![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back
|
CDC Diagnostic Criteria for PID |
Sexually active female with pelvic or lower abdominal pain with no other identifiable cause for illness other than PID identified
Minimum criteria (1 or more of following on pelvic): -Cervical motion tenderness -Uterine tenderness -Adenexal tenderness Supportive: -Temperature >38.3 -Cervical/vaginal mucopurulent discharge -Elevated ESR/CRP -Documented G/C on swab Definite: -Laproscopy -Biopsy proven endometritis -Transvaginal or MRI evidence of saplingitis, TOA |
|
|
Risk factors for PID
|
Young age (15-25 years of age)
Multiple sexual partners Cigarette smoking Menses Insertion of IUD within previous 3 weeks Recent uterine instrumentation African American |
|
|
Indications for Admission in PID
|
Cannot exclude surgical emergency
Prengnacy Not responding to oral therapy Not reliable for outpatient treatment Severe illness (vomitting, high fever) Tubo-ovarian abscess |
|
|
Initial treatment for PID
|
250 mg Ceftriaxone IM |
|
|
Key points to differential ulcerative STI's |
Description of lesions - single or multiple - painful or painless - Indurated or soft - Irregular or soft - Evolution Presence of Absence of adenopathy Systemic symptoms |
|
|
Most common ulcerative STI |
Genital herpes |
|
|
Primary herpes infection in patients without pre-exsisting antibodies |
Vesicles -> PAINFUL shallow multiple grouped ulcers that may coalesce
Systemic symptoms
Bilateral midly tender non fluctuant adenopathy |
|
|
DDX for ulcerative STIs |
Herpes genitalis Primary syphillis Chancroid Lymphogranuloma vereneum (LGV) Molluscum contagiosum Condyloma acuminata (genital warts) Pediculosis Scabies Pyoderma Trauma Excoriations Bechet's disease Fixed drup eruption Yeast infection
|
|
|
DDX for non-ulcerative STIs |
Gonorrhea Chlamydia Nongonoccocal urethritis Secondary or tertiary syphillis Candidal vaginitis Trichomoniasis Bacterial vaginosis Endometriosis |
|
|
Recommended diagnostic test for herpes |
PCR testing for HSV DNA
Consider serology if negative but high clinical suspicion |
|
|
Syphillis causative organism and transmission |
Treponema pallidum
A Spirochete bacterium
Transmission is via exposure of moist skin to an infected area |
|
|
Syphilis Manifestations |

|
|
|
Chancre |
Solitary, PAINLESS papule that then ulcerates
Smooth raised edge with sharply defined borders and clean base |
|
|
Non-Treponemal testing for syphillis |
VDRL (Veneral disease research laboratory) RPR (rapid plasma reagin) tests
Both are screening tests |
|
|
Treponemal/Confirmatory testing |
Microhemagglutination test for treponema pallidum (MHA-TP)
Florescent treponemal antibody absorption test (FTA-ABS) |
|
|
Lymphogranuloma verenum |
Causes by specific serotypes of Chalmyidia trachomatic
Small, PAINLESS, transient genital lesions
Followed by unilateral inguinal lymphadenitis (groove sign) mainly non fluctuant |
|
|
Chancroid |
Caused by Haemophilus ducreyi, Multiple PAINFUL genital ulcerations and inguinal bubo formation |
|
|
Criteria for "probable" diagnosis of chancroid |
(1) One or more PAINFUL genital ulcers (2) no evidence of T. pallidum infection (3) the clinical presentation typical for chancroid (4) HSV testing on the ulcer exudates are negative. |
|
|
Granuloma inguinale (donovanosis) |
Caused by Klebsiella granuomatis
Chronic, PAINLESS, progressive ulcerative lesions on the genitalia or perineum
Irregular, clean-based granulomatous ulcers that are highly vascular (giving the classic “beefy red appearance”)
|
|
|
CONDYLOMATA ACUMINATA |
Anogenital warts causes by HPV |
|
|
Characteristics of ulcerative STIs |
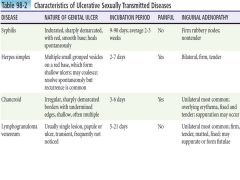
|
|
|
Most common STI |
Chlamyidia |
|
|
Causes of nongonococcal urethritis other than chlamyidia |
Ureaplasma urealyticum Haemophilus vaginalis Mycoplasma genitalium |
|
|
Disseminated gonococcal infections |
Causes by gonococcal bacteremia
More common in woman
Characterized by arthritis-dermaitis syndrome |
|
|
Characteristics of vulvovaginitis by cause |
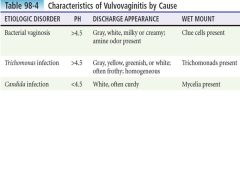
|
|
|
Trichomoniasis |
Causes by flagellated protozoan -> Trichomonas vaginalis
|
|
|
Bacterial vaginosis |
Shift in normal vaginal flora towards polymicrobial infection with anaerobes |
|
|
Amsel critieria for bacterial vaginosis |
1. A thin, white homogeneous discharge that smoothly coats the vaginal walls. |
|
|
Conditions in DDX for vulvovaginal discharge/itching |
allergic or chemical vaginitis atrophic vaginitis scabies, vaginal foreign bodies |
|
|
Pelvic inflammatory disease |
Infectious disease of female upper genital tract
Any combination of endometritis, salpingitis, peritonitis, and tubo-ovarian abscess |
|
|
Summary of STI Treatment |

|
|
|
DDX of rash on palm/sole |
P - Psoriasis A - Atopic dermatitis L - Lips/Hand/Foot/Mouth Disease (coxsackie) M - Menningococcemia G - Gonnocococcemia R - RMSF E - Erythema Multiforme A - Allergic/contact dermatitis S - Syphillis (Secondary) E - Eczema
+ Toxic shock syndrome Graft versus host disease |

