![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
282 Cards in this Set
- Front
- Back
|
What range of frequencies does the stethoscope diaphragm detect? |
Sounds having frequencies of 100 - 400 Hz
|
|
|
What is the highest frequency heart sound? What part of the stethoscope is best for hearing this high frequency heart sound?
|
Diastolic murmur of Aortic insufficiency which is best heard w/ the diaphragm of the stethoscope
|
|
|
What frequencies does the bell of the stethoscope detect?
|
Detects low frequency sounds less than 100 Hz
|
|
|
What is the lowest frequency heart sound? what part of the stethoscope is best for listening to this heart sound?
|
Diastolic murmur of mitral stenosis and S3 and S4 are the lowest frequency heart sounds and are heard best w/ the bell of the stethoscope
|
|
|
What effect does the tubing length of the stethoscope have on auscultation?
|
The shorter the tubing the better high-pitched sounds are transmitted to the ear
|
|
|
What direction must the ear pieces of the stethoscope point? What effect would ear pieces that are too small have on auscultation?
|
Ear pieces must point forward, if the ear pieces are too small for the ear canals they may occlude or prevent a seal from forming and thereby diminish the intensity of the heart sounds
|
|
|
Where is the Aortic Valve heard best?
|
In the second right intercostal space adjacent to the sternum, as well as the 3rd left intercostal space to the cardiac apex
|
|
|
Where is the pulmonic valve heard best?
|
The second and third left intercostal spaces adjacent to the sternum
|
|
|
Where is the tricuspid valve heard best?
|
In the fourth and fifth left intercostal spaces along the sternal border
|
|
|
Where is the mitral valve heard best?
|
Just medial to or at the cardiac apex
|
|
|
Where is the left ventricular area grossly on the thorax?
|
Located at the cardiac apex
|
|
|
Where is the right ventricular area grossly on the thorax?
|
In the 4th intercostal space at the sternal border and distal to the xiphoid in pts w/ emphysema
|
|
|
Where is the right ventricular area in pts w/ emphysema?
|
Distal to the xiphoid
|
|
|
What produces S1?
|
Closure of the mitral and tricuspid valve
|
|
|
What does S1 mark?
|
The onset of ventricular systole and the end of ventricular diastole
|
|
|
Where is S1 louder than S2? what portion of the stethoscope should you use to listen to S1?
|
Normally S1 is louder than S2 at the cardiac apex and either the bell or diaphragm can be used
|
|
|
Where is splitting of S1 normally heard?
|
Normally splitting of S1 into its two components is audible adjacent to the lower left sternal border
|
|
|
How far apart does normal splitting of S1 into its component parts occur?
|
.02-.03 seconds apart
|
|
|
What causes splitting of S1 to be heard at the cardiac apex?
|
A 4th heart sound and mitral valve closure; or mitral valve closure and an ejection sound
|
|
|
When does wide splitting of S1 occur? why?
|
In RBBB; b/c there is delayed closure of the tricuspid valve
|
|
|
Why is S1 heard at the cardiac apex unusual?
|
B/c normally the sound produced by TV closure is too faint to be heard at the apex
|
|
|
When is S1 increased in intensity?
|
When it is louder than S2 in the second intercostal spaces
|
|
|
What does intensity of S1 depend on?
|
1. the rate of pressure development in the ventricles
2. thickness of the AV valve leaflets 3. position of the AV valve leaflets at the start of ventricular contraction |
|
|
What can cause S1 to have increased intensity? what causes these conditions?
|
When contractility and myocardial tension development are increased
*Caused by: 1. Anemia 2. Pregnancy 3. Hyperthyroidism 4. Anxiety 5. Fever |
|
|
What heart sound is caused by a short PR interval? What quantifies a short PR interval? What affect does this have on the heart sound?
|
A short P-R interval (quantified by .11-.13 seconds) on the EKG causes the ventricles to contract before the atria have had a chance to relax. SO the MV/TV valves are fully open when the ventricles start to contract and S1 is increased in intensity
|
|
|
What causes the PR interval to be shorter?
|
Mitral stenosis causes the mitral valve to be fully open at the onset of LV contraction and S1 to be increased in intensity
|
|
|
How can TV/MV stenosis severity be judged based on heart sounds?
|
The thicker the AV valve leaflets, the louder the S1 heart sound. SO the louder the sound the worse the stenosis
|
|
|
When is S1 decreased in intensity?
|
When S2 is louder than S1 at the cardiac apex
|
|
|
What causes S1 to have decreased intensity?
|
1. When contractility and myocardial tension development are decreased (CHF)
2. When the MV is so calcified that it is completely immobile (calcific mitral stenosis) 3. When the MV valve is nearly closed at the start of ventricular contraction |
|
|
What detectable auscultation symptoms are caused by 1st degree heart block?
|
Prolongation of the PR interval to greater than .20 seconds on EKG
1st degree AV block delays the onset of ventricular contraction and allows the AV valve leaflets to float mostly shut following the completion of atrial contraction, this causes S1 to have decreased intensity |
|
|
What causes S1 to vary beat to beat?
|
When the position of the AV valves at the start of ventricular contraction changes from beat to beat
|
|
|
What is the most common cause for S1 to have variable intensity?
|
Atrial fibrillation
|
|
|
What produces S2?
|
Closure of the aortic and pulmonic valves in that order
|
|
|
What does S2 mark?
|
Marks the end of systole and the onset of diastole
|
|
|
What is different about S2 compared to S1?
|
S2 is higher pitched and shorter in duration that S1
|
|
|
Where is S2 normally louder than S1? what part of the stethoscope is used to hear S2?
|
In the second intercostal space; S2 is heard best w/ the diaphragm or the bell
|
|
|
What effect does a pt sitting upright have on S2? What effect does age have on S1 and S2?
|
Both the aortic and pulmonic components of S2 are normally audible in the 2nd intercostal space in a upright adult, the ability to hear both components decreases w/ age and most elderly pts do not have detectable splitting of S2
|
|
|
What produces the first component of S2? where is it audible?
|
Closure of the Aortic Valve (A2); it is audible pretty much everywhere on the precordium
|
|
|
What produces the second component of S2? where is it audible?
|
Produced by closure of the pulmonic valve (P2) and is normally only heard in the 2nd and 3rd left intercostal spaces
|
|
|
What does it mean if you hear P2 at the cardiac apex?
|
It is bad, it means that the PV is closing w/ extra force, consistent w/ pulmonic HTN
|
|
|
What does it mean if you hear a suspicious sound while the pt is supine but you do not hear it when the pt sits up?
|
It means the sound did not really exist and it was artifactual
|
|
|
What causes the intensity (loudness) of S2 to decrease?
|
When the Ao valve or Pu valve leaflets are fused together, or have stenosis
|
|
|
When is the intensity of S2 increased?
|
When it is louder than S1 at the cardiac apex
|
|
|
What causes an increased intensity of S2? why?
|
systemic HTN or pulmonary HTN; b/c they cause the valve leaflets to close w/ more force
|
|
|
What is normal physiologic splitting of S2?
|
When the time interval b/e A2 and P2 widens during inspiration and narrows during expiration while the pt is breathing normally
|
|
|
What components of S2 can be heard during inspiration? expiration?
|
Inspiration: both Ao and Pu components of S2 can be heard
Expiration: only A2 can be heard |
|
|
What is the underlying mechanism that causes normal physiologic widening of S2?
|
The split relates to a delay in closure of the PV w/ inspiration
|
|
|
How do intrathoracic pressure and venous return relate to normal physiologic splitting of S2?
|
Intrathoracic pressure falls and venous return to the right side of the heart increases during inspiration, thus inspiration increases RV filling and and lengthens the time for RV ejection. This causes closure of the PV to be delayed
|
|
|
What effect does lung inflation during inspiration have on S2?
|
Causes splitting of S2 b/c when pulmonary vascular resistance decreases and then the RV contracts it pushes the blood column out. When the blood column encounters a low resistance system then the blood will keep flowing longer and will delay closure of the PV, causing a wide, split, S2
|
|
|
What effect does lung expiration/deflation have on S2?
|
When the blood column ejected by the RV encounters a high resistance wall in the lungs it is not able to travel as far so as soon as the RV stops contracting it will stop flowing and will slam the pulmonic valve closed, causing a narrow S2
|
|
|
When can you rule out heart dz entirely just from auscultation?
|
When you hear normal physiologic splitting
|
|
|
What time interval does the S2 split narrow to during expiration?
|
.01-.02 second and is heard as only one sound b/c the human ear cannot distinguish b/e sounds that occur .02 seconds apart
|
|
|
What causes wide physiologic splitting of S2? what time interval does S2 occur at during inspiration and expiration?
|
Caused by a delay in closure of P2 or early closure of A2; S2 widens to .06 seconds during inspiration and narrows to .03-.04 seconds during expiration
(so the split is heard during both inspiration and expiration but the split varies in length) |
|
|
If both components of S2 can be heard during expiration what condition is that?
|
Wide physiologic splitting of S2
|
|
|
What conditions cause wide physiologic splitting of S2?
|
Conditions that prolong RV ejection (pulmonary stenosis), that delay RV ejection (RBBB) or that shorten LV ejection (mitral regurgitation or a VSD)
|
|
|
What is RBBB?
|
"Right bundle-branch block"; is a problem of condition to the right ventricle where there is delayed activation of the RV
|
|
|
What age group is it normal to have wide physiologic splitting? What age group is it abnormal to have wide physiologic splitting?
|
May be normal in young adults but is nearly always physiologic in pts older than 50 years
|
|
|
What is wide fixed splitting of S2?
|
Present when splitting is detectable during both inspiration and expiration and does not change with breathing
|
|
|
What pathology causes a wide fixed splitting of S2? why?
|
Atrial Septal Defects cause wide fixed splitting b/c the left-right shunting of blood causes RV volume to constantly be elevated and exceeding LV volume which causes RV ejection to be prolonged causing a delayed P2
|
|
|
What is reversed "paradoxical" splitting of S2?
|
Essentially it is backwards of normal, it is present when the splitting of S2 narrows during inspiration and widens during expiration. Reversed splitting results from severe prolongation of LV ejection such that A2 occurs AFTER P2
|
|
|
What is the most common cause of paradoxical splitting of S2? why?
|
Left bundle-branch block; b/c LBBB causes RV ejection to finish before LV ejection, so P2 occurs before A2
|
|
|
What pathologies can cause paradoxical splitting of S2?
|
1. LBBB
2. severe Aortic stenosis 3. hypertrophic obstructive cardiomyopathy (HOCM); where LV ejection is markedly prolonged |
|
|
What pathology causes narrow physiologic splitting of S2?
|
Severe pulmonary HTN b/c RV ejection is markedly abbreviated due to abnormally high pulmonary vascular resistance
|
|
|
When does pulmonary HTN cause narrow physiologic splitting of S2? wide splitting of S2?
|
When pulmonary HTN is severe it causes a narrow splitting b/c RV ejection is markedly abbreviated, wide splitting develops in pulmonary HTN when RV failure eventually occurs
|
|
|
When is narrow physiologic splitting of S2 normal? abnormal?
|
It is normal in the elderly but bad in young people
|
|
|
What happens to the P2 component of S2 in narrow physiologic splitting of S2?
|
P2 closure sound is increased in intensity (louder) and may even be palpable in the 2nd LICS
|
|
|
What does a palpable P2 mean?
|
It means that mean pulmonary artery pressure is > 50mmHg
|
|
|
What is S3?
|
A low-pitched sound that is audible almost exclusively w/ the bell of the stethoscope
|
|
|
When is a S3 bad? okay?
|
S3 is often normal in adolescents and young adults but in people older than 40 it is nearly always pathologic
|
|
|
During what time of the cardiac cycle does S3 occur in?
|
Occurs in early diastole (.12-.20 seconds after S2)
|
|
|
Where is S3 heard if it originated in the LV?
|
If S3 originated in the LV it is heard at the apex
|
|
|
How can you improve your ability to hear S3?
|
By placing the pt in the left lateral decubitis position, but you have to listen as they turn because you can only hear the murmur for a few beats after they turn then it fades
|
|
|
Where can you hear S3 if it originated in the RV?
|
It is localized to the 4th left intercostal space adjacent to the sternum
|
|
|
What causes S3?
|
When the ventricle reaches its elastic limit in early rapid diastolic filling. Basically it is caused by blood slamming into the walls of the ventricle during filling
|
|
|
What pathology causes S3?
|
1. Systolic heart failure, which causes a dilated LV w/ a low ejection fraction
2. Valvular Regurgitation and High Output States - when an excessive amount of blood enters an otherwise normally functioning ventricle |
|
|
What does S3 in a older adult indicate?
|
That the ventricular ejection fraction is significantly depressed
|
|
|
What does the absence of S3 indicate in an older adult?
|
Indicates that ejection fraction is > 30%
|
|
|
When does the presence of S3 NOT indicate a poor ejection fraction or elevated filling pressure?
|
When S3 is produced by valvular regurgitation and high cardiac output states
|
|
|
What are a few high cardiac output states?
|
1. pregnancy
2. anemia |
|
|
When does the intensity (loudness) of S3 increase?
|
During inspiration and during maneuvers that increase venous return (such as feet elevation)
|
|
|
What heart sound can be described as a protodiastolic gallop?
|
S3
|
|
|
What are some special characteristics of a LV S3?
|
S3 decreases in intensity during inspiration and varies little w/ maneuvers that increase venous return
|
|
|
Is atrial contraction necessary for S3?
|
Nope
|
|
|
What is S4?
|
A low-pitched ("atrial") sound that is heard almost exclusively w/ the bell of the stethoscope
|
|
|
When does S4 occur during the cardiac cycle?
|
During late diastole (.04-.12 seconds prior to S1)
|
|
|
What heart sound is described as a presystolic gallop?
|
S4
|
|
|
Where can you hear a S4 that originates in the LV?
|
At the cardiac apex
|
|
|
How can you position the pt to better hear S4?
|
Placing them in the left lateral decubitis position allows S4 to be heard better
|
|
|
Where can you hear a S4 that originates in the RV?
|
To hear a RV S4 you listen in the left intercostal space adjacent to the sternum
|
|
|
When is S4 normal? abnormal?
|
Abnormal in pts older than 40 years but can be completely normal in adolescents and young adults
|
|
|
What causes S4?
|
Forceful atrial contraction that ejects blood into a stiff and non-compliant left ventricle w/ an elevated filling pressure
|
|
|
What causes decreased ventricular compliance?
|
Concentric ventricular hypertrophy and myocardial infarction
|
|
|
What pathology causes a pt to definitely NOT have a S4?
|
Atrial fibrillation
|
|
|
What causes RV concentric hypertrophy?
|
Pulmonary HTN and pulmonic stenosis
|
|
|
What causes LV concentric hypertrophy?
|
Systemic HTN and Aortic stenosis
|
|
|
What causes a RV/LV S4 to increase or decrease in intensity?
|
Inspiration: RV S4 increases in intensity during inspiration and LV S4 decreases in intensity during inspiration
Expiration: RV S4 decreases in intensity during expiration and LV S4 increases in intensity during expiration |
|
|
What can cause a LV S4 to decrease to the point of inaudibility?
|
Standing
|
|
|
How can you distinguish a LV S4 from a split S1?
|
By location (S1 is loudest at the LSB and S4 is loudest at the apex)
By the fact that S4 is virtually inaudible w/ the diaphragm of the stethoscope |
|
|
What is a opening snap?
|
A high-pitched snap that occurs in early diastole and follows A2 by .03-.15 seconds
|
|
|
What produces the opening snap?
|
Forceful opening of the mitral or tricuspid valve in mitral or tricuspid stenosis
|
|
|
Where can you hear the OS of the mitral valve?
|
It is located half-way b/e the lower left sternal border and the cardiac apex
|
|
|
Where can you hear the OS of the tricuspid valve?
|
It is located in the 4th intercostal space at the left sternal border
|
|
|
How can you distinguish b/e a split S2 from a S2-OS?
|
1. A S2-OS is most likely when the second component of the split sound is louder at the apex than in the second LICS
2. A S2-OS is most likely when the interval b/e the two sounds becomes wider after standing |
|
|
How can you measure the severity of mitral stenosis using A2-OS?
|
The shorter the A2-OS interval, the more severe the mitral stenosis, the shorter the interval the higher the LA stenosis, the quicker the OS occurs after S2
|
|
|
What is an ejection sound?
|
A high-pitched sound that follows S1 by .04-.06 seconds
|
|
|
Where do ejection sounds originate from?
|
1. forceful contraction of blood into the great vessels
2. the opening of an abnormal or stenotic semilunar valve |
|
|
What sound indicates valvular or vascular pathology until proven otherwise?
|
Ejection sound
|
|
|
Where is the ejection sound of pulmonic stenosis located? how can severity be judged?
|
Localized to the 2nd and 3rd LICS and decreases in intensity during inspiration. The closer the pulmonic ejection sound occurs to S1, the more severe is the pulmonic stenosis
|
|
|
Where is the ejection sound of idiopathic pulmonary HTN located?
|
Localized to teh 2nd and 3rd LICS and DOES NOT change appreciably w/ breathing
|
|
|
Where does the ejection sound of valvular aortic stenosis occur? bicuspid Aortic valve?
|
Loudest in the 2nd RICS but may also be prominent at the apex
|
|
|
How does the aortic ejection sound vary in intensity?
|
The ejection sound of aortic ejection has a constant intensity throughout the respiratory cycle
|
|
|
What causes Aortic ejection sounds?
|
Dilation of the aortic root and systemic HTN
|
|
|
What is the relationship b/e ejection sounds and an accompanying murmur?
|
An ejection sound in the presence of an accompanying murmur almost always indicates that the murmur is pathologic
|
|
|
What is a mid-systolic click?
|
A high-pitched sound that occurs in the middle third of systole
|
|
|
What produces a mid-systolic click?
|
Produced when mitral or tricuspid valve leaflets prolapse into the atria during ventricular contraction
|
|
|
If you hear a mid-systolic click what can you immediately diagnose?
|
Mitral or tricuspid valve prolapse w/o the need for cardiac ultrasound
|
|
|
What causes a MSC to move closer to S1? S2?
|
The MSC moves closer to S1 w/ maneuvers that decrease the intracavitary size of the LV (sustained valsalva or standing)
The MSC moves closer to S2 w/ maneuvers that increase the intracavitary size of the LV (elevation of the legs or squatting) |
|
|
How could you tell whether a pt has Aortic stenosis or pulmonic stenosis?
|
If the pt has an opening snap the sound decreases in intensity w/ inspiration if they have pulmonic stenosis, whereas if they have aortic stenosis then it stays at a constant intensity throughout the respiratory cycle
|
|
|
What heart sound do pts with a bicuspid aortic valve have? what is a bicuspid aortic valve?
|
Pts w/ a bicuspid aortic valve have a opening snap, a bicuspid valve is a congenital condition that puts the pt at risk for developing Aortic stenosis in their 40s
|
|
|
How can you tell pulmonic stenosis from any other right-sided heart condition's sound?
|
During inspiration the ejection sound caused by pulmonic stenosis gets softer (less intense), and the sound gets louder during exhalation. EVERY other right-sided sound is the opposite
|
|
|
What causes the mitral/tricuspid valves to prolapse?
|
The chordae tendinae are too long, which causes the valve to prolapse when the ventricle is fully contracted (which happens in midsystole). SO what causes the sound? the click is the sound of the chordae tendinae which were slack while the ventricle was contracting suddenly get tight as the valve prolapses into the atrium
|
|
|
What causes murmurs?
|
Turbulence in the heart or great vessels
|
|
|
What is the most common cause of murmurs?
|
Abnormal heart valves
|
|
|
What is a bruit?
|
A "murmur" that occurs in arteries, caused by turbulence
|
|
|
What characterizes murmurs?
|
1. Location on the cardiac cycle
2. Frequency characteristics 3. Intensity 4. Shape 5. Location on the chest wall 6. Duration 7. Direction of radiation/transmission |
|
|
How can you characterize a murmur based on location in the cardiac cycle?
|
Whether the murmur is systolic or diastolic
|
|
|
How can you characterize a murmur based on frequency?
|
Is it low-pitched? high-pitched? heard only w/ the bell?
|
|
|
How can you characterize a murmur based on intensity?
|
Does the murmur's intensity change over time? B/c innocent murmurs do not get worse over time
|
|
|
What is a Grade 1/6 murmur?
|
Faint and inaudible unless you really "tune in" or listen hard for the murmur
|
|
|
What is a grade 2/6 murmur?
|
Still faint but loud enough to be heard immediately when the stethoscope is first placed on the chest
|
|
|
What is a grade 3/6 murmur?
|
Intermediate in intensity, but not loud. Basically a moderately loud murmur w/o a thrill
|
|
|
What is a grade 4/6 murmur?
|
Loud and associated w/ a palpable vibration (thrill)
|
|
|
What is a grade 5/6 murmur?
|
Loud and still associated w/ a thrill but this murmur is audible when the rim of the diaphragm is placed on the pts chest
|
|
|
What is a grade 6/6 murmur?
|
Loud and still associated w/ a thrill and is audible w/o a stethoscope
|
|
|
What are the major versions of systolic murmurs?
|
1. midsystolic
2. holosystolic 3. late systolic variant of the holosystolic murmur |
|
|
What produces midsystolic murmurs?
|
Anterograde flow across the aortic and pulmonic outflow tracts
|
|
|
What produces holosystolic murmurs?
|
retrograde flow from a high pressure cardiac chamber into a lower pressure cardiac chamber
|
|
|
What are the two major categories of diastolic murmurs?
|
1. early diastolic
2. late diastolic |
|
|
What causes early diastolic murmurs?
|
Retrograde flow across incompetent aortic or pulmonic valves
|
|
|
What causes late diastolic murmurs?
|
Anterograde flow across a narrowed mitral or tricuspid valve orifice
|
|
|
When do midsystolic murmurs start, end and peak?
|
Start after S1, End before S2 and peak in the middle third of systole
|
|
|
What is the "shape" of midsystolic murmurs?
|

Diamond-shaped (crescendo-decrescendo) and tend to be harsh and saw-like in quality
|
|
|
What murmurs exhibit post-extrasystolic potentiation?
|
Midsystolic murmurs
|
|
|
What is postextrasystolic potentiation?
|
The murmur increases one-grade in intensity during the beat following a brief interruption in the cardiac rhythm, or the murmur suddenly gets stronger on the NEXT beat after a extra beat
|
|
|
Why does postextrasystolic potentiation cause midsystolic murmurs to suddenly get stronger?
|
B/c there is more Ca in the SERCA which increases contractility and the longer diastole b/e the extra beat and the stronger beat means there was longer filling time, so there was a higher preload. Combined these both mean that the SV was much higher after that beat. SO b/c the increased force and volume ejected from the ventricle causes the murmur to have higher intensity
|
|
|
What conditions cause increased rate/volume of blood to be ejected through a normal aortic or pulmonic outflow tract? What murmur would this produce?
|

These would produce a midsystolic murmur that peaks prior to midsystole: ("A" in the picture)
1. Maximum aerobic exercise 2. Pregnancy 3. Anemia 4. Hyperthyroidism 5. Systemic arteriovenous fistulas |
|
|
What condition would cause ejection of blood into a dilated aorta? What murmur would be produced?
|

Aortic Root dilation (aneurysm); and would produce a midsystolic murmur that peaks prior to mid-systole ("A" in the picture)
|
|
|
What condition would cause ejection of blood across thickened valve cusps or an uneven lining of the aorta? what murmur would be produced?
|
Aortic sclerosis (athersclerotic roughening of the aortic lining); it would produce a midsystolic murmur that peaks prior to midsystole ("A" in the pic)
|
|
|
What condition would cause ejection of blood through a narrow aortic or pulmonic outflow tract? what murmur would be produced?
|

Subvalvular, valvular and post-valvular stenosis; these would produce a midsystolic murmur that peaks during mid-to-late systole ("C" in the picture)
|
|
|
What murmur does aortic stenosis produce?
|
A midsystolic murmur when blood is ejected is ejected through a narrowed aortic valve orifice
|
|
|
What is the range of intensity of the murmur that aortic valve stenosis produces?
|
Grade 1 to Grade 4 depending on the severity of the obstruction and the degree of LV function
|
|
|
When does the murmur produced by Aortic valve stenosis peak? where is it loudest? How can the peak of the murmur be used to judge the severity of the stenosis?
|
In mid-late systole, it is loudest at the 2nd RICS; where to murmur peaks can be used to judge the severity of the stenosis
|
|
|
What part of the stethoscope can be used to hear a murmur produced by aortic valve stenosis?
|
Either the bell or the diaphragm
|
|
|
What precedes a aortic valve stenosis murmur?
|
An ejection sound that is also loudest in the second RICS
|
|
|
What pulse abnormality is produced by aortic valve stenosis?
|
A narrow pulse pressure and a slow delayed carotid upstroke
|
|
|
What does a slow, delayed, carotid pulse indicate in the presence of a mid-late systolic murmur?
|
Severe aortic stenosis
|
|
|
What is the radiation pattern of the murmur produced by aortic valve stenosis?
|
Radiates to the right clavicle or into the carotid arteries
|
|
|
What four findings almost prove that a pt has significant aortic stenosis?
|
1. mid-late systolic murmur
and at least three of these findings: 2. Loudest in 2nd RICS 3. slow carotid upstroke 4. reduced carotid volume 5. decreased intensity of S2 |
|
|
What effect does aortic stenosis have on the LV?
|
Causes pressure overloading of the LV, concentric LV hypertrophy and a sustained apical impulse
|
|
|
What causes the aortic stenosis murmur to decrease by one grade?
|
The murmur decreases by one-grade during the straining phase of the valsalva maneuver
|
|
|
What is HOCM? What characteristics of the LV are present in pts w/ HOCM?
|
A hereditary cardiac dz characterized by asymmetric concentric LV hypertrophy and sub-valvular stenosis of the aortic outflow tract at the level of the mitral valve and interventricular septum
|
|
|
What is the mechanism by which HOCM creates a murmur?
|
The hypertrophied interventricular septum make contract w/ the anterior leaflet of the mitral valve, partly obstructing the LV outflow tract during systole. The partial obstruction creates a systolic pressure gradient b/e the distal LV cavity and the proximal LV cavity. This pressure gradient produces turbulent flow.
|
|
|
What murmur is caused by HOCM?
|
A mid-late midsystolic murmur similar to the murmur produced by aortic stenosis
|
|
|
Where is the HOCM murmur loudest?
|
The HOCM murmur is loudest at the cardiac apex and sometimes along the mid to lower left sternal border, it is audible with either the bell or diaphragm of the stethoscope
|
|
|
What causes the HOCM murmur to increase in intensity?
|
The HOCM murmur increases in intensity by one grade whenever the LV cavity becomes smaller (during the straining phase of the valsalva maneuver or after standing up from a recumbent position)
|
|
|
What dz is predicted by a midsystolic murmur that increases one grade in intensity during the straining phase of the valsalva maneuver?
|
HOCM
|
|
|
When does the intensity of HOCM decrease?
|
The HOCM murmur decreases in intensity by one grade whenever the LV cavity becomes larger (during passive leg elevation or while squatting like a baseball catcher)
|
|
|
What dz is strongly predicted by a midsystolic murmur that decreases in intensity whenever the pts legs are raised passively?
|
HOCM
|
|
|
Does the HOCM murmur show extrasystolic potentiation?
|
Maybe, sometimes yes sometimes no
|
|
|
What is the pulse abnormality produced by HOCM? what carotid pulse abnormality is produced?
|
The carotid pulse is brisk (not delayed) and the pulse may exhibit a bisferiens contour
|
|
|
How can you tell the murmur produced by HOCM from the murmur produced by aortic stenosis?
|
A pt w/ a mid-late midsystolic murmur caused by HOCM will be loudest at the apex, will increase in intensity during the valsalva maneuver, and decrease in intensity during passive leg raising.
A pt w/ a mid-late midsystolic murmur caused by aortic stenosis will have the murmur loudest in the second RICS, and decreases in intensity during the straining phase of the valsalva maneuver |
|
|
What murmur is produced by pulmonic valve stenosis?
|
A diamond-shaped mid-late midsystolic murmur that is loudest in the 2nd/3rd LICS. The murmur is usually less intense than the murmur produced by Aortic stenosis
|
|
|
When does the midsystolic murmur produced by pulmonic stenosis peak?
|
In mid-late systole, the later it peaks the more severe the stenosis
|
|
|
Where does the murmur produced by pulmonic stenosis radiate to?
|
Does NOT radiate into the carotid arteries or to the clavicle, it is audible w/ either the bell or the diaphragm
|
|
|
What effect does pulmonic stenosis have on the right ventricle? what effect does this have on JVP? cardiac impulse?
|
Pu stenosis creates a pressure overload in the RV that causes concentric ventricular hypertrophy. This causes a Giant "a" wave on JVP and a sustained RV impulse in the lower left sternal border
|
|
|
What other sounds besides the murmur are produced by pulmonic stenosis?
|
Wide physiologic splitting of S2 and an ejection sound at the upper left-sternal border that DECREASES in intensity during inspiration
|
|
|
What happens to RVEDP during inspiration in a hypertrophied RV?
|
RVEDP rises b/c during inspiration venous return to the right heart increases. BUT b/c the ventricle is hypertrophied it has decreased compliance SO RVEDP increases b/c the ventricle cannot accomodate the increased pressure as well
|
|
|
When does the murmur of pulmonic stenosis increase in intensity?
|
Increases one-grade in intensity during maneuvers that increase venous return to the right heart (during inspiration and passive leg elevation)
|
|
|
What are the characteristics of holosystolic murmurs?
|
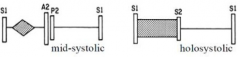
They begin w/ S1, end w/ S2 and occupy the entire duration of systole
|
|
|
What are the frequency characteristics of holosystolic murmurs?
|
They tend to be more constant throughout the entire systolic interval
|
|
|
Do holosystolic murmurs have postextrasystolic potentiation? why?
|
NOPE, b/c the increased SV that occurs w/ the beat following an interruption in the cardiac rhythm is distributed b/e the two outflow tracts: the normal anterograde outflow tract and the abnormal outflow tract
|
|
|
What is the murmur caused by chronic mitral regurgitation?
|
A holosystolic murmur that is loudest at the apex and radiates to the left axilla
|
|
|
What causes the murmur in chronic mitral regurgitation?
|
Caused by failure of the mitral valve leaflets to close tightly during ventricular systole as a result ventricular contraction forces retrograde flow from the high-pressure ventricle into the low pressure atrium which creates turbulence and generates a holosystolic murmur throughout systole
|
|
|
What causes the chronic mitral regurgitation murmur to increase in intensity?
|
When systemic vascular resistance increases (through handgrip exercises or transient arterial occlusion)
|
|
|
What causes the chronic mitral regurgitation murmur to decrease in intensity?
|
When systemic vascular resistance decreases (vasodilators) and during the straining phase of the valsalva maneuver
|
|
|
What other heart sounds are affected by chronic mitral regurgitation besides the murmur?
|
wide physiologic splitting of S2: b/c the duration of LV ejection is shorter than normal due to the presence of two LV outflow tracts essentially
S3: b/c of rapid LV filling which indicates SEVERE mitral regurg |
|
|
What impulse is generated by chronic mitral regurgitation?
|
A hyperdynamic apical impulse that is displaced down and to the left, due to eccentric LV dilation
|
|
|
What murmur is produced by tricuspid regurgitation?
|
A low-grade holosystolic murmur that is loudest in the 4th and 5th LICS adjacent to the sternum
|
|
|
What is the radiation pattern of the murmur produced by tricuspid regurgitation?
|
Radiates toward the xiphoid
|
|
|
What causes the murmur of tricuspid regurgitation to increase in intensity?
|
Inspiration and passive leg elevation
|
|
|
What detectable symptoms does chronic tricuspid regurg cause?
|
Giant V-waves on JVP and the ear and liver may pulsate w/ each heart beat
|
|
|
What murmur is caused by a VSD?
|
A harsh, grade 2-4 holosystolic murmur (often a systolic murmur w/ a palpable thrill) that is loudest at the left sternal border in the 4th and 5th LICS
|
|
|
What other heart sounds are associated w/ a VSD besides the murmur?
|
A wide split S2: b/c LV ejection is shorter than normal and RV ejection takes longer than normal (inc. preload)
|
|
|
What impulse is generated by a VSD?
|
A hyperdynamic apical impulse that is displaced down and left b/c the blood entering the RV through the VSD returns to the LV (by flowing out to the lungs and back around)
|
|
|
What causes a late systolic murmur?
|
Valvular regurgitation through a prolapsed mitral/tricuspid valve
|
|
|
What are late systolic murmurs preceded by? when do they end?
|
They are preceded by a midsystolic click and they end w/ S2
|
|
|
What causes a late systolic murmur to increase in intensity and begin earlier in systole?
|
When the ventricular EDV decreases (during valsalva or standing up from a recumbent position)
|
|
|
What causes a late systolic murmur to decrease in intensity and begin later in systole?
|
Squatting and passive leg elevation
|
|
|
What causes a late systolic murmur to only become softer?
|
When vascular resistance to ventricular ejection decreases (like when you give a vasodilator)
|
|
|
What causes a late systolic murmur to only become louder?
|
When vascular resistance to ventricular ejection increases (like during valsalva)
|
|
|
What produces mid-diastolic filling murmurs?
|
"Rumbling Murmurs"
Produced by turbulent anterograde flow across the MV or TV valves (stenotic valves) |
|
|
What produces early diastolic murmurs?
|
"Regurgitant Murmurs"
Produced by turbulent retrograde flow across the aortic or pulmonic valves |
|
|
What effect on the left atrium does mitral stenosis have? how does this produce a murmur?
|
Limits left atrial emptying and raises left atrial pressure. Flow from the high pressure atrium into the lower pressure left ventricle during ventricular diastole creates turbulence and produces a low-pitched mid-diastolic murmur
|
|
|
What is the grade/quality of the mitral stenosis murmur? what part of the stethoscope can you use to detect it?
|
It is a low-pitched murmur that is rumbling in quality; grade 1-2 in intensity and can only be detected w/ the bell of the stethoscope
Loudest at the apex |
|
|
When does the mitral stenosis murmur begin? end? how does it change?
|
Begins immediately after an opening snap and is loud, then becomes soft in mid-diastole, then gets loud in late diastole again and ends w/ S1
|
|
|
What causes the mitral stenosis murmur to get louder in late diastole?
|
Atrial contraction forces more blood through the stenotic valve
|
|
|
What causes the mitral stenosis murmur to increase in intensity in late diastole?
|
Presystolic accentuation
|
|
|
What affect does atrial fibrillation have on mitral stenosis murmurs?
|
A-fib causes presystolic accentuation to disappear in mitral stenosis murmurs
|
|
|
What accentuates the mitral stenosis murmur?
|
Passive leg elevation and turning the pt into the left lateral decubitis position
|
|
|
What increases the intensity of the mitral stenosis murmur? why?
|
Arterial vasodilators decrease systemic vascular resistance which increases the intensity of the murmur by lowering LV EDV (and inc. the pressure gradient)
|
|
|
What other heart sounds are associated w/ mitral stenosis besides the murmur?
|
An opening snap from the stenotic valves and an S1 that is increased in intensity
|
|
|
What other pathologies are caused by mitral stenosis?
|
Pulmonary HTN and concentric RV hypertrophy
|
|
|
What affect does mitral stenosis have on the cardiac impulse?
|
produces a sustained left parasternal impulse that occurs synchronously w/ the apical impulse, the apical impulse is normal
|
|
|
What murmur is produced by tricuspid stenosis?
|
A low-grade, low-pitched murmur at the lower left sternal border
|
|
|
What causes the TV stenosis murmur to increase in intensity?
|
Inspiration and passive leg elevation (b/c of inc. venous return)
|
|
|
What other ways can you use to detect tricuspid stenosis besides the murmur?
|
Giant A waves and a slow y descent
|
|
|
What causes the chronic aortic regurg murmur?
|

Retrograde flow through a incompetent aortic valve during left ventricular diastole. This produces a high-pitched early diastolic murmur.
|
|
|
What part of the stethoscope do you use to detect chronic aortic regurgitation?
|
It is so high-pitched that it can only be heard w/ the diaphragm
|
|
|
What position should the patient be in, in order to detect the chronic aortic regurg murmur?
|
The murmur is typically inaudible unless the pt is sitting upright and leaning forward after a full exhalation.
|
|
|
How can you increase the intensity of the aortic regurgitation murmur? decrease?
|
By increasing systemic vascular resistance (handgrip exercise or squatting) and you can decrease it by decreasing systemic vascular resistance (arterial vasodilators)
|
|
|
What other pulse abnormalities would you find in a pt w/ chronic aortic regurgitation?
|
1. Wide pulse pressure (>50% BPsys or >60mmHg diff.)
2. Waterhammer pulse and bisferiens pulse |
|
|
What specific pulse pressures indicate significant aortic regurgitation is present?
|
A pulse pressure > 80mmHg and BPdias < 50mmHg
|
|
|
What is a quincke pulse? what is it diagnostic of?
|
A visible "to-and-fro" pulsation in the proximal fingernail bed: dx'es chronic aortic regurgitation
|
|
|
What is a DeMusset Sign? What does it dx?
|
Bobbing of the head w/ each heartbeat. Dx'es chronic aortic regurgitation.
|
|
|
What is a lighthouse sign? What does it dx?
|
Alternate flushing and blanching of the face. Dx'es chronic aortic regurgitation.
|
|
|
What is Muller's Sign? what does it dx?
|
Pulsation of the uvula. Dx'es chronic aortic regurgitation.
|
|
|
What is Becker's sign? what does it dx?
|
Pulsation of the retinal arterioles. Dx'es chronic aortic regurgitation.
|
|
|
What do DeMusset's sign, lighthouse sign, Muller's sign and Becker's sign all reflect?
|
LARGE LV SV and rapid diastolic run-off
|
|
|
What is Duroziez's sign? what does it dx?
|
A bruit w/ systolic and diastolic components that occur in the femoral artery when pressure is firmly applied just proximal to the stethoscope. Dx'es chronic aortic regurgitation.
|
|
|
What is Ewart sign? what does it dx?
|
Dullness to percussion, increased tactile fremitus and egophany at the lower tip of the left scapula. Indicates lung compression by the massively dilated LV. Dx'es chronic aortic regurgitation.
|
|
|
What is Hill sign? what does it dx?
|
A foot-arm BP difference > 60mmHg. Indicates the presence of significant regurgitation.
*The normal foot-arm BP difference is 12mmHg +/- 2 |
|
|
What affect does chronic aortic regurg have on the impulse?
|
Apical impulse is hyperdynamic and displaced down and to the left b/c of LV dilation
|
|
|
What other heart sounds accompany the murmur caused by chronic aortic regurg?
|
1. A midsystolic murmur occurs in the absence of aortic stenosis due to the large LV SV that is ejected across the AV.
2. Austin-Flint murmur |
|
|
What is a austin-flint murmur? When does it occur? Where do you hear it? what causes it?
|
A low-pitched mid-diastolic murmur that occurs w/ chronic aortic regurg. You can hear it at the apex when the regurgitant stream impinges on the anterior leaflet of the mitral valve and partially closes it.
*Basically creates a functional mitral stenosis |
|
|
How can you tell a austin-flint murmur from mitral stenosis's murmur?
|
Arterial vasodilators decrease the intensity of the austin-flint murmur by reducing the amount of regurgitant flow, in mitral stenosis vasodilators increase the intensity of the mid-diastolic murmur
|
|
|
What murmur is indicated by the combination of a S3 w/ a mid-diastolic murmur?
|
Austin-flint
|
|
|
What is the murmur created by PV regurg?
|
A low-pitched early diastolic murmur that is heard w/ either the bell or the diaphragm in the 2nd/3rd LICS
|
|
|
What causes the PV murmur to increase/decrease in intensity?
|
Increases one grade in intensity during inspiration and passive leg elevation; which both increase venous return.
|
|
|
What murmur does pulmonary HTN cause?
|
An early diastolic murmur that is higher pitched than the murmur of valvular pulmonic regurgitation. (Graham-Steele murmur)
|
|
|
What is the Graham-Steele murmur? what does it dx?
|
A high-pitched murmur that is only audible w/ the diaphragm. It dx'es pulmonary HTN.
|
|
|
What murmur is created by a ASD? what causes it?
|
1. A midsystolic murmur that is heard in the 2nd LICS caused by increased anterograde flow across the pulmonic valve.
2. A low-pitched mid-diastolic murmur at the lower left sternal border caused by increased anterograde flow across a normal TV valve. 3. Wide fixed splitting of S2 |
|
|
What murmur is created by a PDA?
|
A "continuous murmur" that has components in systole and diastole. The murmur sounds very machine-like.
|
|
|
What is a machinery murmur? what does it dx?
|
A continuous murmur that dx'es a PDA
|
|
|
Where is the machinery murmur loudest?
|
In the 2nd LICS but is also prominent in the left infraclavicular area.
|
|
|
What position should the pt be in to hear a PDA murmur?
|
The murmur may only be audible when the pt is recumbent.
|
|
|
What other heart sounds are associated w/ a PDA besides the murmur?
|
S2 is singly or paradoxically split.
|
|
|
What is pericardial friction rub?
|
When the visceral and parietal layers of the pericardium rub together during pericardial inflammation (pericarditis)
|
|
|
What alleviates the pain from a pericardial friction rub?
|
When the pt leans forward.
|
|
|
What part of the stethoscope should be used to listen to a pericardial friction rub?
|
The diaphragm
|
|
|
What are the three components of a pericardial friction rub?
|
1. Systolic component
2. Early diastolic component 3. Late diastolic component |
|
|
What produces the systolic component of a pericardial friction rub?
|
Ventricular contraction
|
|
|
What produces the early diastolic component of a pericardial friction rub?
|
Ventricular filling
|
|
|
What produces the late diastolic component of a pericardial friction rub?
|
Atrial contraction. The late diastolic component is absent during Atrial fibrillation
|
|
|
What can cause the late diastolic component of a pericardial friction rub to be absent?
|
Atrial fibrillation
|
|
|
Where is the pericardial friction rub loudest? when does it increase in intensity?
|
Loudest at the mid-left sternal border and increases in intensity when the pt leans forward or is prone.
|
|
|
What are all innocent murmurs accompanied by? What is the timing of all innocent murmurs?
|
All innocent murmurs are midsystolic in timing except the venous hum. All innocent murmurs are accompanied w/ a S2 that exhibits normal physiologic splitting.
|
|
|
What innocent murmur is NOT midsystolic in timing?
|
The venous hum.
|
|
|
What is the "venous hum"
|
A innocent, continuous, murmur that is very common in school-age children.
|
|
|
Where is the venous hum loudest?
|
Loudest just above the sternal end of the clavicle when the pt is sitting upright.
|
|
|
What causes the venous hum?
|
Turbulent flow through the internal jugular vein resulting from jugular compression by the transverse process of the atlas.
|
|
|
What causes the venous hum to increase/decrease in intensity?
|
Increase: When the pt turns their head away from the side being examined.
Decrease: Murmur can be eliminated by manually compressing the jugular veins on the side being examined. |
|
|
What is a Still's murmur?
|
The most-common innocent murmur in children. Is midsystolic in timing and has a vibratory quality.
|
|
|
What causes the Still's murmur?
|
Periodic vibrations of anomalous chordae tendinae connected to the mitral valve.
|
|
|
Where is still's murmur loudest? What is it's quality?
|
Loudest along the lower left sternal border or apex. it is NEVER louder than 3/6.
|
|
|
What position should the pt be in to listen to a still's murmur?
|
Loudest during a recumbent position and diminishes in intensity or disappears altogether during standing.
|
|
|
What is a supraclavicular arterial murmur?
|
A innocent murmur that is midsystolic and that begins shortly after S1 and occupies less than half of systole.
|
|
|
What produces the supraclavicular arterial murmur?
|
Ejection of blood into the large arteries of the aortic arch.
|
|
|
Where is the intensity of the supraclavicular arterial murmur greatest? weakest?
|
Maximal above the clavicles and tends to be louder on the right. Hyperextension of the shoulders toward the back decreases or abolishes the supraclavicular murmur.
|
|
|
What can cause the intensity of left-sided S3 and S4 to be increased?
|
Moving the pt into the left-lateral decubitis position.
|
|
|
What position should the pt be in to listen to the murmur of mitral stenosis?
|
Left-lateral decubitis position.
|
|
|
What effect does standing have on murmurs? What murmurs are NOT effected by standing?
|
Standing decreases venous return and ventricular filling, so it decreases all murmurs EXCEPT mitral/tricupsid prolapse and HOCM.
|
|
|
What effect does squatting have on murmurs?
|
Causes abdominal compression that increases venous return and femoral artery compression that increases LV afterload.
|
|
|
What murmurs are increased by squatting? decreased?
|
Squatting increases the murmurs of chronic mitral/aortic regurgitation and decreases the murmurs of HOCM and MV prolapse.
|
|
|
What effect does inspiration have on the heart?
|
Increases venous return to the right atrium and ventricle and decreases resistance to RV ejection.
|
|
|
What effect does inspiration have on murmurs?
|
Inspiration increases the intensity of all sounds and murmurs that originate from the right heart EXCEPT the pulmonic ejection sound.
|
|
|
What position causes respiratory changes in heart sounds to be greatest?
|
When the pt is upright, they can be imperceptible when the pt is recumbent.
|
|
|
What affect on murmurs does isometric exercise (repeated handgrip) have?
|
Increases LV afterload and the intensity of left-sides regurgitant murmurs (mitral and aortic regurgitation).
|
|
|
What effect does the valsalva maneuver have on the heart?
|
Decreases venous return to the left and right ventricles.
|
|
|
What effect on heart murmurs does the valsalva maneuver have?
|
Decreases the intensity of all left-sided murmurs EXCEPT HOCM and MV prolapse.
|
|
|
What pt maneuver can provoke an MI?
|
Valsalva in pts who have severe CAD.
|
|
|
What effect on heart sounds does transient arterial occlusion have?
|
Increases the intensity of all left-sided regurgitant murmurs.
*performed by inflating bilateral BP cuffs to 20-40 mmHg above BPsys. |
|
|
What effect do arterial vasodilators have on heart sounds?
|
Increase murmur intensity of Aortic stenosis and decrease murmur intensity of chronic aortic regurgitation and chronic mitral regurgitation.
|

