![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
127 Cards in this Set
- Front
- Back
|
Presbyopia |
Impaired near vision, found in middle-aged and older people
Often sees better when the card (simulated Snellen chart) is farther away |
|
|
US Legally Blind |
Vision in the better eye, with glasses, is 20/200 or less
Constricted field of vision: 20 degrees or less in the better eye |
|
|
Myopia |
Impaired far vision |
|
|
Vision of 20/200 |
At 20 feet the patient can read print that a person with normal vision could read at 200 feet
Larger the second number the worse the vision |
|
|
Static Finger Wiggle and Kinetic Red Target Tests |
Sensitivity and specificity of the two tests compared to automated perimetry is 78% and 90%
Diagnostic practice improves with higher density and severity of field defects, irrespective of diagnosis |
|
|
Causes of anterior pathway defects |
Glaucoma, optic neuropathy, optic neuritis, glioma |
|
|
Causes of posterior pathways defects |
Stroke and chiasmal tumors |
|
|
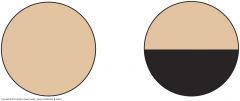
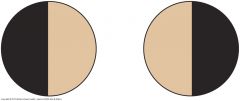
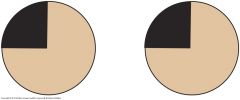
Left homonymous hemianopsia |

When the patients left eye repeatedly does not see you fingers until they have crossed the line of gaze a left temporal hemianopsia is present and then a left homonymous hemianopsia can be established; if only in one eye then the other eye is a nasal defect
Picture (left and right)
|
|
|
Enlarged blind spot |
Conditions affecting the optic nerve: 1) Glaucoma 2) Optic neuritis 3) Papilledema |
|
|
Scaliness of eyebrows |
Seborrheic dermatitis |
|
|
Lateral sparseness of eyebrows |
Hypothyroidism |
|
|
Upstarting of palpebral fissures |
Down syndrome |
|
|
Blepharitis |
Red inflamed lid margins, often with crusting |
|
|
Poor eye convergence |
Hyperthyroidism
Normal eye can follow the object within 5cm to 8cm of the nose |
|
|
Contraindications for mydriatic drops (dilate) |
1) Head injury and coma, in which continuing observations of pupillary reactions are essential 2) Suspicion of narrow-angle glaucoma
|
|
|
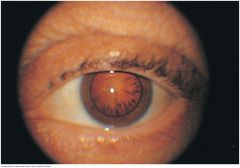
Absence of red reflex |
1) Opacity of the lens (cataract) or vitreous
Less commonly: 1) Detached retina 2) In children, rentinoblastoma
Artificial eye |
|
|
Lens surgically removed |
Magnifying effect is lost
Retinal structures look smaller and you can see much larger expanse of the fundus |
|
|
How light rays shine on retina |
Refractive error - light rays from a distance do not focus on retina
Myopia - light rays focus anterior to the retina; retinal structures look larger than normal
Hyperopia - light rays focus posterior to the retina |
|
|
Enlarged physiologic cup |
Chronic open-angle glaucoma |
|
|
Loss of spontaneous venous pulsations |
High intracranial pressures (above 190 mm H2O) that change the pressure gradient between cerebral spinal fluid pressure and intraocular pulse pressure in the optic disc |
|
|
Cotton Wool Patches |
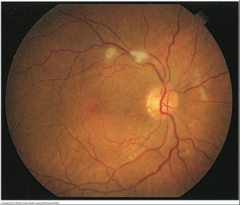
Irregular white patches
|
|
|
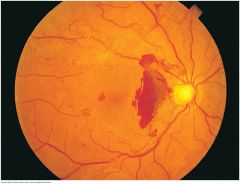
Macular degeneration |
Important cause of poor central vision in older adults
1) Dry atrophic 2) Wet exudative (neovascular) |
|
|
Drusen |
Undigested cellular debris
May be hard and sharply defined (picture) or soft and confluent with altered pigmentation
|
|
|
Vitreous floaters |
Dark specks or strands between the fundus and the lens |
|
|
Acute otitis externa |
Ear canal is swollen, narrowed, moist, pale, and tender; may also be reddened |
|
|
Chronic otitis externa |
Skin of ear canal is thickened, red and itchy
Decreased eardrum mobility |
|
|
Acute purulent otitis media |
Red, bulging eardrum
Decreased eardrum mobility |
|
|
Retracted ear drum |
Unusually prominent short process of malleus and a prominent handle that looks more horizontal |
|
|
"Do you feel you have a hearing loss or difficulty hearing?" |
If "yes", twice as likely to have a hearing deficit
If "no", the likelihood of moderate to severe hearing impairment if only 0.13 |
|
|
Whispered voice test |
Detects significant hearing loss of greater than 30 decibels Sensitivity - 90% to 100% Specificity - 70% to 87% |
|
|
Presbycusis |
Older adult hearing loss
Higher frequency hearing loss; cannot hear consonants |
|
|
Tuning fork tests |
Do not distinguish normal hearing from bilateral neurosensory loss or from mixed conductive and neurosensory loss
Weber Test: Sensitivity - 55% Specificity for neurosensory loss - 79% Specificity for conductive loss - 92%
Rinne Test: Sensitivity - 60% to 90% Specificity - 95% to 98% |
|
|
Unilateral conductive hearing loss |
Sound is heard in (lateralized to) the impaired ear with Weber test
Explanations: 1) Otoclerosis otitis media 2) Perforation of the eardrum 3) Cerumen |
|
|
Local infection of nose (Furuncle) |
Tenderness of the nasal top or alae |
|
|
Viral rhinitis |
Mucosa is reddened and swollen |
|
|
Allergic rhinitis |
Mucosa is pale, bluish, or red |
|
|
Causes of septal perforation |
1) Trauma 2) Surgery 3) Intranasal use of cocaine or amphetamines (also cause ulceration) |
|
|
Nasal polyps |
Pale saclike growths of inflamed tissue that can obstruct the air passage or sinuses
Conditions with nasal polyps: 1) Allergic rhinitis 2) Aspirin sensitivity 3) Asthma 4) Chronic sinus infections 5) Cystic fibrosis |
|
|
Acute sinusitis involving the frontal or maxillary sinuses |
Local tenderness of nose
Pain, fever, and nasal discharge
Transillumination can show that light cannot travel through sinuses; due to thickened mucosa or secretions or developmental absence of one or both sinuses |
|
|
Enlargement of supraclavicular node |
Suggests a possible metastasis from a thoracic or an abdominal malignancy, especially on the left side
Nodes described in two dimensions, maximal length and width (1 cm x 2 cm) |
|
|
Tender nodes |
Inflammation |
|
|
Hard or fixed nodes |
Malignancy |
|
|
Generalized lymphadenopathy |
Lymph nodes which are abnormal in size, number or consistency and is often used as a synonym for swollen or enlarged lymph nodes
Seen in:
1) HIV or AIDS 2) Infectious mononucleosis 3) Lymphoma 4) Leukemia 5) Sarcoidosis |
|
|
Tracheal deviation |
Masses in the neck can push the trachea to the side
Signify problems in the thorax: 1) Mediastinal mass 2) Atelectasis 3) Large pneumothorax |
|
|
Goiter |
Enlargement of the thyroid gland to twice its normal size
May be simple, without nodules, or multinodular, are are usually euthyroid (state of having normal thyroid gland function)
With swallowing, the lower border of this large gland rises and looks less symmetric |
|
|
Retrosternal goiters |
Below the suprasternal notch
Cause hoarseness, shortness of breath, stridor, or dysphagia from tracheal compression
Neck hyperextension and arm elevation may cause flushing from dilation of the external jugular veins and obstruction of the thoracic inlet
Usually present in the 5th decade; over 85% are benign |
|
|
Assessment of thyroid gland |
Physical: size, shape and consistancy
Function mostly depends on symptoms and signs elsewhere in the body, and on lab tests |
|
|
Lobes of the thyroid gland |
Graves' disease: soft Hashimoto's thyroiditis & Malignancy: firm Thyroiditis: tender |
|
|
Exophthalmos |
Eyes that look unusually prominent
Graves' disease from autoimmune hyperthyroidism: 50% of patients Graves' ophthalmopathy: 60% of patients Common symptoms 1) Diplopia 2) Tearing, grittiness, and pain from corneal exposure 3) Eyelid retraction 4) Extraocular muscle dysfunction 5) Ocular pain 6) Lacrimation |
|
|
Obstructed nasolacrimal duct |
Discharge of mucopurulent fluid from the puncta (small hole where tears from lacrimal glands are collected) |
|
|
Left-sided optic nerve damage
Marcus Gunn pupil |
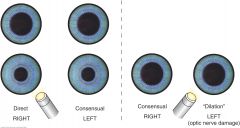
1) Light beam shines into the normal right eye; Brisk constriction of both pupils (direct response on the right and consensual response on the left) 2) Light beam swings over to the abnormal left eye; Partial dilation of both pupils occur a. Afferent stimulus on the left is reduced so the efferent signals to both pupils are also reduced and a net dilation occurs
Marcus Gunn pupil, most common pupillary abnormality; afferent pupillary defect |
|
|
Primary Headaches: Migraines |
Process: Neuronal dysfunction, possibly of brainstem origin, involving low serotonin, spreading cortical depression and trigemino-vascular activation. Types: w/ aura, w/o aura, variants
Location: Unilateral ~70%, Bifrontal or Global ~30%
Quality and Severity: Throbbing or aching, variable in severity
Timing: Onset: Fairly rapid, reaching a peak in 1-2 hours Duration: 1-2 hours Course: Peak incidence early to mid-adolescence; Men ~6%, Women ~15%; Recurrent - usually monthly, but weekly in ~10%
Associated Factors: N/V, photophobia, phonophobia, aura in 30%, either visual (flickering, zig-zagging lines), motor (parethesias of hand, arm, or face, or language dysfunction)
Factors that Aggravate or Provoke: Alcohol, certain foods, or stress may provoke; also menses, high altitude; aggravated by noise and bright light
Factors that Relieve: Quiet, dark room; sleep; sometimes transient relief from pressure on the involved artery
Highly likely if 3 of the 5 "POUND" features are present: Pulsatile or throbbing One-day duration, or lasts 4 to 72 hours if untreated Unilateral Nausea or vomiting Disabling or intensity causing interruption of daily activity |
|
|
Primary Headaches: Tension |
Process: Unclear - possibly heightened CNS pain sensitivity. Involves pericranial muscle tenderness. Etiology also unclear
Location: Usually bilateral; may be generalized or localized to the back of the head and upper neck or to the frontotemporal area
Quality and Severity: Steady; pressing or tightening; nonthrobbing. Mild to moderate intensity
Timing: Onset: Gradual Duration: 30 minutes to 7 days Course: Episodic; may be chronic; Annual prevalence ~40%
Associated Factors: Sometimes photophobia, phonophobia; nausea absent
Factors that Aggravate or Provoke: Sustained muscle tension, as in driving or typing
Factors that Relieve: Possibly massage, relaxation |
|
|
Primary Headaches: Cluster |
Process: Unclear - possibly hypothalmic then trigemino-autonomic activation
Location: Unilateral, usually behind or around the eye or temple
Quality and Severity: Deep, continuous, severe
Timing: Onset: Abrupt; peaks w/i minutes Duration: Up to 3 hours Course: Episodic, clustered in time, with several each day for 4-8 weeks and then relief for 6-12 months; prevalence <1%, more common in men
Associated Factors: Autonomic symptoms: lacrimation, rhinorrhea, miosis, ptosis, eyelid edema, conjunctival infection
Factors that Aggravate or Provoke: During attack, sensitivity to alcohol may increase |
|
|
Secondary Headaches: Analgesic Rebound |
Process: Withdrawal of medication
Location: Previous headache pattern
Quality & Severity: Variable
Timing: Onset: Variable Duration: Depends on prior headache pattern Course: Depends in frequency of "mini withdrawals"
Associated Factors: Depends on prior headache pattern
Factors that Aggravate or Provoke: Fever, carbon monoxide, hypoxia, withdrawal of caffeine, other headache triggers
Factors that Relieve: Depends on cause |
|
|
Secondary Headaches: Headaches from Eye Disorders Errors of Refraction (farsightedness and astigmatism, but not nearsightedness) |
Process: Probably the sustained contraction of extraocular muscles, and possibly of the frontal, temporal and occipital muscles
Location: Around and over the eyes; may radiate to the occipital area
Quality & Severity: Steady, aching, dull
Timing: Onset: Variable Duration: Variable Course: Variable
Associated Factors: Eye fatigue, "sandy" sensations in the eyes, redness of the conjunctiva
Factors that Aggravate or Provoke: Prolonged use of the eyes, particularly for close work
Factors that Relieve: Rest of the eyes |
|
|
Secondary Headaches: Headaches from Eye Disorders Acute Glaucoma |
Process: Sudden increase in intraocular pressure
Location: In and around eye
Quality & Severity: Steady, aching, often severe
Timing: Onset: Often rapid Duration: Variable, may depend on treatment Course: Variable, may depend on treatment
Associated Factors: Diminished vision, sometimes N/V
Factors that Aggravate or Provoke: Sometimes provoked by drops that dilate the pupils |
|
|
Secondary Headaches: Headache from Sinusitis |
Process: Mucosal inflammation of the paranasal sinuses
Location: Usually above the eye (frontal sinuses) or over the maxillary sinus
Quality & Severity: Aching or throbbing, variable in severity; consider possible migraine
Timing: Onset: Variable Duration: Often several hours at a time; recurring Course: Often recurrent in repetitive daily patter
Associated Factors: Local tenderness, nasal congestion, discharge
Factors that Aggravate or Provoke: Coughing, sneezing, or harring the head
Factors that Relieve: Nasal decongestants, antibiotics |
|
|
Secondary Headaches: Meningitis |
Process: Infection of the meninges surrounding the brain and spinal cord
Location: Generalized
Quality & Severity: Stead or throbbing, very severe
Timing: Onset: Fairly rapid, usually less then 24 hours Duration: Variable, usually days Course: A persistent headache in an acute illness
Associated Factors: Fever, stiff neck, change in mental status
Factors that Relieve: Immediate antibiotics until determined if bacterial or viral |
|
|
Secondary Headaches: Subarachnoid Hemorrhage |
Process: Bleeding, most often from a ruptured intracranial aneurysm
Location: Generalized
Quality & Severity: Very severe, "the worst of my life"
Timing: Onset: Usually abrupt, severe with prodromal symptoms Duration: Variable, usually days Course: A persistent headache in an acute illness
Associated Factors: N/V, possibly loss of consciousness, neck pain
Factors that Relieve: Subspecialty treatments |
|
|
Secondary Headaches: Brain Tumor |
Process: Displacement of or traction on pain sensitive arteries and veins or pressures on nerves
Location: Varies with the location of the tumor
Quality & Severity: Aching, steady, variable in intensity
Timing: Onset: Variable Duration: Often brief Course: Often intermittent but progressive
Factors that Aggravate or Provoke: May be aggravated by coughing, sneezing, or sudden movements of the head
Factors that Relieve: Subspecialty treatments |
|
|
Secondary Headaches: Giant Cell (Temporal) Arteritis |
Process: Vasculitis from cell-mediated immune response to elastic lamina of artery
Location: Localized near the involved artery, most often the temporal, but also the occipital; age related
Quality & Severity: Throbbing, generalized, persistent; often severe
Timing: Onset: Gradual or rapid Duration: Variable Course: Recurrent or persistent over weeks to months
Associated Factors: Tenderness of the adjacent scalp; fever, fatigue, weight loss; new headache, jaw claudication, visual loss or blindness, polymyalgia rheumatica
Factors that Aggravate or Provoke: Movement of the neck |
|
|
Secondary Headaches: Postconcussion Headache |
Process: Follows acceleration-deceleration traumatic brain injury
Location: May be localized to the injured area, but not necessarily
Quality & Severity: Generalized, dull, aching, constant; may have features of tension and migraine headaches
Timing: Onset: W/i 7 days of the injury up to 3 months Duration: Weeks, months, or even years Associated Factors: Poor concentration, problems with memory, vertigo, irritability, restlessness, fatigue
Factors that Aggravate or Provoke: Mental and physical exertion, straining, stooping, emotional excitement, alcohol
Factors that Relieve: Rest, medication |
|
|
Cranial Neuralgias: Trigeminal Neuralgia (CNV) |
Process: Compression of the CN V, often by aberrant loop of artery or vein, usually near entry to pons
Location: Cheek, jaws, or gums; trigeminal nerve divisions 2 and 3 > 1
Quality & Severity: Shocklike, stabbing, bruning; severe
Timing: Onset: Abrupt, paroxysmal Duration: Each jab lasts seconds but recurs at intervals of seconds or minutes Course: May last for months, then disappear for months, often recurs. It is uncommon at night
Associated Factors: Exhaustion from recurrent pain
Factors that Aggravate or Provoke: Touching certain areas of the lower face or mouth; chewing, talking, brushing teeth
Factors that Relieve: Medication; Neurovascular decompression |
|
|
Facial Swelling: Cushing's Syndrome |
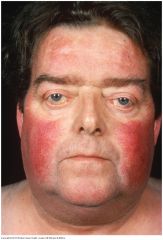
The increased adrenal cortisol production of Cushing's syndrome produces a round or "moon" face with red cheeks. Excessive hair growth may be present in the mustache and sideburn area and on the chin
|
|
|
Facial Swelling: Nephrotic Syndrome |
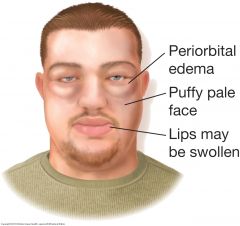
The face is edematous and often pale. Swelling usually appears first around the eyes and in the morning. The eyes may become slitlike when edema is severe
|
|
|
Facial Swelling: Myxedema |
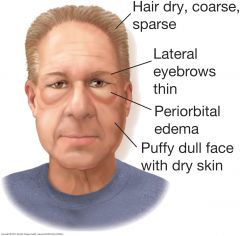
The patient with severe hypothyroidism (myxedema) has a dull, puffy facies. The edema often pronounced around the eyes, does not pit with pressure. The hair and eyebrows are dry, coarse, and thinned. The skin is dry.
|
|
|
Other Facies: Parotid Gland Enlargement |
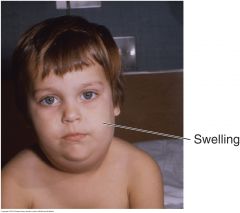
Chronic bilateral asymptomatic parotid gland enlargement may be associated with obesity, diabetes, cirrhosis, and other conditions. Note the swellings anterior to the ear loves and above the angles of the jaw. Gradual unilateral enlargement suggests neoplasm. Acute enlargement is seen in mumps
|
|
|
Other Facies: Acromegaly |
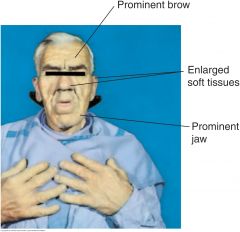
The increased growth hormone of acromegaly produces enlargement of both bone and soft tissues. The head is elongated, with bony prominence of the forehead, nose, and lower jaw. Soft tissues of the nose, lips and ears also enlarge. The facial features appear generally coarsened
|
|
|
Other Facies: Parkinson's Disease |
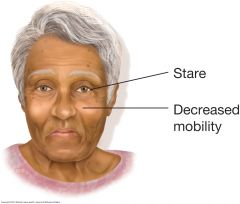
Decreased facial mobility blunts expression. A masklike face may result, with decreased blinking and a characteristic stare. Since the neck and upper trunk tend to flex forward, the patient seems to peer upward toward the observer. Facial skin becomes oily, and drooling may occur
|
|
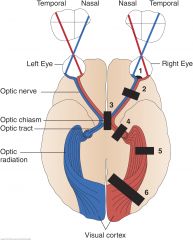
Visual Field Defects: Horizontal Defect (1)
|
Occlusion of a branch of the central retinal artery may cause a horizontal (altitudinal) defect. Ischemia of the optic nerve can produce a similar defect
|
|
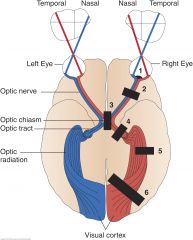
Visual Field Defects: Blind Right Eye (Right Optic Nerve) (2)
|

A lesion of the optic nerve and of course the eye itself, produces unilateral blindness
|
|
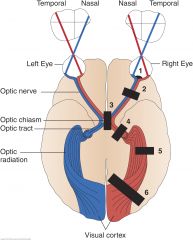
Visual Defects: Bitemporal Hemianopsia (optic chiasm) (3)
|
A lesion at the optic chiasm, may involve only fibers crossing over to the opposite side. Since these fibers originate in the nasal half of each retina. visual loss involves the temporal half of each field
|
|
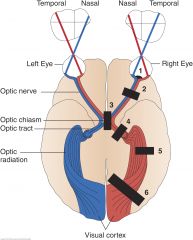
Left Homonymous Hemianopsia (right optic tract) (4)
|

A lesion of the optic tract, interrupts fibers originating on the same side of both eyes. Visual loss in the eyes is, therefore, similar (homonymous) and involves half of each field (hemianopsia)
|
|
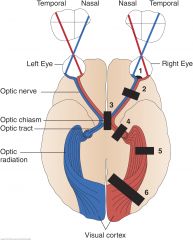
Homonymous Left Superior Quadrantic Defect (right optic radiation, partial) (5)
|
A partial lesion of the optic radiation in the temporal lobe, may involve only a portion of the nerve fibers, producing, for example, a homonymous quadrantic defect.
|
|
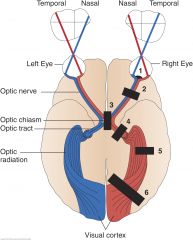
Left Homonymous Hemianopsia (right optic radiation) (6)
|

A complete interruption of fibers in the optic radiation, produces a visual defect similar to that produced by a lesion of the optic tract
|
|
|
Eyelid Abnormalities: Ptosis |
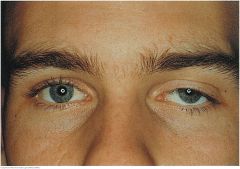
A drooping of the upper eyelid. Causes include myasthenia gravis, damage to the oculomotor nerve, and damage to the sympathetic nerve supply (Horner's syndrome). A weakened muscle, relaxed tissues, and the weight of the herniated fat may cause senile ptosis. May also be congenital
|
|
|
Entropion |
Entropion, more common in the elderly, is an inward turning of the lid margin. Lower lashes, which are often invisible when turned inward, irritate the conjunctiva and lower cornea. Ask patient to squeeze the lids together and then open them; then check for an entropion that is not obvious |
|
|
Ectropion |
Margin of the lower lid is turned outward, exposing the palpebral conjunctiva. When the punctum of the lower lid turns outward, the eye no longer drains well, and tearing occurs. More common in the elderly |
|
|
Lid retraction and Exophthalmos |
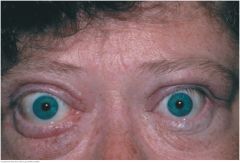
A wide-eyed stare suggests retracted eyelids. Note the rim of sclera between the upper lid and the iris. Retracted lids and "lid lag" when eyes move from up to down markedly increase the likelihood of hyperthyroidism, especially when accompanied by a fine tremor, moist skin, and heart rate >90 beats per minute
Exophthalmos decribes protrusion of the eyeball. A common feature of Graves' ophthalmopathy, triggered by autoreactive T lymphocytes. In this disorder, there are a spectrum of eye changes, ranging from lid retraction to extraocular muscle dysfunction, ocular pain, and lacrimation. Changes do not always progress. In unilateral exophthalmos, consider Graves' disease (usually bilateral), trauma, orbital tumor, and granulomatous disorders
|
|
|
Pinguecula |
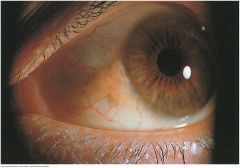
A harmless yellowish triangular nodule in the bulbar conjunctiva on either side of the iris. Appears frequently with aging, first on the nasal and then on the temporal side
|
|
|
Episcleritis |
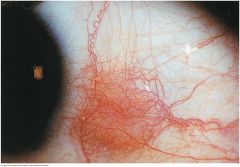
A localized ocular inflammation of the episcleral vessels. Vessels appear movable over the scleral surface. May be nodular or show only redness and dilated vessels. Seen in rheumatoid arthritis, Sjogren's syndrome, and herpes zoster
|
|
|
Sty |
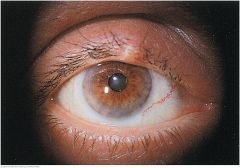
A painful, tender, red infection in a gland at the margin of the eyelid
|
|
|
Chalazion |
A subacute nontender, usually painless nodule involving a blocked meibomian gland. May become acutely inflamed but, unlike a sty, usually points inside the lid rather than on the lid margin
|
|
|
Xanthelasma |
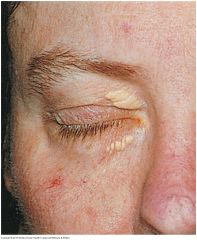
Slightly raised, yellowish, well-circumscribed plaques that appear along the nasal portions of one or both eyelids. May accompany lipid disorders.
|
|
|
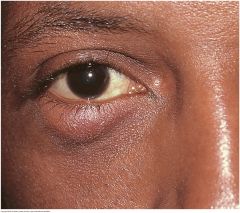
Inflammation of the Lacrimal Sac (Dacryocystitis) |

A swelling between the lower eyelid and nose. An acute inflammation is painful, red and tender. Chronic inflammation is associated with obstruction of the nasolacrimal duct. Tearing is prominent, and pressure on the sac produces regurgitation of material through the puncta of the eyelids.
|
|
|
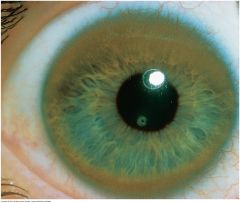
Corneal Arcus |

A thin grayish white arc or circle not quite at the edge of the cornea. Accompanies normal aging but also seen in younger people, especially African Americans. In young people, suggests possible hyperlipoproteinemia. usually benign
|
|
|
Kayser-Fleischer Ring |
A golden to red brown ring, sometimes shading to green or blue, from copper deposition in the periphery of the cornea found in Wilson's disease. Due to a rare autosomal recessive mutation of the ATO7B gene on chromosome 13 causing abnormal copper transport, reduced biliary cooper excretion, and abnormal accumulation of copper in the liver and tissues throughout the body. Patients present with liver disease, renal failure, and neurologic symptoms of tremor, dystonia, and psychiatric disorders ranging from behavior changes to depression and schizophrenia
|
|
|
Corneal Scar |

A superficial grayish white opacity in the cornea, secondary to an old injury or to inflammation. Size and shape are variable. Do not confuse with the opaque lens of a cataract, visible on a deeper plane and only through the pupil.
|
|
|
Pterygium |
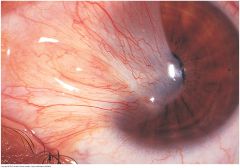
A triangular thickening of the bulbar conjunctiva that grows slowly across the outer surface of the cornea, usually from the nasal side. Reddening may occur. May interfere with vision as it encroaches on the pupil
|
|
|
Cataracts |

Opacities of the lenses visible through the pupil. Risk factors are older age, smoking, diabetes, corticosteroid use.
Nuclear cataract - looks gray when seen by a flashlight. If the pupil is widely dilated, the gray opacity is surrounded by a black rim
|
|
|
Peripheral Contact |
Produces spokelike shadows that point - gray against black, as seen with a flashlight, or black against red with an ophthalmoscope. A dilated pupil, as shown here, facilitates this observation
|
|
|
Fundi: Superficial Retinal Hemorrhages |

Small, linear, flame-shaped, red streaks in the fundi, shaped by the superficial bundles of the nerve fibers that radiate from the optic disc in the pattern illustrated (O=optic disc; F=fovea). Sometimes the hemorrhages occurs in clusters and look like a larger hemorrhage but can be identified by the linear streaking at the edges. These hemorrhages are seen in severe hypertension, papilledema, and occlusion of the retinal vein, among other conditions. An occasional superficial hemorrhage has a white center consisting of fibrin. White-centered retinal hemorrhages have many causes
|
|
|
Fundi: Preretinal Hemorrhage |

Develops when blood escapes into the potential space between the retina and vitreous. This hemorrhage is typically larger than retinal hemorrhages. Because it is anterior to the retina, it obscures any underlying retinal vessels. In an erect patient, red cells settle, creating a horizontal line of demarcation between plasma above and cells below. Causes include a sudden increase in intracranial pressure
|
|
|
Fundi: Deep Retinal Hemorrhages |

Small, rounded, slightly irregular red spots that are sometimes called dot or blot hemorrhages. They occur in a deeper layer of the retina than flame-shaped hemorrhages. Diabetes is a common cause
|
|
|
Fundi: Microaneurysms |

Tiny, round, red spots commonly seen in and around the macular area. They are minute dilatations of very small retinal vessels; the vascular connections are too small to be seen with an ophthalmoscope. A hallmark of diabetic retinopathy
|
|
|
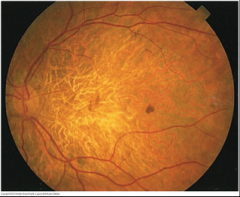
Fundi: Neovascularization |
Refers to the formation of new blood vessels. They are more numerous, more torturous, and narrower than other blood vessels in the area and form disorderly looking red arcades. A common feature of the proliferative stage of diabetic retinopathy. The vessels may grow into the vitreous, where retinal detachment or hemorrhage may cause loss of vision
|
|
|
Normal Fundus of a Light-Skinned Person |
Slightly darker fovea is just discernible No light reflex is visible in the subject Striped, or tessellated, character of the fundus, especially in the lower field
|
|
|
Normal Fundus of a Dark-Skinned Person |
Ring around the fovea is a normal light reflection The color of the fundus has a grayish brown, almost puprlish cast, which comes from pigment in the retina and the choroid that characteristically obscures the choroidal vessels No tessellation is visible
|
|
|
Hypertensive Retinopathy |

Marked arteriolar-venous crossing changes are seen, especially along the inferior vessels. Copper wiring of the arterioles is present. A cotton-wool spot is seen just superior to the disc. Incidental disc drusen are also present but are unrelated to hypertension |
|
|
Hypertensive Retinopathy with Macular Star |

Punctuate exudates are readily visibly: some are scattered; others radiate from the fovea to form a macular star. Note the two small, soft exudates about 1 disc diameter from the disc. Find the flame-shaped hemorrhages sweeping toward 7 o'clock and 8 o'clock; a few more may be seen toward 10 o'clock. These two fundi show changes typical of accelerated (malignant) hypertension and are often accompanied by papilledema
|
|
|
Hard Exudates |

Creamy or yellowish, often bright, lesions with well-defined "hard" borders. They are small and round but may coalesce into larger irregular spots. They often occur in clusters or circular, linear, or star-shaped patterns. Causes include diabetes and hypertension |
|
|
Healed Chorioretinitis |

Inflammation has destroyed the superficial tissues to reveal well-defined, irregular patch of white sclera marked with dark pigment. Size varies from small to very large. Toxoplasmosis is illustrated. Multiple, small, somewhat similar-looking areas may be due to laser treatments. Here there is also a temporal scar near the macula |
|
|
Serous Effusion |

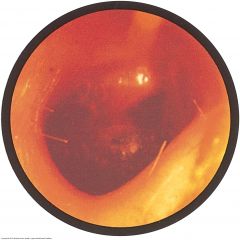
Usually caused by viral upper respiratory infections (otitis media with serous effusion) or by sudden changes in atmospheric pressure as from flying or diving (otitis barotrauma). The eustachian tube cannot equalize the air pressure in the middle ear and outside air. Air is absorbed from the middle ear into he bloodstream, and serous fluid accumulates there instead. Symptoms include fullness and popping sensations in the ear, mild conduction hearing loss, and sometimes, pain. Decreased eardrum mobility
Amber fluid behind the eardrum is characteristic, as in this patient with otitic barotrauma. A fluid level, a line between air above and amber fluid below, can be seen on either side of the short process. Air bubbles (not always present) can be seen here within the amber fluid.
|
|
|
Acute Otitis Media with Purulent Effusion |

Commonly caused by bacterial infection from S. pneumoniae and H. influenzae. Symptoms include earache, fever, and hearing loss. The eardrum reddens, loses its landmarks, and bulges laterally, toward the examiner's eye.
Here the eardrum is bulging, and most landmarks are obscured. Redness is most obvious near the umbo, but dilated vessels can be seen in all segments of the drum. A diffuse redness of the entire drum often develops. Spontaneous rupture (perforation) of the drum may follow, with discharge of purulent material into the ear canal.
Hearing loss is the conductive type. Acute purulent otitis media is much more common in children than in adults
|
|
|
Bullous Myringitis |
Painful hemorrhagic vesicles appear on the tympanic membrane, the ear canal, or both. Symptoms include earache, blood-tinged discharge from the ear, and conductive hearing loss.
In this right ear, at least two large vesicles (bullae) are discernible on the drum. The drum is reddened, and its landmarks are obscured.
This condition is caused by mycoplasma, viral, and bacterial otitis media
|
|
|
Angular Cheilitis |

Starts with softening of the skin at the angles of the mouth, followed by fissuring. It may be due to nutritional deficiency or, more commonly, to overclosure of the mouth, seen in people with no teeth or with ill-fitting dentures. Saliva wets and macerates the infolded skin, often leading to secondary infections with Candida, as seen here
|
|
|
Actinic Cheilitis |
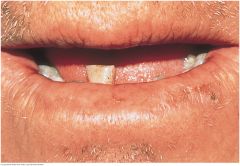
Results from excessive exposure to sunlight and affects primarily the lower lip. Fair-skinned men who work outdoors are most often affected. The lip loses its normal redness and may become scaly, somewhat thickened, and slightly everted. Because solar damage predisposes to carcinoma of the lip, examine such skin lesions carefully
|
|
|
Herpes Simplex (Cold Sore, Fever Blister) |

Produces recurrent and painful vesicular eruptions of the lips and surrounding skin. A small cluster of vesicles first develops. As there break, yellow-brown crusts form. Healing takes 10 to 14 days. Both new and erupted vesicles are visible here
|
|
|
Angioedema |

A localized subcutaneous or submucosal swelling caused by leakage of intravascular fluid into interstitial tissue. Two types are common. When vascular permeability is triggered by mast cells in allergic and NSAID reactions, look for assicated urticaria and pruritis. These are uncommon in angioedema from bradykinin and complement-derived mediators, the mechanism in ACE-inhibitor reactions. Angioedema is usually benign and resolves within 24 to 48 hours. It can be life threatening when it involves the larynx, tongue, or upper airway or develops into anaphylaxis
|
|
|
Hereditary Hemorrhaguc Telangiectasia (Osler-Weber-Rendu syndrome) |

Multiple small red spots on the lips strongly suggest this. An autosomal dominant endothelial disorder causing vascular fragility and arteriovascular malformations (AVMs). Telangiectasias are also visible on the oral mucosa and fingertips. Nosebleeds, gastrointestinal bleeding, and iron deficiency anemia are common. AVMs in the lungs and brain can cause life threatening hemorrhage and embolic disease
|
|
|
Peutz-Jeghers Syndrome |
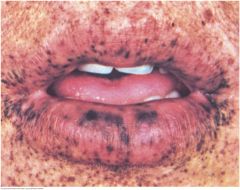
Look for prominent small brown pigmented spots in the dermal layer of the lips, buccal mucosa, and perioral area. These spots may appear on the hands and feet. In the autosomal dominant syndrome, these characteristic skin changes accompany numerous interstitial polyps. The risk of gastrointestinal and other cancers ranges form 40% to 90%. Note that spots rarely appear around the nose and mouth
|
|
|
Chancre of Primary Syphillis |

The ulcerated papule with an indurated edge usually appears after 3 to 6 weeks of incubating infection from spirochete Treponema pallidum. These lesions may resemble a carcinoma or crusted cold sore. Similar primary lesions are common in the pharynx, anus, and vagina but may escape detection since they are painless, nonsuppurative, and usually heal spontaneously
|
|
|
Carcinoma of the Lip |

Like actinic cheilitis, squamous cell carcinoma usually affects the lower lip. It may appear as a scaly plaque, as an ulcer with or without a crust, or as a nodular lesion, illustrated here. Fair skin prolonged exposure to the sun are common risk factors
|
|
|
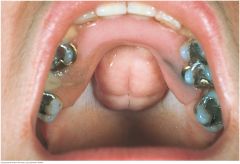
Large Normal Tonsils |

Normal tonsils may be large without being infected, especially in children. They may protrude medially beyond the pillars and even to the midline. Here they touch the sides of the uvula and obscure the pharynx. Their color is pink. The white marks are light reections, not exudate. |
|
|
Exudative Tonsillitis |

This red throat has a white exudate on the tonsils. This, together with fever and enlarged cervical nodes, increases the probability of group A streptococcal infection or infectious mononucleosis. Anterior cervical lymph nodes are usually enlarged in the former, posterior nodes in the latter. |
|
|
Pharyngitis |
Redness and vascularity of the pillars and uvula can be mild to moderate.
Redness is diffuse and intense.
Diphtheria, an acute infection caused by Corynebacterium diphtheriae, is now rare but still important. Prompt diagnosis may lead to life-saving treatment. The throat is dull red, and a gray exudate (pseudomembrane) is present on the uvula, pharynx, and tongue. The airway may become obstructed.Each patient would probably complain of a sore throat, or at least a scratchy one. Causes are both viral and bacterial. If the patient has no fever, exudate, or enlargement of cervical lymph nodes, the chances of infection by either of two common causes—group A streptococci and Epstein-Barr virus (infectious mononucleosis)—are small. |
|
|
Diphtheria |

Diphtheria, an acute infection caused by Corynebacterium diphtheriae, is now rare but still important. Prompt diagnosis may lead to life-saving treatment. The throat is dull red, and a gray exudate (pseudomembrane) is present on the uvula, pharynx, and tongue. The airway may become obstructed. |
|
|
Thrush on the Palate (Candidiasis) |

Thrush is a yeast infection from Candida species. Shown here on the palate, it may appear elsewhere in the mouth (see p. 289). Thick, white plaques are somewhat adherent to the underlying mucosa. Predisposing factors include (1) prolonged treatment with antibiotics or corticosteroids and (2) AIDS. |
|
|
Kaposi's Sarcoma in AIDS |

The deep purple color of these lesions suggests Kaposi’s sarcoma, a low-grade vascular tumor associated with human herpesvirus 8. The lesions may be raised or at. About a third of patients with Kaposi’s sarcoma have lesions in the oral cavity; other affected sites are the gastrointestinal tract and the lungs. Antiretroviral therapy has markedly reduced the prevalence of this disease. |
|
|
Torus Palatinus |
A torus palatinus is a midline bony growth in the hard palate that is fairly common in adults. Its size and lobulation vary. Although alarming at rst glance, it is harmless. In this example, an upper denture has been tted around the torus. |
|
|
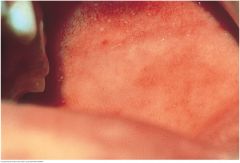
Pharynx, Palate, and Oral Mucosa: Fordyce Spots (Fordyce Granules) |

Fordyce spots are normal sebaceous glands that appear as small yellowish spots in the buccal mucosa or on the lips. Here they are seen best anterior to the tongue and lower jaw. These spots are usually not numerous. |
|
|
Koplik's Spots |
Koplik’s spots are an early sign of measles (rubeola). Search for small white specks that resemble grains of salt on a red background. They usually appear on the buccal mucosa near the rst and second molars. In this photo, look also in the upper third of the mucosa. The rash of measles appears within a day. |
|
|
Petechiae |

Petechiae are small red spots caused by blood that escapes from capillaries into the tissues. Petechiae in the buccal mucosa, as shown, are often caused by accidentally biting the cheek. Oral petechiae may be due to infection or decreased platelets, as well as trauma. |
|
|
Leukoplakia |

A thickened white patch (leukoplakia) may occur anywhere in the oral mucosa. The extensive example shown on this buccal mucosa resulted from frequent chewing of tobacco, a local irritant. This benign reactive process of the squamous epithelium may lead to cancer and should be biopsied. Another risk factor is human papillomavirus infection. |
|
|
Hyperthyroidism |
Symptoms: Nervousness Weight loss despite increased appetite Excessive sweating and hear intolerance Palpitations Frequent bowel movements Tremor and proximal muscle weakness
Signs: Warm, smooth, moist skin With Graves' disease, eye signs such as store, lid lag, exophthalmos Increased systolic and decreased diastolic blood pressures Tachycardia or atrial fibrillation Hyperdynamic cardiac pulsations with an accentuated S1 Tremor and proximal muscle weakness Localized systolic or continuous bruit can be heard over the lateral lobes |
|
|
Hypothyroidism |
Symptoms: Fatigue, lethargy Modest weight gain with anorexia Dry, coarse skin and cold intolerance Swelling of face, hands, and legs Constipation Weakness, muscle cramps, arthralgias, paresthesias, impaired memory and hearing
Signs: Dry, coarse, cool skin, sometimes yellowish from carotene, with nonpitting edema and loss of hair Periorbital puffiness Decreased systolic and increased diastolic blood pressures Bradycardia and, in late stages, hypothermia Sometimes decreased intensity of heart sounds Impaired memory, mixed hearing loss, somnolence, peripheral neuropathy, carpal tunnel sydrome |

