |
|
|
Acanthocytosis, retinitis pigmentosa, hypocholesterolemia
Steatorrhea, ataxia Dx? inheritance pattern? |
Abetalipoproteinemia
autosomal recessive |
|

Alkaline gel electrophoresis Hemoglobins from + to -
|
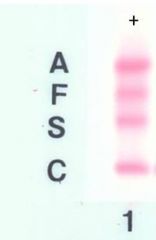
A F S C
|
|
|
pancellular K-B test indicates ?
|
HPFH
normal neonate |
|
|
heterocellular K-B test?
Heterogeneous |
fetomaternal hemorrhage
Hemoglobinopathies (SS, beta-thalassemia) Childhood CML B12/folate deficiency EPO tx |
|
|
Hemoglobins that run with S on alkaline gel?
|
D, G, Lepore
|
|
|
Prevalence of Sickle cell trait (SA) in African-Americans?
mutation? |
10%
point mutation chrom 11 causing glutamate to be replaced with valine at the 6th position in the beta chain. beta6glu-->val |
|
|
average lifespan of RBCs in HBSS
|
17 days
|
|
|
Presence of HbF does what to HbS?
|
inhibits polymerization of HbS
|
|
|
Accounts for the majority of aplastic crises in children with sickle cell disease.
|
Parvovirus B19
|
|
|
7 classic sickle cell nephropathies
|
gross hematuria
papillary necrosis nephrotic syndrome renal infarction isosthenuria - inability to concentrate urine pyelonephritis renal medullary carcinoma |
|
|
In SS disease what is the percentage of HgbS?
In SA trait? In SC disease? In S-alpha thalassemia? In S-beta thalassemia? |
>80%
35-45% 50% S, 50% C 30-40% S in 1-gene del, 25-30% S in 2-gene del >50% S |
|
|
SC disease 2 complications that are equally common or more common than in SS?
|
avascular necrosis and proliferative retinopathy
|
|
|
Hemogloblin C substitution?
|
Beta6glu-->lys
Glutamate replaced with lysine at position 6 in beta chain |
|
|
HbE substitution?
|
beta26glu-->lys
|
|
|
HbS on electrophoresis at 15%. What should you suspect?
|
Hb Lepore
|
|
|
Hb that is the result of a fusion between delta and beta genes.
|
Hb Lepore
|
|
|
In methemoglobin what ion is bound to hemoglobin?
tx for methemoglobinemia? |
Fe+++ Ferric state
methylene blue |
|

Acid gel hemoglobin electrophoresis.
What is the order of hemoglobins anode + to cathode - ? |
C S A F
|
|
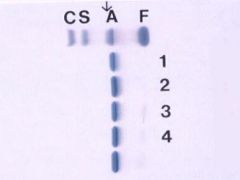
Patient is in lane 1. The above is agarose (acid) gel.
On cellulose (alkaline) gel there was an abnormal hemoglobin in the C lane. What is the likely hemoglobin? What geographic region? |
Hb E, Southeast Asia, will have thalassemic traits
On alkaline gel E, O and A2 run with C. A2 is usually < 3.5%. On acid gel, E and O run with A. Could also be Hb O, clinically normal |
|
|
What is a classic slow-migrating hemoglobin on alkaline?
|
Constant Spring
|
|
|
What are the fast migrating hemoglobins?
|
Hb Barts = gamma 4
Hb H = beta4 |
|
|
Beta-globin gene cluster includes ?
|
beta, delta, gamma, and pseudo-beta
|
|
|
Hb Constant Spring mutation in ?
|
alpha gene stop codon producing abnormally long transcript that is unstable.
|
|
|
Patient with left-shifted O2 dissociation curve. Gel and HPLC appear normal but there is erythrocytosis on CBC. What hemoglobins are implicated?
|
Hb Chesapeake and Hb Denver -- high O2 affinity hemoglobins
|
|
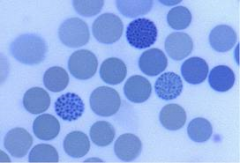
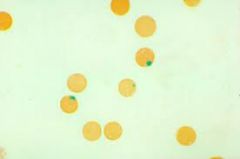
What stain? What hemoglobin?
|
cresyl blue
Hb H (beta tetramer) |
|

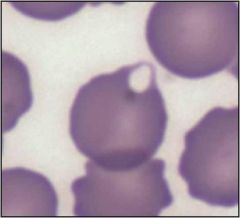
What is this test?
|
dithionate - Sickle solubility test.
left is negative, right is positive for Hb S |
|
|
Most frequent genetic cause of beta0 allele production?
|
point mutations
|
|
|
Thalassemic indices
|
elevated RBC count (> 5.5 men and 5.0 women x10^12)
low MCV (65-75 fL in alpha, 55-65 fL in beta)) low Hct normal to slightly increased RDW MCV/RBC ratio <13 |
|
|
Common confounding factor that causes beta-thalassemia to be dxed as alpha-thalassemia based on Hb electrophoresis?
|
Iron deficiency
|
|
|
alpha thalassemic trait
which genotype is common to Asians and which to Africans? |
-a/-a common in Africans
--/aa common in Asians |
|
|
Acquired Hb H may be seen in what disorders?
|
erythroleukemia
myeloproliferative disorders myelodysplastic syndromes |
|
|
beta thalassemia minor genotypes
|
beta/beta+, beta/beta0
|
|
|
beta thalassemia major genotypes
what distinguishes as major? |
beta0/beta0
beta+/beta0 transfusion dependent |
|
|
hemoglobin components
HbA HbA2 HbF |
A: alpha2/beta2
A2: alpha2/delta2 F: alpha2/gamma2 |
|
|
Sulfhemoglobin causes
|
Sulfa-containing agents
C. perfringens - enterogenous cyanosis |
|
|
Cyanosis with chocolate-brown blood
|
Methhemeglobinemia
|
|
|
Cyanosis with cherry-red color
|
Carboxyhemoglobinemia
or cyanide |
|
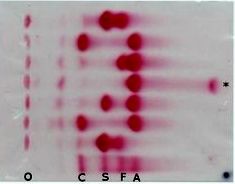
What is represented at * ?
|
HbH
fast migrating hb |
|
|
thalassemia intermedia
|
beta+/beta+
beta/beta0 not transfusion dependent |
|
|
Which organ is spared in Gaucher's disease?
|
brain
|
|
|
Positive acidified serum test (Ham) in heterologous serum only.
|
CDA II Congenital dyserythropoietic anemia
PNH is + in both autologous and heterologous serum. |
|
|
high density of 'i' antigen observed on red cells
|
CDA II
|
|
|
Patient with episodic hemolysis and thrombosis in large vessels. Sucrose hemolysis test and Ham test are both + (enhanced hemolysis). What will flow cytometry show? What is the etiology?
|
Diminished expression of CD59 and CD55 on leukocytes, platelets, and RBCs.
PNH decreased GPI (glycosyl phosphatidyl inositol) anchors. Initial step in GPI synthesis encoded by PIG-A gene. |
|
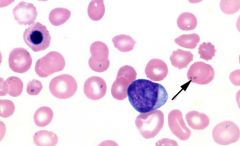
Patient with asplenia or sideroblastic anemia. What is the arrow pointing to?
|
Pappenheimer bodies
Iron-containing autophagosome |
|
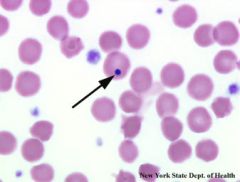
Patient with asplenia. What is the arrow pointing to?
|
Howell-Jolly body
residual nuclear fragment Cabot ring is the same. |
|
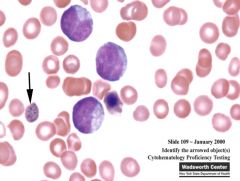
associated with hemolytic anemias, lead poisoning, thalassemias
|
Basophilic stippling
clusters of ribosomes |
|
|
Parvovirus B19 arrests at which stage of erythroid development
|
Pronormoblast
|
|
|
What test is crucial for diagnosing WAIHA?
With what antibody is it most commonly associated? Occurs secondary to? |
DAT + in nearly all cases (IgG only 2/3, IgG/C3 1/4)
IgG anti-Rh (broad activity) Lymphoma (esp CLL/SLL). medications, and inherited autoimmunity (CVID, Bruton's, IgA defic) |
|
|
Complement activated by what antibodies?
|
IgA, IgM, IgG1, IgG3
|
|
|
Cold agglutinin disease associated with what infections and what antibodies?
What are the most important laboratory features in predicting pathogenicity? |
Mycoplasma pneumoniae: IgM anti-I (most common)
infectious mono (EBV): IgM anti-i titer and thermal range |
|
|
What reagent can be used to identify i antigen?
|
Type O cord blood
|
|
|
Paroxsysmal cold hemoglobinuria associated with?
What antibody? |
syphilis, children with viral illnesses (measles, mumps, chickenpox and EBV)
IgG biphasic hemolysin with anti-P specificity (Donath-Landsteiner antibody) |
|
|
How is Donath Landsteiner test done?
|
2 vials of blood, one @ 4 degrees C and one @ 37 degrees C. + test if only incubation of patient's RBCs at 4 then 37 leads to hemolysis.
|
|
|
To detect cryoglobulins ?
|
Clot blood at 37 degrees C and then centrifuge.
Store serum at 4 degrees C for 3 days and then centrifuge. Cryoprecipitate can be used for electrophoresis. |
|
|
Most common type of cryoglobulin?
|
type II monoclonal IgM and polyclonal IgG
|
|
|
Most common cause of mixed cryoglobulinemia?
|
HCV
|
|
|
Clinical syndrome of cryoglobulinemia
|
palpable purpuras (leukocytoclastic vasculitis)
arthralgias hepatosplenomegaly lymphadenopathy anemia sensorineural defects glomerulonephritis |
|
|
Most common finding in the kidney in cryoglobulinemia?
|
MPGN type II or DDD
|
|
|
First indicator of iron deficiency anemia?
|
Ferritin decreases
|
|
|
1 mL of packed RBCs contains how much iron?
|
1 mg
|
|
|
In children increased lead correlates with ?
|
decreased iron.
Lead ingestion inhibits intestinal iron absorption. |
|
|
B12 is bound to intrinsic factor in what part of the GI tract?
IF is derived from what part of the GI tract? |
duodenum
stomach |
|
|
Classic features of megaloblastic anemia?
|
marked oval macrocytosis
hypersegmented neutrophils large platelets |
|
|
The most common cause of anemia in hospitalized patients?
|
anemia of chronic disease
|
|
|
EPO-secreting neoplasms
|
RCC
cerebellar hemangioblastoma uterine leiomyomas hepatocellular carcinoma |
|
|
Sideroblastic anemia most often caused by ?
Distinguished from hereditary hemochromatosis by? Inherited forms gene? May be overcome with? |
clonal stem cell defect
low hemoglobin and low MCV ALAS2 gene on X chromosome, large doses of B6, pyridoxine |
|
|
Acquired pure red cell aplasia caused by?
Congenital pure red cell aplasia? |
thymoma and parvovirus B19
Blackfan-Diamond syndrome |
|
|
i antigen overexpressed on RBCs
Hb F increased. What's the dx? |
Diamond-Blackfan syndrome
|
|
|
AR chromosomal breakage syndrome
café au lait spots, hypo- or hyperpigmentation skeletal anomalies, hypoplastic thumb, absent radii renal anomalies, horseshoe kidney short stature microphthalmia mental retardation What disease? Increased risk for ? |
Fanconi anemia
myelodysplasia and AMLs |
|
|
chromosomal breakage syndromes
|
Xeroderma pigmentosum XP
Ataxia telangiectasia AT Bloom syndrome BS Cockayne syndrome Fanconi anemia |
|
|
Wright stain is made by?
|
methylene blue
eosin alcohol |
|
|
1. stain for lipid material in granulocytes and monocytes?
2. Stain found only in granulocytes, not monocytes and lymphocytes? 3. Monocyte NSE (nonspecific esterase) is inhibited by? |
1. Sudan black B SBB
2. Chloroacetate esterase 3. Sodium fluoride NaF |
|
|
Leukocyte alkaline phosphatase score is decreased in ?
|
CML
PNH some myelodysplastic syndromes congenital hypophosphatasia neonatal septicemia |
|
|
LAP score increased in ?
|
Leukemoid reaction
non-CML myeloproliferative disorders glucocorticoid administration third trimester of pregnancy |
|
|
normal blood and tissue T:B cell ratio?
|
2-6:1
|
|
|
earliest B-cell precursors express?
|
CD34
TdT CD38 dim CD45 CD10 CD19 |
|
|
B-cells that express IgM also express?
|
CD19
CD20 CD22 CD79 CD40 CD38 expressed on activated B-cells |
|
|
Plasma cells express?
|
CD79a
bright CD38 and CD138 CD10 CD13 CD33 |
|
|
early T-cell precursors express?
|
CD34
TdT HLA-DR dim CD45 CD38 CD2 CD7 cyt CD3 |
|
|
surface CD3 expression coincides with expression of what other marker in T-cells?
|
TCR
|
|
|
Mature T-cells express?
activation marker? |
CD 4 or CD8 with CD3 (gamma-delta T cells do not express CD3)
CD38 |
|
|
CD4:CD8 ratio?
|
2:1
|
|
|
gamma-delta T cells found mostly where?
|
spleen, dermis, intestine
|
|
|
NK cells express?
|
CD16 - receptor for the Fc portion of gamma heavy chains
CD56 may express cyt CD3, but not surface CD3 |
|
|
Myeloblasts express?
|
CD34
HLA-DR CD38 CD117 CD13 CD33 |
|
|
Promyelocytes
Metamyelocytes |
CD13, CD33, CD15
acquire CD11b |
|
|
Monocytes
|
CD64
CD14 CD11b CD15 |
|
|
CD4+/CD8+ T cells found where?
Majority of T-cell lymphomas and leukemias are? |
thymic cortex
CD4+ |
|
|
Hairy cell leukemia neoplastic B-cells express?
|
CD11c
CD103 |
|
|
Platelets are counted by electrical impedance at what size range?
|
2-20 fL
|
|
|
What is a fluorochrome?
How are its properties used in FC? |
Substance that absorbs light at one wavelength and emits it at a different wavelength.
Detection of original wavelength determines size and complexity of cell. Emitted wavelength determines antigen expression. |
|
|
Difference between absorbed and emitted wavelength in a fluorochrome in flow cytometry called?
|
Stokes shift
|
|
|
CD45 bright?
CD45 intermediate? CD45 dim or not expressed? |
lymphocytes and monocytes
granulocytes RBCs |
|
|
bcl-1 (cyclin-D1, PRAD-1) expressed by?
|
neoplastic mantle cells
|
|
|
Antigen expresssed in most low-grade B-cell lymphomas, many high-grade B-cell lymphomas and decreasing expression in follicular lymphomas with higher grade?
|
bcl-2
not expressed by Burkitt |
|
|
Antigen associated with Burkitt, follicular, NLPHL, and subset of DLBCL.
expression in DLBCL associated with what translocation? |
bcl-6
t(3;14) IGH-BCL-6 |
|
|
Anaplastic large cell lymphoma unique expression of?
|
Clusterin in a discrete golgi pattern
|
|
|
CD20 expression by CLL/SLL is bright or dim?
What antibody recognizes a particular conformation of CD20? Which cells tend to be + for this antibody? |
Dim
FMC-7, CD20 bright are usually + |
|
|
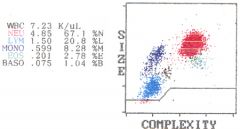
Eosinophils more complex than neutrophils?
|
|
|
Reactive neutrophilia often accompanied by ?
|
toxic granulation
Dohle bodies cytoplasmic vacuoles left shift consisting of bands and some metamyelocytes (NO blasts!) |
|
|
Reactive neutrophilia in which toxic changes are absent seen in what syndrome? What is the only dependable finding?
|
Hantavirus pulmonary syndrome
thrombocytopenia |
|
Young female adult, smoker with absolute increase in lymphocytes. Polyclonal IgM hypergammaglobulinemia. What likely HLA type is most likely?
|
HLA-DR7
Persistent polyclonal B lymphocytosis |
|
|
Which cytokine is most specific for eosinophil lineage and responsible for selective differentiation of eosinophils and release of eosinophils from bone marrow?
|
IL-5
|
|
|
triad of rheumatoid arthritis, splenomegaly, and neutropenia?
|
Felty syndrome
|
|
|
Asian man with soft tissue mass of the head with cervical lymphadenopathy, peripheral blood with eosinophilia and increased IgE.
|
Kimura disease
|
|
Patient with bilateral cervical lymphadenopathy and above cell found on biopsy.
Dx? Histiocytes express? |
Rosai-Dorfman
S100, CD11b, CD14, lysozyme, HLA-DR, and unexpectedly CD31 |
|
Male patient with diarrhea, arthralgias, and hepatospenomegaly. GI bx above. PAS w/ diastase.
What organism and dx? |
Tropheryma whippelii
Whipple disease |
|
Histiocytes with karyorrhectic debris and no neutrophils. Young Japanese woman with unilateral cervical LAD and fever.
|
Kikuchi-Fujimoto disease
|
|
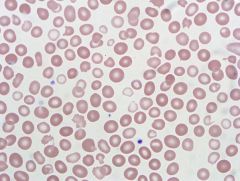
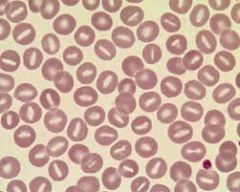
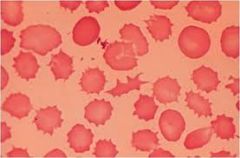
The blood smear pictured shows a dimorphic red cell population. This can be seen in
A) myelodysplastic syndrome (MDS). B) oxidative hemolysis. C) hereditary spherocytosis (HS). D) hereditary elliptocytosis (HE). E) thrombotic thrombocytopenic purpura (TTP). |
A) Dimorphism is seen in red blood cells in sideroblastic anemia, transfusion, and sometimes in MDS. Oxidative hemolysis results in bite cells. Thrombotic thrombocytopenic purpura (TTP) shows schistocytes. HS and HE show spherocytes and elliptocytes, respectively
|
|
|
An 76-year-old man is being evaluated for fever, weight loss, and a WBC count of 36,900/µL (Reference range: 4,000-10,000/µL), with 60% granulocytes and 12% unclassified cells. Peripheral blood flow cytometry demonstrates a 20% population of cells that are CD10(bright +), CD19(+), CD20(partial +), CD22(+), CD33(+), CD34(+), CD38(+), CD45(dim +), CD79a(+), CD117(-), Tdt(+), and MPO(-). Fluorescence in situ hybridization shows a BCR-ABL1 translocation in 73% of cells. What is the most likely diagnosis?
A) Chronic myelogenous leukemia, chronic phase B) Chronic myelogenous leukemia, blast phase C) Chronic myelomonocytic leukemia D) Chronic neutrophilic leukemia E) Acute myeloid leukemia |
Flow cytometry is positive for a population (20%) of B-lymphoblasts, and cytogenetics shows the presence of a Philadelphia chromosome in a higher proportion of cells (73%). These findings are indicative of a blast phase of chronic myelogenous leukemia (CML), which is defined as 20% of greater blasts in the peripheral blood or bone marrow. Chronic phase CML does not usually show more than 2% myeloblasts in the peripheral blood.
|
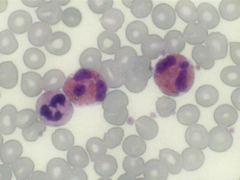
|
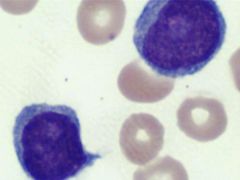
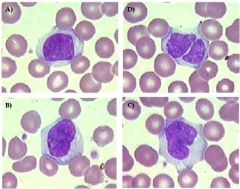
An 88-year-old man presents to the emergency room with a WBC of 110,000 (Reference Range: 4,000-10,000) and extreme fatigue. The emergency room physician asks you to review the peripheral blood smear where you see the following cells, comprising up to 75% of the leukocytes. Which of the following is true about this entity?
A) >20% of total leukocytes is defining B) > 55% of total leukocytes is defining C) > 20% of total lymphoid cells is defining D) > 55% of total lymphoid cells is defining E) No percentage has been defined |
D) B-cell prolymphocytic leukemia (B-PLL) occurs usually de novo (although some can transform from chronic lymphocytic leukemia). It is characterized by rapidly rising white blood cell count and minimal peripheral LAD. Seen here are prolymphocytes and when they number >55% of lymphoid cells, a diagnosis of B-PLL is favored.
|
|
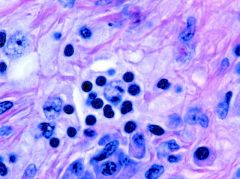
A) histoplasmosis.
B) coccidiomycosis. C) Cryptococcus. D) leishmaniasis. E) Candida. |
C) The fungal organism present is consistent w/ cryptococcus in a pt with disseminated disease (cryptococcosis). A mucicarmine stain could be used to highlight the mucopolysaccharide capsule (you can see a space around the organisms). Masson-Fontana stain would result in a melanin-like pigment.
|
|
|
Patients with transient abnormal myelopoiesis have
A) trisomy 18. B) trisomy 21. C) trisomy 8. D) deletion 5q. E) deletion 20q. |
Transient abnormal myelopoiesis is a condition seen exclusively in patients with Down's syndrome (trisomy 21) or rarely in patients with trisomy 21 mosaicism. It presents with increased blasts in the peripheral blood and bone marrow which resolve spontaneously over time.
|
|
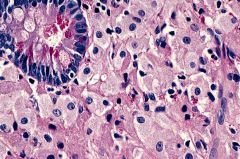
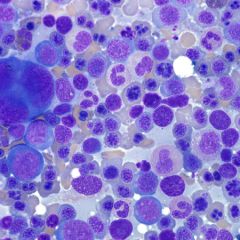
A 78-year-old man presents with a lumbar fracture after a traumatic fall. Bone scan shows multiple lytic lesions. A bone marrow biopsy showed the following (see figure). Given the choices, what would be the most reasonable next step to further classify this disease state?
A) Flow cytometry on the aspirate is needed. B) Cytochemical staining would help classify the lesion. C) Pursue a non-hematopoietic neoplasm workup. D) Special stains for fungal organisms are required. E) FISH and/or PCR studies may be diagnostic. |
C) Pursue a non-hematopoietic neoplasm workup.
|
|
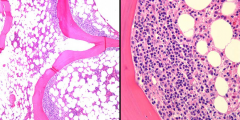
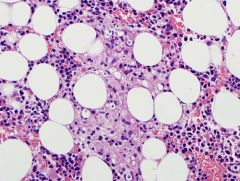
An 82-year-old man is diagnosed with diffuse large B-cell lymphoma (DLBCL) of the lung, and representative images from a staging bone marrow biopsy are shown. Which one of the following statements is correct regarding this histological pattern of bone marrow involvement?
A) It has a better prognosis than concordant involvement. B) It is more common than concordant involvement. C) It has a different immunophenotype than concordant involvement. D) Its involvement has a different gene expression profile than concordant involvement. E) It has different chromosomal abnormalities than concordant involvement |
B) It is more common than concordant involvement.
|
|
|
A bone marrow biopsy performed on a 45-year-old patient shows a myeloid neoplasm that does not harbor a BCR-ABL1 translocation. Of the choices, which diagnosis requires an absence of a BCR-ABL1 translocation?
A) Acute myeloid leukemia B) B-lymphoblastic leukemia / lymphoma C) Chronic myelogenous leukemia, chronic phase D) Atypical chronic myeloid leukemia E) Chronic myelogenous leukemia, blast phase |
By definition, atypical chronic myeloid leukemia is a myelodysplastic / myeloproliferative neoplasm that lacks a Philadelphia chromosome. A BCR-ABL1 translocation is seen in chronic myelogenous leukemia, both chronic phase or blast phase, and may be found in acute myeloid leukemia or B-lymphoblastic leukemia.
|
|
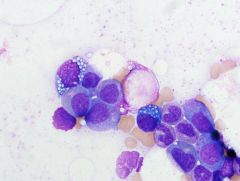
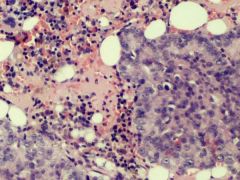
In patients with the finding pictured, it is important to exclude
A) B12 deficiency. B) thiamine deficiency. C) folate deficiency. D) zinc deficiency. E) copper deficiency. |
Vacuolated erythroid precursors and cytopenias can be seen in patients with copper deficiency. Copper deficiency can be secondary to zinc overload (zinc lozenges, denture cream ingestion). B12 and folate typically show megaloblastoid change and hyperlobulated neutrophils.
|
|
|
Congenital dyserythropoietic anemias (CDA) are inherited red cell disorders, characterized by ineffective erythropoiesis. Frequently a distinguishing morphologic feature is multinucleated erythroblasts, amount of which helps define the most common types of I, II, and III. For CDA type II, what other feature is typically seen?
A) Negative Ham test B) Positive sucrose hemolysis test C) Peripheral double membranes by electron microscopy D) No reaction with anti-i E) Massive giant multinucleated erythroblasts |
The double membrane appearance is actually excessive endoplasmic reticulum running parallel to the cell membrane, imparting a double membrane look. The other choices are opposite, while choice E is usually seen with type III.
|
|
|
Polycythemia vera (PV) is a chronic myeloproliferative neoplasm, diagnosed by criteria established by the WHO 2008. Of the major criteria, JAK2 V617F mutation or other functionally similar mutation must be demonstrated. A certain type of PV with isolated erythrocytosis versus the usual panmyelosis of the JAK2 V617F type may be seen with what mutation type?
A) JAK2 exon 14 B) JAK2 exon 13 C) JAK2 exon 12 D) JAK2 exon 11 E) JAK2 exon 10 |
JAK2 exon 12 mutation has been described to be associated with primarily erythrocytosis-type PV. If PV is strong in the differential and JAK2 V617F is negative, follow up with additional exon 12 testing may be prudent, especially if this morphology is seen. Of note, V617F is on exon 14.
|
|
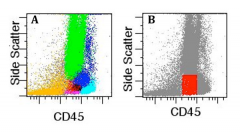
Incorrect Ungraded 17.
The figure shows various cell populations identified in a bone marrow specimen by clusters analysis (panel A) and the boundaries of a traditional CD45/side scatter "blast gate" (panel B, in red). In myeloproliferative neoplasms, myeloblasts comprise approximately what percentage of total events within the traditional CD45/SSC "blast gate"? A) 20% B) 40% C) 60% D) 80% E) 100% |
The traditional CD45/SSC “blast gate” has a heterogeneous composition, and includes granulocytes, monocytes, lymphocytes, erythroid precursors, hematogones, and basophils, in addition to myeloblasts. As a consequence, blasts represent only about 20% of the events contained within the “blast gate”.
|
|
A 67-year-old woman presents with a WBC of 40,000 x 103/µL where over half the cells are of the following depicted here. Duodenal biopsies and a removed gallbladder all show similar cells infiltrating throughout. Before you can make a diagnosis, which statement is correct in regards to the criteria established by the WHO 2008?
A) Idiopathic hypereosinophilic syndrome (HES) has evidence of tissue injury, whereas reactive eosinophilia does not. B) Chronic eosinophilic leukemia, not other specified (CEL, NOS) can be diagnosed regardless of BCR/ABL mutational status. C) CEL, NOS can be diagnosed regardless of JAK2 mutational status. D) CEL, NOS is separated from idiopathic HES by duration of symptoms. E) Idiopathic HES and CEL, NOS are synonyms for the same entity. |
A) According to the WHO 2008 classification, idiopathic HES includes organ injury as well as a thorough rule out of other possible MPS, MDS, or leukemic causes, including mastocytosis. CEL, NOS has overlapping morphologic & lab features w/ idiopathic HES but, in contrast to the latter, there is evidence of eosinophil clonality. In the context of myeloproliferative neoplasms with eosinophilia, it is important to rule out those with specific cytogenetic abnormalities, including PDGFRA, PDGFRB or FGFR1, since this has prx & tx implications.
|
|
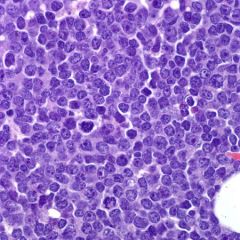
79-year-old man is being evaluated for extensive lymphadenopathy and an elevated WBC count of 100,804/µL (Reference Range: 4,000-10,000/µL), with 79% atypical cells. A representative image of the bone marrow core biopsy is shown. Flow cytometry shows a predominant population of large cells that are CD19(+), CD20(variably +), CD22(dim +), CD5(-), CD10(+), Tdt(-), and surface lambda light chain restricted. Immunohistochemistry is positive for BCL-2, BCL-6, and a MIB-1 proliferation rate of 90%. Cytogenetic analysis shows rearrangements of the BCL-2, BCL-6, and MYC genes. What is the most likely diagnosis?
|
"Triple hit" lymphoma
This patient has a B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma. This is a category of aggressive lymphomas that have morphologic and genetic features of both diffuse large B-cell lymphoma (DLBCL) and Burkitt lymphoma (BL). A subset of these cases show MYC and BCL-2, or MYC and BCL-6 gene rearrangements, and are known as "Double hit" lymphoma. A minority of cases demonstrates rearrangements of all three genes (MYC, BCL-2, and BCL-6) and thereby constitutes "triple hit" lymphomas. |
|
|
Which of the following is true regarding myelodysplastic syndrome (MDS) w/ isolated del 5q?
A) It may have increased blasts, but always fewer than 5% in the bone marrow. B) It may be JAK2 V617F positive. C) It is aggressive with poor long-term survival. D) It often has a complex karyotype. E) Typically has a low platelet count. |
B) It is important to know that it may be JAK2 V617F positive in case this causes confusion with early primary myelofibrosis or essential thrombocythemia. It is a more indolent form of MDS typically.
|
|
A 29-year-old man with history of acute promyelocytic leukemia has a bone marrow biopsy performed for pancytopenia, 45 days after induction chemotherapy; he is currently on maintenance chemotherapy with arsenic trioxide and idarubicin. A representative image of the bone marrow aspirate is shown. What is the most likely diagnosis?
A) Persistent acute promyelocytic leukemia B) Therapy-related myelodysplastic syndrome C) Chemotherapy effect D) Megaloblastic anemia E) Parvovirus B19 infection |
C) This patient has erythroid hyperplasia with prominent dyserythropoiesis, secondary to arsenic trioxide. This morphology mimics dysplasia that can be seen in a myelodysplastic syndrome (MDS), although the time frame for a therapy-related MDS would be too short for this patient
|
|
|
Hepcidin is a hormone that acts to regulate iron metabolism. One site of action is to inhibit iron release from stores in macrophages to be utilized by red blood cells. Of the choices, which disease state is most closely associated with elevated hepcidin levels?
A) Megaloblastic anemia B) Fanconi anemia C) Chronic disease anemia D) Iron deficiency anemia E) Sickle cell anemia |
C) Chronic disease anemia
In anemia of chronic disease, the storage iron in macrophages is relatively increased as compared to sideroblasts. This reflects how hepcidin in macrophages is elevated and inhibits release of iron from macrophages to be transported and incorporated by red blood cells. |
|
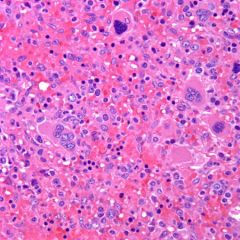
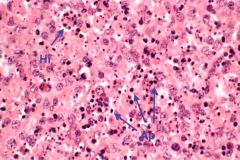
An 82-year-old woman has a splenectomy performed for splenomegaly (3,000 g spleen weight). A representative microphotograph is shown. What is the most likely diagnosis made in a bone marrow biopsy performed concomitantly?
A) Hepatosplenic T-cell lymphoma B) Chronic lymphocytic leukemia C) Primary myelofibrosis D) Hairy cell leukemia E) Splenic marginal zone lymphoma |
C) primary myelofibrosis
The patient has massive splenomegaly with extramedullary hematopoiesis (EMH), secondary to primary myelofibrosis. The splenic red pulp shows maturing myelomonocytic and erythroid precursors, and atypical megakaryocytes. |

