![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
types of haemoglobin
|
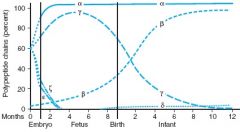
zeta/epsilon - early embryonic period
alpha/gamma - fetal period, gamma is dominant (HbF = a2g2) alpha/beta - perinatal period |
|
|
major Hbs in adults and children > 6mo
|
HbA (a2b2)
HbA2 (a2d2) |
|
|
populations at risk for thalassaemia
|
Mediterranean
Middle Eastern African Indian |
|
|
classification of thalassamia
|
1. Beta or alpha
2. 3beta types: minor (heterozygous), major (homozygous), intermedia (homozygous) 3. Four alpha types: silent carrier (a-/aa), alpha-thal trait (a-/a-), HbH (--/a-), Hb Barts (--/--, hydrops fetalis with g4, b4, Hb Portland (zeta2gamma2)) |
|
|
what is HbH
|
--/a-
excess beta chain results in formation of HbH (beta4) 15-30% Hb Barts (gamma4) in neonatal period |
|
|
what is HbBarts
|
--/--
> 75% Hb Barts = gamma4 |
|
|
what is HbPortland
|
zeta2gamma2, found in Hb Barts disease
|
|
|
what pattern of inheritance is found in thalassaemia?
|
Mendelian - recessive
|
|
|
how many genes are there for beta and alpha globins respectively?
|
beta - 2 genes, on chromosome 11
alpha - 4 genes, on chromosome 16 |
|
|
what is the pathophysiology of beta thalassaemia?
|
point mutations or deletions in one or two genes for beta globin production --> reduced or absent beta globin production
|
|
|
beta thalassaemia minor (heterozygous for b0 or b+) - symptoms
|
usually asymptomatic, usually incidental finding of mild anaemia
lethargy, fatigue, dyspnoea |
|
|
beta thalassaemia minor - signs
|
often normal examination
pallor splenomegaly |
|
|
beta thalassaemia minor - investigations
|
FBC: reduced Hb
Film: mild microcytic hypochromic anaemia occasional target cells Elevated HbA2 |
|
|
what are target cells?
|

relative membrane excess
in thalassaemia, it's due to deficiency of haemoglobin |
|
|
IDA vs beta thalassaemia
|
may co-exist
IDA may mask beta-thalassaemia, preventing Dx until it is corrected |
|
|
what is Cooley anaemia?
|
beta thalassaemia major (homozygous)
|
|
|
what are the two types of beta thalssaemia major?
|
B0 = no beta globin chains
B+ = insufficient beta chains |
|
|
what is the pathophysiology of Cooley anaemia?
|
excess alpha chains precipitate --> shortened red cell survival & destruction within BM and spleen
|
|
|
when do children with beta thalassaemia major (Cooley anaemia) present?
|
between 3 months and 1 year
|
|
|
beta thalassaemia major - presentation
|
pallor
hepatosplenomegaly mild jaundice later (4-5y): skin pigmentation, frontal bossing, malar prominence |
|
|
why does frontal bossing and malar prominence develop in beta thalassaemia major?
|
expansion of bone marrow after ineffective erythropoeisis
|
|
|
beta thalssaemia major - investigation findings
|
Hb - very low
Film - microcytic, hypochromic RBCs, stippled RBCs, macrocytes, target cells, nucleated red cells HbF (a2g2) - elevated HbA2 - elevated |
|
|
how to differentiate between B+ and B0 thalassaemia
|
globin chain synthesis studies
|
|
|
long term sequelae of untreated beta thalassaemia major
|
severe chronic anaemia --> growth retardation, increased iron resorption (skin pigmentation)
extramedullary haematopoesis --> hepatosplenomegaly, abdo distension bone marrow expansion --> frontal bossing, maxillary hypertrophy, cortical thinning of lone bones + fractures |
|
|
why does increased skin pigmentation develop in severe beta thal major?
|
increased iron resorption
|
|
|
from which conditions does death usually occur in beta thal major?
|
cardiac failure
arrythmias infections (iron has toxic effects on myocardium) |
|
|
management of beta thal major
|
transfusions q3-4 weekly
can do a BM or umbilical cord blood transplant if there is an HLA-identical sibling donor. If performed prior to development of hepatomegaly or portal fibrosis, there is a >90% cure rate |
|
|
to which organs is iron toxic (and what are the consequences)
|
myocardium - arrythmias, cardiac failure
pancreas - diabetes liver - fibrosis gonads - infertility |
|
|
how are iron chelators administered
|
subcut infusion over 10 hours, usually overnight
|
|
|
what is an iron chelator
|
binds free iron, so it is excreted in urine
|
|
|
what alternatives to chelation are available to reduce iron loading?
|
erythrocytapheresis
|
|
|
what supplements do patients with beta thal major require?
|
folic acid
|
|
|
what vaccinations are required for pts with beta thal major
|
HBV
give vaccines prior to splenectomy against encapsulated organisms (Hib, S. pneumoniae, N. meningitides) |
|
|
HbE - spectrum of disease
|
homozygous/heterozygous - asymptomatic
doubly heterozygous with beta-thal --> similar to thalassaemia major |
|
|
HbE - diagnosis
|
FBC + film
Haemoglobin electrophoresis |
|
|
what are the two groups of haemoglobinopathies?
|
1. thalassaemias - quantitative deficiency in globin chains
2. structural abnormalities of globins: HbS, HbC, HbE |
|
|
what is the underlying cause of HbS, HbC, HbE?
|
point mutations & single AA substitutions in beta globin
|
|
|
when does HbA become predominant over HbF?
|
2-4 months age
|
|
|
why are alpha thalassaemias manifest in the newborn, unlike beta thalassaemias?
|
because alpha chains are required for both fetal (HbF) and adult (HbA, HbA2) haemoglobins
|
|
|
when do beta thalassaemia and sickle cell disease begin to manifest?
|
after 3-4 months age, when HbF has declined substantially
|
|
|
where are the alpha-globin genes located?
|
chromosome 16
|
|
|
what is the difference in patterns of alpha-thalassaemia between Africans and Asians?
|
Africans more likely to be silent carriers or have alpha-thal trait
Asians more likely to have the full spectrum of disease - implications for genetic counselling |
|
|
what are the types of alpha-thalassaemia
|
one gene deletion --> silent carrier (0-3% Hb Barts, gamma4)
-/aa or -a/-a --> alpha-thal trait (2-10% HbBarts) -/-a --> HbH disease (HbH = beta4) (15-20% HbBarts) --.-- --> hydrops fetalis, >75% HbBarts |
|
|
aa/a- clinical manifestations + Ix
|
asymptomatic, normal Hb, normal MCV
neonatal Hb electrophoresis: HbBarts 0-3% |
|
|
-a/aa or -a/-a clinical + lab manifestations
|
Slight reduction in MCV and Hb level, mild hypochromia
2-10% Hb Barts on eletrophoresis in neonatal period |
|
|
--/-a clinical + lab manifestations
|
this is Haemoglobin H disease. HbH = beta4 chains, with 15-20% Hb Barts present during neonatal period.
Mod-severe microcytic haemolytic anaemia Hepatosplenomegaly Bony abnormalities Jaundice High retics Hypochromic, microcytic RBCs Poikilocytosis Basophilic stippling |
|
|
How is HbH identified on microscopy?
|
brilliant cresyl blue stain --> shows inclusion bodies formed by denatured HbH
|
|
|
--/-- clinical + lab manifestations
|
hydrops fetalis
>75% Hb Barts on electrophoresis absence of normal fetal or adult Hb intrauterine anaemia, fetal demise or death after delivery massive hepatosplenomegaly |
|
|
DDx of alpha-thal trait (two deletions)
|
beta thal minor (will have abnormal Hb eletrophoresis, with insufficient HbA, whereas alpha-thal trait will have normal Hb eletrophoresis)
IDA (thalassaemias have normal or increased serum iron and ferritin) |
|
|
DDx of HbH disease (--/a-)
|
most other haemolytic anaemias have normal MCV and normal colour
HbH will have microcytic, hypochromic red cells, plus all the other features of haemolysis (hepatosplenomegaly, jaundice, high retics, nucleated red cells etc.) |
|
|
DDx of hydrops fetalis
|
other causes of hydrops due to anaemia, e.g. alloimmunisation
|
|
|
Treatment of alpha thalassaemia
|
alpha-thal trait (aa/a-): no Rx
HbH: folic acid, avoid oxidant drugs (as in G6PD). beware infections. consider splenectomy later. Genetic counselling |
|
|
which thalassaemias can be detected on neonatal screening?
|
only the alpha thalassaemias, because they affect HbF, and screening detects Hb Barts.
|
|
|
where are the beta globin genes located?
|
chromosome 11
|
|
|
what are the types of beta globin genes?
|
normal
B+ (produces insufficient beta globin) B0 (produces no beta globin) |
|
|
beta thalassaemia intermedia - clinical manifestations
|
more severe than thalassaemia minor
generally not trasnfusion dependent |
|
|
how is beta thalassaemia diagnosed?
|
haemoglobin eletrophoresis after 6-12 mo age
Shows increased HbA2 and/or HbF Homozygous B0-thalassaemia --> only HbA and HbA2 are present |

