![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
|
Give 6 causes of anaemia |
Infections Nutritional anaemias (iron, folate, vit B12, vit A), Anaemia of chronic disease (renal failure, tb, cancer) blood loss (hookworm) haemoglobinopathies (sickle cell, thalassemia) Malignancies and bone marrow failure |
|
|
Three Cardinal features of haemolysis? |
Worsening anaemia Jaundice Dark urine (Coca-Cola) |
|
|
Lab findings in haemolysis (3) |
Falling Hb Raising unconjugated bilirubin Polychromasia/reticulocytes |
|
|
7 causes for haemolysis |
External to RBC: Septicaemia DIC Mechanical (heart valves) Cell wall associated: Antibodies (transfusion, drugs) Spherocytosis RBC disfunction: Enzymopathies Haemoglobinopathies |
|
|
What is glucose-6-phosphate dehydrogenase useful for and where is it find in highest levels |
It protects RBCs from oxidant damage. Early RBC have higher levels than older cells |
|
|
What genetic patern is G6PD deficiency linked to? |
X-linked recessive |
|
|
What is the prevalence of G6PD deficiency? |
Africa 25% (protects against malaria) Mediterranean basin 35-40% (more severe) |
|
|
Symptoms of G6PD deficiency? (Common x2, rare x2) |
Mostly asymptomatic. Causes sudden, self limiting haemolysis of variable severity. Neonatal jaundice (most common cause) Renal failure (adults >>kids) Chronic haemolysis - rare |
|
|
Triggers for acute haemolysis in G6PD deficiency? |
Infections Diet (fava beans) Stress DKA Meds (variable) including - primaquinine, pamaquine, chloroquine, hydroxychloroquine, sulfonamides, nitrofurantoin, isoniazid |
|
|
G6PD management ? |
Mostly supportive + prevention If severe - blood transfusion Splenectomy |
|
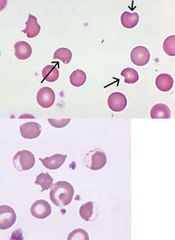
What do these films show? |
G6PD deficiency |
|
|
Symptoms of hereditary spherocytosis and ellipticytosis? |
Mostly asymptomatic Gallstones Haemolysis Anaemia |
|
|
Management of spherocytosis and ellipticytosis? |
Mostly supportive Blood transfusions (might need extended blood matching if repeat transfusions) Folate - if severe or pregnant Splenectomy - if persistently anaemic Cholecystectomy/regular gallstones check |
|
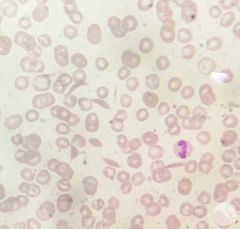
What does this film show? |
Sickle cell disease |
|
|
Give 4 clinically significant sickle cell haemoglobinopathies |
Hb SS - most severe Hb SC - milder form Hb S beta thalassemia (HbS thal) - one gene S and one gene thal. Hb SD, HbSE and HbSO - rare, varable severity HbAS - usually assymptomatic (A is normal) -"sickle cell trait" |
|
|
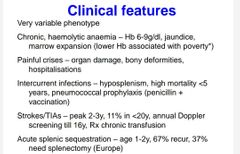
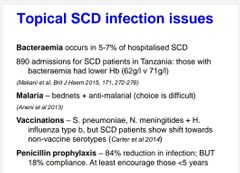
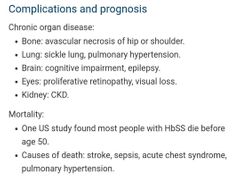
What are the chronic symptoms/features of SCD? |
- Haemolytic anaemia causes pallor, fatigue, jaundice - Chronic pain - Painful dactylitis - painful swelling of the hands and feet (often at 6-8months, rare >2y/o) - Failure to thrive - Splenomegaly - Gallstones (from chronic haemoysis) - high cardiac output - systolicflow murmur, cardiomegaly |
|
|
Sickle cell crisis- give features of a vaso-occlusive crisis |
Acute painful crisis affecting bones, abdo or chest. Other presentations incl - stroke (high in children), priapism, visual floaters (leading to vision loss) |
|
|
Acute chest syndrome in a sickle cell crisis. what is it and how does it present? |
vaso-occlusion +/- infection in lungs. common in kids. pnumonia like presentation with (pleuritic) chest pain, cough, SOB, fever, crackles and tender ribs |
|
|
5 ways to diagnosis SCD |
Family history Clinical features Blood film Sickle screen Haemoglobinelectrophoresis |
|
|
How to manage the anaemia in SCD? |
RBC transfusion when Hb falls under pt's personal baseline consider lifelong folate. need high dose in pregnancy |
|
|
How to manage the pain in SCD? |
Analgesia (opioids, NSAIDs,) – control pain within 60-90 minutes of admission Fluids, oxygen, treat underlying infections |
|
|
Main SCD drug? How does it work? |
Hydroxycarbamide (/hydroxyurea) Hydroxycarbamide increases Hb F (increased NO, reduced WBC andplatelets, end organ protection) Outcomes: less crises, transfusions, chest syndromesand hospital stay. No effect on death, stroke orsequestration. |
|
|
When would chronic/exchange transfusions be recomended in SCD? |
Aim to reduce Hb S% to <30% Data support use for: • primary prevention of stroke • secondary prevention of silent cerebral infarcts in children • preventing recurrent strokes in children. |
|
|
|
|

|
|

