![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Anencephaly
|
- the most severe form of neural tube defect;
-1 in 500 births -More common in female fetuses -Risk increase with with folate (folic acid) deficiency -babies dead at birth |
|
|
|
Spina Bifida
|
-Absence or hypoplasia of one or more of the dorsal arches of the vertebrae;
-meningeal and spinal defects possible -Spina bifida cystica may cause gait disturbance, urinary incontinence, male impotence -Spina bifida occulta: unfused vertebral arch (intact meninges and spinal cord) is common; 20% of general population and is usually symptomatic |
|
|
|
plagiocephaly
scaphocephaly trigonocephly |
-fused coronal suture
-fused saggital suture - fused metopic suture |
|
|
|
Cerebral Edema
|
Increased water content of the brain parenchyma
|
|
|
|
Vasogenic Edema
|
Disruption in blood-brain barrier that allows escape of fluid from the vasculature into the interstitial space of the brain
|
|
|
|
Cytotoxic Edema
|
An increase in intracellular fluid secondary to cellular injury
|
|
|
|
Brain Herniation
|
The displacement of a part of the brain from one dural compartment to another
|
|
|
|
Transtentorial Herniation
|
a medial displacement of temporal lobe against the tentorium cerebelli; causes pupillary dilation,
impaired eye movements, and compression of posterior cerebral artery with ischemia to visual cortex |
|
|
|
Subfalcine Herniation
|
a displacement of c. gyrus under falx cerebri caused by expansion of cerebral hemisphere; results in compression of anterior cerebral artery with ischemia to cortex and weakness/sensory abnormality of leg.
|
|
|
|
types of hernia's
|
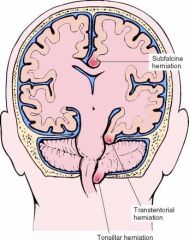
locations
|
|
|
|
ID the sutures of the crown of head
|
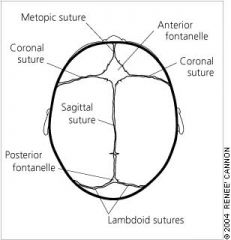
MCSP
|
MCSP
|
|
|
Tonsillar Herniation
|
displacement of the cerebellar tonsils through the foramen magnum that compresses the respiratory centers of the medulla oblongata
|
|
|
|
Hydrocephalus
|
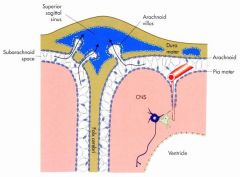
accumulation of excess cerebrospinal fluid in the ventricular system of the brain
|
|
|
|
Causes of Hydrocephalus
|
-Decreased resorption of CSF (most common)
-Overproduction of CSF -Obstruction (within ventricles, foramina of Lushka & Magendie or subarachnoid space) |
|
|
|
Communicating hydrocephalus
|
when full communication exists between the ventricles and subarachnoid space
|
|
|
|
Noncommunicating hydrocephalus
|
when CSF flow is obstructed within the ventricular system or in its outlets to the arachnoid space
|
|
|
|
Obstructive hydrocephalus
|
obstruction of the flow of CSF (intraventricular or extraventricular). Most hydrocephalus is obstructive
|
|
|
|
Vascular Diseases of the Brain
|
Generalized reduction in blood flow (hypoxic-ischemic encephalopathy)
Infarction Hemorrhage (parenchymal or subarachnoid) |
|
|
|
Causes of Hypoxic-ischemic Encephalopathy
|
Cardiac dysrhythmias
Shock Increased intracranial pressure |
|
|
|
Modifiers of Hypoxic-ischemic Encephalopathy
|
Age (younger more tolerant)
Duration (short duration “recoverable”) Temperature (hypothermia slows rate of injury) |
|
|
|
Brain Infarction
|
Most common form (70-80%) of strokes (CVA)
Of brain infarctions, about ¾ are ABI (atherothrombotic brain infarction) 7th decade; males>females Thrombosis of atherosclerotic vessel predisposes to infarction (hypertension, diabetes & smoking) Emboli (from heart or elsewhere can be a cause) |
|
|
|
Features of Brain Infarction
|
-Transient ischemic attacks precede infarct in 1/3; TIA predictive of impending infarct
-Infarcts occur most often in areas supplied by middle cerebral artery -Deficits can include visual field abnormalities, aphasia, apraxia, agnosia, contralateral hemiparesis & hemidysesthesia -Paradoxical infarct related to collateral circulation |
|
|
|
Primary Brain Parenchymal Hemorrhage
|
-Hypertension most common underlying cause (50%); other causes are coagulation disorders, amyloid, neoplasms, aneurysms, AVM (arteriovenous malformation)
-Mid-late adult life; peak at age 60 -Sudden headache, vomiting, loss of consciousness, coma, pupillary fixation, herniation, apena & death |
|
|
|
distribution of hypertensive hemorrhages
|
-65% basal ganglia thalmus
-15% Pons -10% cerebellum |
|
|
|
Types of Aneurysm
|
-medial defect (berry or saccular)
-atheroscelrotic -charcot (hypertension) |
|
|
|
Saccular (berry) Aneurysm
|
-Present at bifurcations in 1%; risk of rupture when 6-10 mm in size; women > men, <50; incidence higher in polycystic kidneys, coarctation of aorta, AVM
-If ruptured, produces subarachnoid and/or brain hemorrhage -Abrupt headache, vomiting, loss of consciousness with 50% death within days; infarction, hydrocephalus, herniation |
|
|
|
Common sites of saccular (berry) aneurysms in the circle of Willis
|
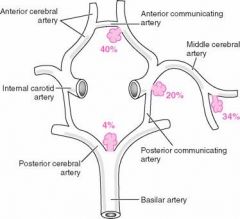
.
|
|
|
|
Arteriovenous Malformation
|
-Most common congenital vascular anomaly of the brain; usually located in the cerebral hemispheres
-Hemorrhage and seizure most likely in 1st decade -10% also have saccular aneurysm |
|
|
|
CNS Trauma
|
Epidural hematoma
Subdural hematoma Traumatic parenchymal injury |
|
|
|
Epidural Hematoma
|
-Most frequently associated with skull fracture & ruptured middle meningeal artery; blood between skull and dura
-Concussion, “ lucid interval” followed by progressive loss of consciousness -Can produce transtentorial and tonsillar herniation if not promptly treated |
|
|
|
Subdural Hematoma
|
-Most acute cases caused by disruption of bridging veins between dura & arachnoid mater; “velocity change injuries”; chronic with atrophy of brain
-Symptoms slower onset than epidural; compression of brain with possible herniation if not resorbed or treated; may be chronic (neomembrane) |
|
|
|
Traumatic Parenchymal Injury
|
Concussion
Contusion Laceration Diffuse axonal injury Traumatic intracerebral hemorrhage Generalized brain swelling |
|
|
|
contusion pattern
hit in front of head hit in back of head hit in back side of head |
-in the front
-in the front -on the opposite side of head and front |
|
|
|
Neurocutaneous Syndromes (gene associations)
|
Neurofibromatosis I (17)
Neurofibromatosis II (22) Tuberous sclerosis (9 or 16) von-Hippel-Lindau disease (3) Sturge-Weber disease (unknown) |
|
|
|
Neurofibromatosis (type I)
|
cafe au lait spots
Lisch nodules (tan or brwon spots on the iris |
|
|
|
Infection of the CNS
|
Leptomeningitis (meningitis)
Brain abscess Tuberculosis and toxoplasmosis Encephalitis (mostly viral) Spongiform encephalopathies |
|
|
|
Leptomeningitis (Meningitis)
|
-Acute (purulent); bacterial
-Acute lymphocytic; viral -Chronic; fungal, TB & neurosyphilis |
|
|
|
Evaluation of CSF
|
Protein
Cell type Glucose |
|
|
|
Brain Abscess
|
Most often bacterial
Hematogenous spread Contiguous spread Direct implantation (trauma) |
|
|
|
Viral Encephalitis
|
-Most common type of encephalitis
-Most often generalized,localized (HSV) to temporal lobe -Arbovirus, HSV, CMV, HIV, JC |
|
|
|
Prions as Agents of Disease
|
-Only known infectious agents devoid of RNA and DNA
-Manifest as infectious, sporadic or genetic diseases -Accumulation of abnormal folded form of normal prion protein -Prion conformation associated with specific disease |
|
|
|
Spongiform Encephalopathies
|
Creutzfeldt-Jacob (CJD); classic and new-variant
Kuru Gerstmann-Straussler syndrome Fatal familial insomnia |
|
|
|
CNS Neoplasms
|
-Astrocytoma
-Oligodendroglioma -Ependymoma -Primitive neuroepithelial neoplasm (medulloblastoma) |
|
|
|
CNS Neoplasms II
|
-Neuronal neoplasms (ganglioglioma, gangliocytoma, dysembryoplastic neuroepithelial tumor)
-Primary CNS lymphoma -Meningioma -Metastatic neoplasms |
|
|
|
Astrocytoma
|
-Most common of primary brain tumors; TP53 mutation thought to play a role
-Pilocytic type are slow growing; mostly in children -Fibrillary types are diffuse and can grow rapidly; “grade” determines behavior; any age; astrocytoma, anaplastic astrocytoma, glioblastoma multiforme |
|
|
|
Metastatic Neoplasms to the Brain
|
-The brain is a common site of metastasis
-Approximately 33% of all intracranial neoplasms are metastatic -Excluding leukemia and lymphoma, frequent primaries are carcinomas of lung and breast and melanoma |
|

