![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
What are symptoms of low cardiac output? |
-Dyspnea -HF symptoms -Syncope |
|
|
In a female, what are early warning symptoms of acute MI? |
-Unusual fatigue -Sleep disturbance -SOB -Indigestion -Anxiety |
|
|
Symptoms reported by women during acute coronary syndrome? |
-SOB -Weakness -Unusual fatigue -Diaphoresis ("Cold sweat") -Dizziness -Chest pain or pressure (30%) -No chest discomfort during event (43%) |
|
|
ACS in the elder - Clinical presentation ≥ 75 years of age |
-Dyspnea -Neurological sxs: syncope, weakness, acute confusion -Chest pain or pressure (< 50%)
**ACS should be considered a possibility in any acute illness in an elder |
|
|
A healthy adult's heart is roughly.... |
1/3 right heart and 2/3 left heart |
|
|
In which side of the heart are the majority of cardiac problems found? |
-The left side of the heart is such a high pressure system, attempting to overcome the PVR w/ every heartbeat, the majority of cardiac problems are found in the left side of the heart. Particularly the valvular problems.
Mitral valve disease and Aortic Valve disease are more common than Pulmonic or tricuspid valve disease
Higher pressure L side of heart Lower pressure R side of heart
|
|
|
Normal PMI |
-Size of impulse = about the area of a nickel
-Location = 5th ICD, MCL
-Sensation = gentle tap by one finger, single impulse
-Time = PMI takes about 1/3 of systole |
|
|
Displaced PMI.... |
-Usually displaced laterally
-Indicates increased LV volume (e.g., LVH) |
|
|
Unusually forceful, sustained PMI.... |
-Pressure overload, HTN |
|
|
Big waves on an ECG indicate... |
a big left ventricle |
|
|
If you cannot palpate the PMI on a patient, what can you do? |
Move the patient into the left lateral decubitus position to enhance the PMI
Consider concomitant conditions: -Thick chest wall (e.g., body builder) -Obesity -COPD (Increased A-P diameter) |
|
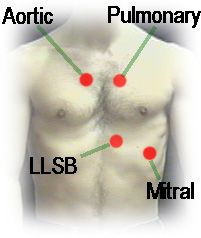
Cardiac Auscultation |
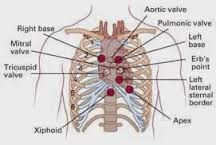
|
|
|
Pathway of blood through the heart |
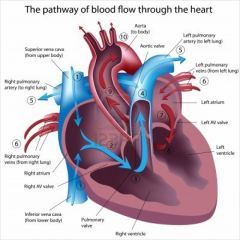
|
|
|
Heart sounds -
S1 |
-Marks the beginning of systole -Produced by events surrounding the closure of mitral and tricuspid valve
-Best heard at the apex w/ the diaphragm
-"Lub" of "lub-dub" -Heard nearly simultaneously with the carotid upstroke |
|
|
Heart sounds -
S2 |
-Marks the end of systole -Produced by events surrounding the closure of the aortic and the pulmonic valves
-Best heard at the base with diaphragm
-"Dub" of "lub-dub"
*When the HR, < 120 bpm, generally diastole is longer than systole; when HR ≥ 120, Systole and diastole are pretty much the same length |
|
|
Heart sounds -
Physiologic split S2 |
Significance: widening of normal interval between aortic and pulmonic components of the second heart sound. Caused by a delay in the pulmonic component
-Heard best in pulmonic region
-Split increases on patient inspiration
-Found in the majority of adults < age 30, fewer beyond this age
-A benign finding |
|
|
Heart sounds -
Pathologic split S2 |
Significance: -Fixed split - No change w/ inspiration -Paradoxical split - narrows or closes on inspiration
-Heard best in pulmonic region
-Fixed split often found in uncorrected atrial septal defect (ASD)
-Paradoxical split often found in conditions that delay aortic closure such as LBBB
-Finding can resolve w/ tx of underlying condition |
|
|
Heart sounds -
Pathologic S3 heart sounds (aka S3) |
-Marker of ventricular overload and/or systolic dysfunction (part of the pathophysiology of HF)
-Heard in early diastole, can sound like it's "hooked on" to the back of S2 -Low-pitch, best heard w/ bell, might miss w/ diaphragm
-For dx of HF, correlate w/ add'l findings such as dyspnea, tachycardia, crackles
-Finding can resolve w/ treatment of underlying condition
|
|
|
Heart sounds -
S4 heart sound |
-Marker of poor diastolic function, most often in poorly controlled HTN or recurrent MI
-Heard best in late diastole, can sound like it's "hooked on" to the front of S1 -Sometimes called a presystolic sound -Soft, low-pitch (higher than S3), best heard w/ bell
-Finding can resolve w/ tx of underlying condition |
|
|
Heart valve dysfunction -
Failure to open adequately |
Stenosis |
|
|
Heart Valve dysfunction -
Failure to close adequately |
Incompetent - Incompetent valves cause regurgitant murmurs |
|
|
Systolic cardiac murmurs |
-may be benign or pathologic
-Mitral -Regurgitation -Physiologic -Aortic -Stenosis -Systolic
Mitral regurgitation: holosystolic, takes up all of systole and is the same intensity throughout systole
Aortic Stenosis: A crescendo-decrescendo (louder-softer) systolic murmur |
|
|
MR PASS wins the Most Valuable Player Award |
-Mitral -Valve -Prolapse
-Mid- to late-systolic mumur -Usually preceded by a mid-systolic click |
|
|
Diastolic cardiac murmurs |
-Always pathologic
-Mitral -Stenosis -Aortic -Regurgitation -Diastolic
-Mitral stenosis: a later diastolic murmur -Aortic regurgitation: Earlier diastolic murmur |
|
|
Grading Heart Murmurs - the sound of turbulent blood flow |
I - very faint
II - Quiet but immediately heard
III - Moderately loud without thrill (about as loud as S1 or S2)
IV - Loud w/ thrill (tremor or vibration on palpation)
V - Very loud with thrill
VI - Audible w/o stethoscope |
|
|
Character of murmurs |
Harsh: heard well w/ bell & diaphragm (Ex- murmur of aortic stenosis)
Rumble: low, heard best w/ bell (Ex- murmur of mitral stenosis)
Blowing: High, heard best w/ diaphragm (Ex - murmur of aortic regurgitation)
Musical: Vibratory quality (Ex- still murmur [benign childhood murmur]) |
|
|
Systolic murmurs - Benign (aka physiologic, flow, functional) or pathologic? |
Likely benign - consider benign only if all noted:
-Negative hx
-lower grade (≤ Gr III/VI)
-No radiation beyond the precordium (i.e. all over the chest)
-S1, S2 intact
-No heave or thrill
-PMI WNL (5th ICS MCL)
-Soften or disappears w/ supine to stand position change (*Chief characteristic of physiologic murmurs)
*Supine is the preferred position for cardiac auscultation at least to start cardiac exam --> heart is more filled w/ blood than when person is standing; When stand pt up, heart gets taller, thinner, "less fluid in the pump" --> murmur either softens or disappears. Again, this is the chief characteristic of physiologic murmurs
|
|
|
Radiating Murmur vs. Carotid Artery Bruit? |
Carotid Bruit: -Usually softer -Often unilateral -Different sound than that found in chest
Radiating Murmur: -Usually louder -Bilateral -Same sound and timing as found in chest |

