![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
26 Cards in this Set
- Front
- Back
|
Increased risks w/ a lack of prenatal care?
|
Inc. risk of low birth weight.
Inc risk of preterm delivery Inc risk of maternal infant mortality |
|
|
Trimesters of pregnancy
|
1st - Week 1 - 13
2nd - Week 14 - 27 3rd - Week 28 -40 |
|
|
Nagele's Rule
Formula |
assumes 28 day cycle
used to determine EDD EDD = [(LMP + 7 days) - 3 months] + 1 yr |
|
|
Initial Assessment - Physical Exam should include
|
- VS
- Height and weight - Examination of mouth, teeth, and gums - Palpation of thyroid - Auscultation of maternal heart sounds - Inspection and palpation of breasts - Inspection and palpation of abdomen - Inspection of extremities - Measurement of fundal height -Auscultation of FHT - Pelvic exam -BP - will be a baseline measurement, 30/15 increase during pregnancy, should always be taken w/ patient in same position for each visit. |
|
|
Antibody titer screen - Rh
- A problem if ___mother + ___ fetus. - How does it happen? - Fetus at risk for: -routing laboratory test done at |
Rh- mother + Rh+ fetus
Mother's body reacts to the blood of the fetus as a foreign protein produces IgG & IgM. IgG crosses placenta, antibodies bind to fetal RBCs -> cell lysis -> fetal anemia. Fetus at risk for erythroblastosis fetalis or hyperbilirubinemia. - Routine IM injection at 28wks (or after exposure risk (bleeding during preg, truma, delivery, amnio, CVS) - Rogan |
|
|
Laboratory tests
Hemoglobin normal values: Hematocrit normal values: |
Hgb > 10.5g/100ml
Hct > 32-34% used to detect anemia or infection |
|
|
Other laboratory tests done
|
PPD
Rubella screening STI screening - syphillis, GC, chlamydia, HIV PAP Smear HbsAg Sickle cell- + result -> further testing for SC trait or disease Urine analysis - C&S |
|
|
Laboratory tests
DMS done at: |
24-28 wks
blood sample drawn 1hr after 50g glucose drink. levels are taken 2 and 3 hrs after. If all are high mother is considered to have GDM. |
|
|
Ultrasound
Routine at ___ wks. Used to see: |
16-20 wks.
congenital malformation fetal measurement vs. EGA placental location fetal # amniotic fluid volume |
|
|
Gentetic testing
Amniocentesis done at __ wks. Rec for women: Rate of miscarriage |
16-18wks
Women at risk for fetal abnormalities. 35yo and above Family history US abnormality 1 in 200-400 procedures |
|
|
Genetic testing
CVS - Chorionic Villi Sampling done at: Miscarriage risk |
10-13 wks
Misc. risk 1-2% Becoming more common then amnio. Advantage is earlier detection - 1st tirmester |
|
|
Ongoing Assessments for prenatal visits
|
- Weight - watching for TRENDS
- VS - Urine - protein, glucose - looking for UTIs - Abdominal palpation - tenderness (would indicate possible uterine infection), Leopold maneuvers |
|
|
Leopold Maneuvers
|
reveals presenting part of the fetus, can also be used to estim. fetal weight
(dont have to memorize) #1 What is in the fundus? Head or breech? #2 Where is the back #3 What is the presenting part? #4 Where is the cephalic prominence? |
|
|
Fundal Height
McDonalds measurement |
measurement of the height of the uterus above the symphysis pubis. Provides a gross estimate of the duration of pregnancy
done after 20wks gestation, measured in cm, app the wks in pregnancy. watch for trending, # of wks should = # of cm |
|
|
Fetal heart tones
Auscultation done with ___ at 10-12wks ___ at 18-20wks |
doppler 10-12
fetascope 18-20 Difficult in: obese women, back of fetus is facing the womens back, hydraminos (lg amt of amniotic fluid), fetal movement |
|
|
Anticipated schedule of prenatal visits
|
Initial visit w/ in 1st 4-8wks.
q 4wks until 28wks q 2wks until 36 q wk until delivery |
|
|
Initial Prenatal education
|
- S&S to report to HCP - any concerns, bleeding
- Practices to promote health maintenance. - seat belt use, lap belt worn low across pelvic bones, shoulder harness above uterus, below neck. -substance use - childbirth education |
|
|
3rd Trimester Education classes
|
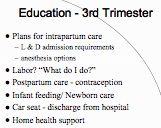
3rd Trimester Education
|
|
|
3rd Trimester Education
Birth Plan |
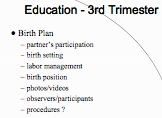
Birth plan
|
|
|
Antepartum fetal surveillance
|

Antepartum fetal surveillance
|
|
|
When to phone health care provider?
|
- Frequent, regular, painful uterine contractions x 1 hour
- ROM - gush or trickle of clear, watery fluid from vagina - Bloody show - Vaginal bleeding - Decreased or absent fetal movement |
|
|
Non-stress Test (NST)
|
Antepartum fetal surveillance
Observed fetal heart rate accelerations associated w/ fetal movement -reactive = 2FH accelerations in 20min -nonreactive |
|
|
Contraction stress test (CST)
2 methods Adequate UC: Interpretation of CST |
observed fetal heart response to uterine contractions.
1) nipple stimulated 2) oxytocin stimulated If no late decels the test is negative, if positive further testing is done. *Good contractions: UC lasting 40-60sec w/in 10min pd. |
|
|
Biophysical profile (BPP)
|
non invasive assessment of the fetus and its environment using ultrasonography and fetal monitoring; includes fetal breathing movements, gross body movements,
fetal tone, reactive fetal heart rate, and qualitative amniotic fluid volume. |
|
|
Amniotic fluid volume
increases until ___wks volume decreases by ____% per week after ___wks |
inc until 33wks
volume dec 10-15% per wk until 40wks extremes of inc or dec are related to poor perinatal outcomes. |
|
|
Fetal kick counts
|
# of fetal movements not defined or minutes for testing. Recommended 60min or 1-3 times per day. Mother counts fetal movements.
Concern is if no movements in 12hr period. A count of fewer then 3 in 1hr warrents further evaluation. |

