![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
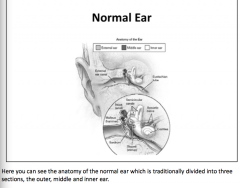
Review the anatomy of the normal ear. |
|
|
|
Draw the pathway of sound conduction |

Sound waves propagate in the air, enter the external auditory canal and bounce off the tympanic membrane like a trampoline. Set into motion, the tympanic membrane moves the malleus, incus and stapes. Movement of the stapes footplate changes the pressure in the fluid-filled inner ear and that triggers a traveling wave in the basilar membrane of the cochlea. Hearing can also occur by bone conduction when the sounding source, such as a vibrating tuning fork, is in contact with the bones of the skull resulting in their vibration. When the sound is transmitted through air or bone, the traveling wave in the basilar membrane moves from the base to the apex of the cochlea. |
|
|
Inside the cochlea, hair cells with _____ are found in the organ of Corti, which rests on the _____ membrane. These hair cells are in contact with the tectorial membrane and are deformed by the traveling wave of sound. High frequency tones maximally displace the basilar membrane near the base of the _____. As the frequency of the sound decreases, the point of maximal membrane displacement moves toward the _____ apex. The distortion of the stereocilia on the hair cells causes _____ of the cell and that results in increased electrical activity along the auditory nerve. |
Inside the cochlea, hair cells with stereocilia are found in the organ of Corti, which rests on the basilar membrane. These hair cells are in contact with the tectorial membrane and are deformed by the traveling wave of sound. High frequency tones maximally displace the basilar membrane near the base of the cochlea. As the frequency of the sound decreases, the point of maximal membrane displacement moves toward the cochlear apex. The distortion of the stereocilia on the hair cells causes depolarization of the cell and that results in increased electrical activity along the auditory nerve. |
|
|
|
|
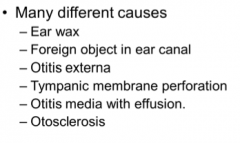
What are these all causes of? |
Conductive hearing loss
Transmission of sound through the air blocked. |
|
What are these all causes of?
What is primarily damaged? |
Sensorineural hearing loss
Damage to hair cells in the organ of Corti. |
|
|
Sensorineural hearing loss arises principally from damage to hair cells in the ______. This can occur following a very loud noise, viral infection, ototoxic medication, fractures of the temporal bone and Ménière's disease. It can be a congenital problem and commonly occurs with advancing _____. _____ refers to age-related hearing loss that is gradually progressive and involves mostly high frequency sounds. Drug induced ototoxicity occurs with aminoglycoside antibiotics such as gentamicin, but can also occur with Lasix, salicylates, quinine and cancer drugs such as cisplatin. Sensorineural hearing loss occurs with acoustic neuroma and other tumors of the ______ angle that compress the auditory nerve. Theoretically hearing loss can also occur with stroke, demyelination, trauma or any other structural disease affecting the central auditory pathways. However, hearing loss is _____ often seen with disease of the brain parenchyma because the central auditory pathways cross over at many way-stations along their journey to the medial geniculate nucleus of the thalamus and ultimately to Heschl's gyrus. This redundancy in neural circuitry helps to protect the individual from gross lateralizing hearing loss which is not the case for other sensory systems such as vision, pain and temperature. Occasionally one does find hearing loss in multiple sclerosis patients with brainstem plaques. |
Sensorineural hearing loss arises principally from damage to hair cells in the organ of Corti. This can occur following a very loud noise, viral infection, ototoxic medication, fractures of the temporal bone and Ménière's disease. It can be a congenital problem and commonly occurs with advancing age. Presbyacusis refers to age-related hearing loss that is gradually progressive and involves mostly high frequency sounds. Drug induced ototoxicity occurs with aminoglycoside antibiotics such as gentamicin, but can also occur with Lasix, salicylates, quinine and cancer drugs such as cisplatin. Sensorineural hearing loss occurs with acoustic neuroma and other tumors of the cerebellar pontine angle that compress the auditory nerve. Theoretically hearing loss can also occur with stroke, demyelination, trauma or any other structural disease affecting the central auditory pathways. However, hearing loss is less often seen with disease of the brain parenchyma because the central auditory pathways cross over at many way-stations along their journey to the medial geniculate nucleus of the thalamus and ultimately to Heschl's gyrus. This redundancy in neural circuitry helps to protect the individual from gross lateralizing hearing loss which is not the case for other sensory systems such as vision, pain and temperature. Occasionally one does find hearing loss in multiple sclerosis patients with brainstem plaques. |
|
What are these all causes of? |
Mixed hearing loss |
|
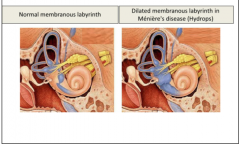
Which is a normal membranous labyrinth? Which is dilated membranous labyrinth from Meniere's disease? |
|
|
|
Ménière's disease produces vertigo, fluctuating _____ hearing loss and ____. Decreased resorption of endolymphatic fluid causes fluid build-up or _____ with high pressure, bowing and subsequent rupture in the membranes separating the endolymph from the _____. The two fluids have very different compositions and their mixture produces a sudden change in vestibular cochlear pressure and in their electrical firing properties. Attacks can last 30 minutes to several hours, until _____ is reestablished. The next slide shows a cartoon of this process. In the early stages, the symptoms remit between attacks and patients may be symptom free for a year or more. With disease progression, the hearing loss persists and gradually worsens. Tinnitus may become continuous. Treatment with a _____ diet and diuretics can be helpful. Vestibular sedatives including anticholinergics, antihistamines and benzodiazepines may be helpful when the patient is stricken with an attack. |
Ménière's disease produces vertigo, fluctuating sensorineural hearing loss and tinnitus. Decreased resorption of endolymphatic fluid causes fluid build-up or hydrops with high pressure, bowing and subsequent rupture in the membranes separating the endolymph from the perilymph. The two fluids have very different compositions and their mixture produces a sudden change in vestibular cochlear pressure and in their electrical firing properties. Attacks can last 30 minutes to several hours, until equilibrium is reestablished. The next slide shows a cartoon of this process. In the early stages, the symptoms remit between attacks and patients may be symptom free for a year or more. With disease progression, the hearing loss persists and gradually worsens. Tinnitus may become continuous. Treatment with a low salt diet and diuretics can be helpful. Vestibular sedatives including anticholinergics, antihistamines and benzodiazepines may be helpful when the patient is stricken with an attack. |
|
What is this the clinical assessment for? |
Hearing loss |
|
|
|
|
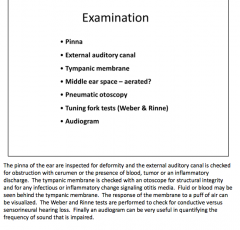
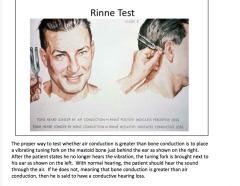
Review the Rinne test. |
|
|
|
In performing the Weber test, the vibrating tuning fork is placed on the patient's forehead. The patient is asked if the sound seems louder in one ear. If the patient has a _____ hearing loss, the sound will lateralize to that ear. You can check this for yourself by placing the tuning fork on your forehead and plugging one ear with your finger. The vibration will sound louder on the side you plugged your ear. If there is sensorineural hearing loss, the sound will be louder in the _____ (normal or abnormal) ear. In that case, however, the Rinne test will show air conduction to be greater than bone in both the normal and in the abnormal ear with the sensorineural hearing loss. |
In performing the Weber test, the vibrating tuning fork is placed on the patient's forehead. It does not necessarily have to be above the hairline as it is shown here. The patient is asked if the sound seems louder in one ear. If the patient has a conductive hearing loss, the sound will lateralize to that ear. You can check this for yourself by placing the tuning fork on your forehead and plugging one ear with your finger. The vibration will sound louder on the side you plugged your ear. If there is sensorineural hearing loss, the sound will be louder in the normal ear. In that case, however, the Rinne test will show air conduction to be greater than bone in both the normal and in the abnormal ear with the sensorineural hearing loss. |
|
Review |
|
|
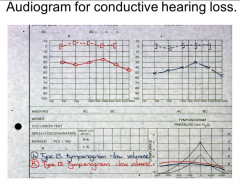
Conductive or sensorineural hearing loss? |
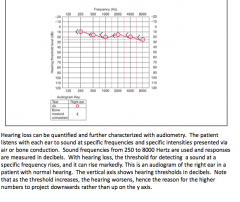
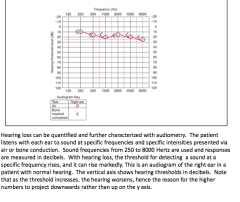
Conductive
Bone conduction greater than air
The audiometric pattern of hearing loss can be very helpful in diagnosis. Conductive hearing loss typically shows a fairly equal threshold elevation for each frequency as shown in the this slide. However, early otosclerosis can cause fixation of the footplate of the stapes and result in a greater threshold elevation in the lower frequencies. With middle ear effusions, there may be a greater elevation of thresholds in the higher frequencies. The tympanogram measures the impedance of the middle ear to sound and can be useful for the identification of middle ear effusions in children. |
|
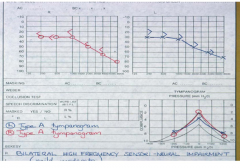
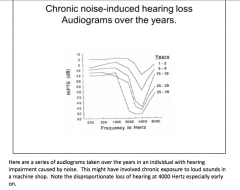
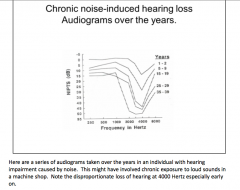
Conduction or sensorineural hearing loss? |
Sensorineural hearing loss typically shows steadily rising threshold elevations with increasing frequencies. In other words, the higher the sound frequency, the worse the hearing. However, noise-induced hearing loss often shows a selectively greater loss at 4000 Hertz when compared to higher frequencies. This is illustrated on the next slide. Another exception is Ménière's disease in its early stages. There the thresholds are elevated more in lower than in higher frequencies. In other words hearing is initially worse for sounds in the lower frequency range. |
|
|
|
|
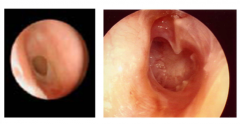
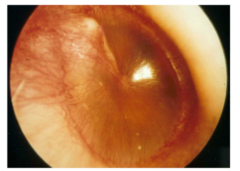
What is shown here?
What does the degree of hearing loss depend upon? |
TM perforation
Size of the hole |
|
What is happening here? |
Otitis media with effusion Very common in children |
|
|
Otosclerosis: Describe the process. What type of hearing loss? What age does it usually start? Bilateral or unilateral? Familial? What is treatment? |
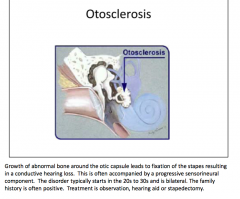
|
|
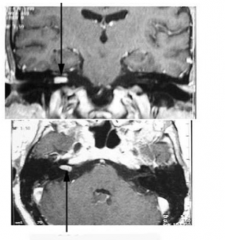
What is the arrow pointing to here?
How would this present differently if it were a meningioma? |
The arrows point to a contrast enhancing lesion in the right cerebellar pontine angle. This most often turns out to be a vestibular schwannoma, formerly called an acoustic neuroma. Meningiomas also occur in this spot. However, the patients typically present with sensorineural hearing loss and not with vertigo. The compression of the eight cranial nerve is so slow and gradual that the brain has more than adequate time for central compensation when the vestibular input decreases on one side. By blocking visual fixation and provoking the semicircular canals, one can still detect the vestibular abnormality but that is a topic covered in a separate module on vertigo. |
|
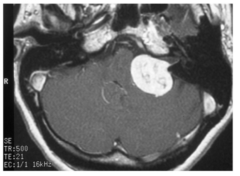
What is it compressing? What other deficits will be noted?
What is the patient at risk for due to obstruction in this area? |
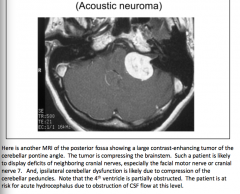
|

