![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
35 Cards in this Set
- Front
- Back
|
Examples of liver diseases? |
1. Fulminant liver failure 2. Hepatitis - viral hepatitis 3. Liver cirrhosis 4. Non-alcoholic Fatty Liver Disease (NAFLD) |
|
|
What is fulminant liver failure? |
1. Massive necrosis of liver cells (parenchyma) - leads to severe impairment of liver function - ↓ liver size 2. Acute liver failure - in patients without obvious / previous liver diseases |
|
|
Fulminant liver failure can be caused by? |
- infections - drugs - toxins - others |
|
|
How infections can cause fulminant liver failure? |
1. Viral hepatitis (HBV, HCV, CMV) - most common cause 2. Yellow fever 3. Leptospirosis |
|
|
Which drugs can cause fulminant liver failure? |
- overdose of paracetamol (PCM) - halothane, isoniazid |
|
|
Examples of toxins that can cause fulminant liver failure? |
- Amanita phalloides - carbon tetrachloride (fridge, cleaning agent) |
|
|
Other reasons of fulminant liver failure? |
- shock - malignancy - autoimmune - Wilson's disease - Budd-Chiari syndrome - HELLP syndrome |
|
|
What is Wilson's disease? |
Rare inherited disorder of copper metabolism - causes accumulation of copper in liver, brain and other vital organs |
|
|
What is Budd-Chiari syndrome? |
Obstruction of hepatic venous outflow - FROM small hepatic veins inside liver - TO inferior vena cava & right atrium |
|
|
What is HELLP syndrome? |
HELLP: H - hemolysis EL - elevated liver enzyme LP - low platelets (may associated with pre-eclampsia) |
|
|
What can be seen in patients with fulminant liver failure? |
- jaundice - hepatic encephalopathy - fetor hepaticus - tremor, apraxia - signs of chronic liver diseases |
|
|
How fulminant liver failure can cause hepatic encephalopathy? |
Liver damage - cannot detoxify absorbed products → so, nitrogenous waste (NH3) build up in circulation With portosystemic shunt - NH3 can go to brain → NH3 crosses BBB → metabolised by astrocytes (to synthesise glutamine from glutamate) → ↑ levels of glutamine →↑ osmotic pressure in astrocytes → which become swollen |
|
|
Hepatic encephalopathy is more common in which liver disease? |
Liver cirrhosis |
|
|
What is fetor hepaticus? |
Breath of dead / hepatic foetor - a condition seen in portal HTN - portosystemic shunting allows thiols to pass directly into lungs |
|
|
Fulminant liver failure can also causes coagulopathy. How to confirm this? |
- ↑ PT - INR > 1.5 |
|
|
How to diagnose fulminant liver failure? |
1. Serology - FBC, U&E, LFT - ↑ PT / INR, glucose - level of serum paracetamol - HBV, HCV, CMV, EBV - ceruloplasmin (TRO Wilson disease) - autoAb (TRO autoimmune hepatitis) - NH3 2. Microbiology - blood / urine culture - aspiration of ascitic fluid 3. Radiology - CXR - abdominal US (with Doppler of portal & hepatic veins) |
|
|
Laboratory test for fulminant liver failure? |
1. FBC - to reveal thrombocytopenia 2. Coagulation studies - PT and / or INR 3. LFT - ↑ levels of AST / ALT / ALP 4. U&E - ↑serum bilirubin level - ↑serum ammonia level (dramatically) elevated (accuracy: arterial > venous level) - ↓ serum glucose level - ↑serum (arterial) lactate level - arterial blood gas (hypoxemia) - ↑serum creatinine level - ↓ serum free Cu & ceruloplasmin levels (with Wilson disease) - ↓ serum phosphate level 5. Acetaminophen &acetaminophen-protein adducts levels 6. Drug screening - in patients - IV drug abusers 7. Blood cultures - if suspect infection 8. Viral serology - HAV immunoglobulin M (IgM) - HBsAg, HBV anticore IgM - HCV viral load testing - HDV IgM if HBsAg is positive - in posttransplantation /immunosuppressed setting, consider studies for CMV viremia, CMV antigenemia, and HSV 9. Autoimmune markers (for autoimmune hepatitis diagnosis) - antinuclear antibody (ANA) - anti-smooth muscle antibody (ASMA) - immunoglobulin levels |
|
|
How can we manage fulminant liver failure? |
1. Supportive - NG tube (to avoid aspiration) - urinary & central venous catheter (monitor I/O) - serial blood tests (FBC, U&E, LFT, INR) - adequate nutrition 2. Treat causative agent - gastric lavage / activated charcoal (for PCM overdose) - empiric ATB (for sepsis) 3. Others - hemodialysis (for renal failure) - avoid sedatives / drugs with liver metabolism (lorazepam in seizure) |
|
|
In which conditions, fulminant liver failure can be said to be medical emergency? |
Toxicity - Amanita phalloides - acute severe viral hepatitis - heat stroke (vasoconstriction in splachnic areas) |
|
|
Early complications of fulminant liver failure? |
1. Bleeding 2. Infection 3. Ascites 4. Hypoalbuminemia - edema 5. Hypoglycemia 6. Encephalopathy 7. Brain edema |
|
|
How to treat bleeding complications in fulminant liver failure? |
- may need Vit. K, plt., FFP, blood |
|
|
How to treat infections complications in fulminant liver failure? |
- IV ceftriaxone (until get culture results) |
|
|
How to treat ascites complications in fulminant liver failure? |
- restrict fluid - use diuretics |
|
|
How to treat hypoglycemia complications in fulminant liver failure? |
- check blood glucose regularly - if < 2mmol/L - give 50mL 50% glucose |
|
|
How to treat encephalopathy complications in fulminant liver failure? |
- tilt head up - avoid sedatives - use lactulose |
|
|
How to treat hypoalbuminemia? / brain edema complications in fulminant liver failure? |
- 20% IV mannitol - ventilation |
|
|
Late complications of fulminant liver failure? |
Chronic liver failure - may need transplantation |
|
|
What is portal HTN? |
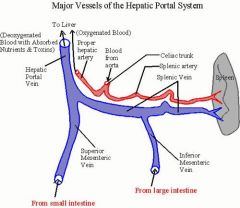
↑ pressure in portal vein (portal venous pressure > 7mmHg) |
|
|
What are normal values of pressure in veins? |
1. Portal veins 5-10mmHg 2. IVC 4-5mmHg |
|
|
Portal HTN can be caused in 3 ways (pre- / intra- / post-hepatic) - it means? |
1. Pre-hepatic - any problems that occur before reaching liver 2. Intra-hepatic - any problems of liver itself 3. Post-hepatic - any problems after passing liver |
|
|
Examples of pre-hepatic etiology in portal HTN? |
- portal vein thrombosis - congenital atresia |
|
|
Examples of intra-hepatic etiology in portal HTN? |
Liver cirrhosis |
|
|
Examples of post-hepatic etiology in portal HTN? |
- hepatic vein thrombosis - constrictive pericarditis - RHF? |
|
|
What happens in portal HTN? (pathophysiology) |
1. ↑ resistance in blood flow in portal vein 2. Blood re-route from portal veins to collateral vessels - to distal esophagus - to rectum - to stomach 3. Blood is shunt away from liver - toxic substance from intestine can be shunted directly to systemic circulation |
|
|
What can be seen in patients with portal HTN? |
1. Splenomegaly - ↑ pressure in splenic veins - thrombocytopenia - leukopenia 2. Caput medusae - collateral vessels in abdominal wall 3. Esophageal varices - risk of upper GI bleeding 4. Gastric varices 5. Rectal varices - maybe mistaken for hemorrhoids 6. Fetor hepaticus 7. Ascites - portal HTN + hypoalbuminemia - venous congestion within visceral organs 8. Hepatic encephalopathy |

