![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
64 Cards in this Set
- Front
- Back
|
Fecal-Oral Transmission Factors
What are the poor personal hygiene factors? |
children (eg, day-care centers)
institutions (eg, prisons, mental hospitals, orphanages) food handlers |
|
|
Fecal-Oral Transmission Factors
What are the issues with developing countries? |
poor sanitation
lack of indoor plumbing endemic travelers' diarrhea |
|
|
Fecal-Oral Transmission Factors
- what cause water-borne epidemics? |
water treatment failures
|
|
|
Fecal-Oral Transmission Factors
- what are the risk factors for homosexuals? |
oral-anal contact
|
|
|
Fecal-Oral Transmission Factors
- Is zoonosis an issue? |
Entamoeba = no
Cryptosporidium = yes Giardia = controversial |
|
|
Intestinal protozoa - which ones are flagellates?
|
Giardia lamblia
Dientamoeba fragilis Pentatrichomonas hominis Chilomastix mesnili Enteromonas hominis Retortamonas intestinalis |
|
|
Intestinal protozoa - which ones are amebas?
|
Entamoeba histolytica
Entamoeba dispar Entamoeba coli Entamoeba hartmanni Endolimax nana Iodamoeba bütschlii |
|
|
Intestinal protozoa - which ones are apicomplexa?
|
Cryptosporidium hominis
Cryptosporidium parvum Cyclospora cayetanensis Isospora belli |
|
|
Intestinal protozoa - which ones are the others?
|
Blastocystis hominis
Balantidium coli |
|
|
Intestinal protozoa - which stage is infective?
|
cysts - they are passed in feces and are resistant
|
|
|
What are the other lumen-dwelling protozoa?
|
Other Lumen-Dwelling Protozoa
Trichomonas vaginalis (urogenital) Trichomonas tenax (oral) Entamoeba gingivalis (oral) |
|
|
What are the life cycle characteristics of trophozoites?
|
feeding
motile replicative |
|
|
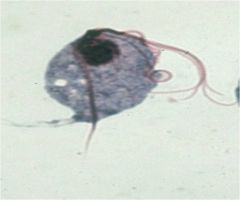
Giardia lambia, trophozoite
|

Who am I and what stage?
|
|
|
What is the most common protozoa in stools?
|
giardia lambia
most common protozoa in stools ~200 million clinical cases/yr |
|
|
How many taxonomy species of giarida are there?
|
Taxonomy
one human species, aka: G. duodenalis G. intestinalis morphologically similar forms in other mammals |
|
|
Who first observed giardia?
|
1681 van Leeuwenhoek observed
|
|
|
Who first document clinical symptoms of giardia
|
1859 Lambl documented
1920’s clinical symptoms, but controversial 1954 Rendtorff fulfilled Koch’s postulate |
|
|
What are the transmission factors of giardia?
|
Fecal-Oral Transmission Factors
- poor personal hygiene -- children (eg, day care centers) -- food handlers developing countries -- poor sanitation -- endemic -- travelers diarrhea water-borne epidemics zoonosis? -- Entamoeba =no -- Cryptosporidium =yes -- Giardia =controversial |
|
|
Is giardiasis a zoonsis?
|
Is giardiasis a zoonosis?
limited documentation transmission between humans and dogs rare (J.Parasit. 83:44, 1997) person-to-person trans-mission is most prevalent |
|
|
How many clades are human isolates found in giardiasis?
|
human isolates only found in clades A and B
Giardia relatively host specific zoonotic transmission relatively rare virulence? |
|
|
What are the in vitro culture excystation features of giardia?
|
Excystation
brief exposure to acidic pH (~2) flagellar activity within 5-10 min after return to neutral pH breakdown of cyst wall (proteases) trophozoite emerges from cyst cytokinesis within 30 min |
|
|
What are the in vitro culture encystation features of giardia?
|
growth at pH 7, no bile
exposure to pH 7.8, high bile cyst wall secretion (appearance of vesicles) loss of disk and flagella nuclear division |
|
|
microtubules
tubulin microribbons giardins lateral crest actin-myosin |
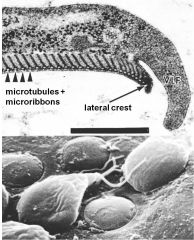
What are the adhesive disk components of giardia?
|
|
|
what are the attachement mechanisms of giardiasis?
|
- Attachment Mechanisms?
contractile force receptor mediated |
|
|
What are the range of outcomes with giardiasis?
|
asymptomatic/latent
acute short-lasting diarrhea chronic/nutritional disorders |
|
|
What are the subacute/chronic symptoms of giardiasis?
|
recurrent diarrheal episodes
cramps uncommon sulfuric belching, ano-rexia, nausea frequent can lead to weight loss and failure to thrive |
|
|
What are the acute symptoms of giardiasis?
|
Acute Symptoms
1-2 week incubation sudden explosive, watery diarrhea -- bulky, frothy, greasy, foul smelling stools -- no blood or mucus upper gastro-intestinal uneasiness, bloating, flatulence, belching, cramps, nausea, vomiting, anorexia usually clears spontaneously (undiagnosed), but can persist and become chronic |
|
|
What are the possible mechanisms of pathogenesis for giardiasis?
|
mechanical irritation
inflammation |
|
|
- epithelial damage
-- villus blunting -- crypt cell hypertrophy -- some inflammation - electrolyte transport -- malabsorption of glucose, Na+, water, etc -- hypersecretion of Cl- - enzyme deficiencies -- lactase → lactose intolerance |
What is the pathogenesis of giardiasis?
|
|
|
What is a confirmed diagnsis of giardiasis?
|
confirmed: detection of parasite in feces or duodenal aspirate or biopsy
|
|
|
What are the lab issues with giardiasis?
|
parasite easy to identify
parasite can be difficult to detect inconsistent excretion in feces patchy loci of infection |
|
|
How do you diagnose giaridasis via parasite detection?
|
Parasite Detection
Stools 3 non-consecutive days wet mounts or stained IFA, copro-antigens Aspirate or Biopsy Enterotest (or string test) |
|
|
How do you treat giardiais?
|
Drug of Choice
metronidazole (Flagyl) 750 mg/tid/5d >90% cure rate Alternatives tinidazole (single dose) paromomycin (pregnancy) quinicrine furazolidone Prognosis is good and generally with no sequelae |
|
|
How do you control giardiasis?
|
avoid fecal-oral transmission
improve personal hygiene - especially institutions treat asymptomatic carriers - eg, family members health education - hand-washing - sanitation - food handling protect water supply treat water if questionable - boiling - iodine - not chlorine |
|
|
where does giardia inhabit?
|
small intestine - duodenum
|
|
|
How many cysts do you need to get infected with giardiasis?
|
10
|
|
|
Describe basic morphology of trichomonads
|
3-5 anterior flagella
one undulating membrane axostyle hydrogensome (EM) |
|
|
cave
|
a deep, hollowed-out area under the earth's surface
|
|
|
Trichomonad
|
Who am I?
|
|
|
How is trichomonas vaginalis transmitted?
|
trophozoite stage transmitted during sexual intercourse
- non-sexual contact possible common STD - co-infection w/other STDs - more prevalent in at risk groups |
|
|
What specific tissue is trichomonas vaginalis attacted to?
|
associated with epithelium of uro-genital tract
- females: vagina - males: urethra, prostate, epididymis |
|
|
Who is more susceptible to getting trichomonas vaginallis?
|
both sexes equally susceptible
symptoms more common in females |
|
|
What is the clinical presentation of trichomonas vaginalis in females?
|
ranges from asymptomatic, to mild or moderate irritation, to extreme vaginitis
- 50-75% abnormal discharge (frothy, yellowish or greenish) - 25-50% pruritis - 50% painful coitus onset or exacerbation often associated with menstruation or pregnancy vaginal erythema, ‘strawberry cervix’ (~2%) |
|
|
What is the clinical presentation of trichomonas vaginalis in males?
|
50-90% are asymptomatic
mild dysuria or pruritus minor urethral discharge |
|
|
HIV and Trichomoniasis - How does trich affect one's immunity and how does that relate to HIV?
|
Leukocyte infiltration and lesions may increase target cells (CD4, MΦ) for HIV
- increased inflammatory response is localized in the sexual organs |
|
|
HIV and Trichomoniasis - how does it effect transmission?
|
Trichomonas infections may enhance HIV transmission by 1.5-3X
Possible increased level of HIV-infected cells in genital area during co-infection ↑ cervical shedding of HIV ↑ viral loads in semen |
|
|
Ho do you diagnose trichomoniasis?
|
demonstration of parasite
direct observation or in vitro culture - vaginal discharge - urine sediment - prostatic secretion |
|
|
How do you txt trich?
|
metronidazole (Flagyl)
- 250 mg (3/d) for 5-7 days - single 2 g dose simultaneous treatment of partner! (85-90% cure rate) |
|
|
How do you prevent trich?
|
limit # of sexual partners
condoms |
|
|
what is unique about dientamoeba fragilis' life cycle?
|
has no cyst stage, only trophozoites
|
|
|
What is morphologically unique about dientamoeba fragilis?
|
it is often binucleated
|
|
|
How is dientamoeba fragilis transmitted?
|
- it has no cyst stage, only trophozoites
- transmission via the pinworm Enterobius vermicularis? - 15-30% of infections associated with diarrhea and other GI symptoms |
|
|
how do you treat dientamoeba fragilis?
|
iodoquinol is drug of choice
|
|
|
What is unique about ciliates?
|
covered with rows of cilia
defining characteristic is nuclear dimorphism micronucleus (genetic) macronucleus (somatic) sexual reproduction involving conjugation |
|
|
How many ciliates infect humans?
|
Despite being a large and diverse group - majority free-living - only Balantidium coli infect humans
|
|
|
How do ciliates reproduce?
Describe pathways |
asexually and sexually.
Asexually - trophozoites replicate by binary fission in which both the macro- and micornucleus undergo mitosis and each of the daughter cells receives copies of both. -- DNA synthesis, mitosis, cytokinesis - Sexually - Trophozoites pair and exchange nuclei during sexual reproduction. -- macronucleus formation -> pairing and meiosis --> loss of macronuculeus and 3 micronuclei --> mitosis and nuclei exchange --> nuclear fusion and speration |
|
|
Where do you geographically see Balantidium coli?
|
world-wide distribution
- especially prevalent in tropics - rarely exceeds 1% common in pigs and monkeys - unlikely to be reservoirs |
|
|
Describe where B coli reside and basic pathology
|
usually non-pathogenic commensal in colon
can invade intestinal epithelium and cause ulceration with dysentery-like symptoms |
|
|
What are the symtpoms of balantidosis (balantidiasis or balantidial dysentery)
|
symptoms: acute diarrhea with mucus and blood, cramps
|
|
|
How do you diagnose balantidosis?
|
diagnosis: identify cyst or trophozoite in feces
|
|
|
How do you treat balantidosis?
|
tetracycline or iodoquinol
|
|
|
Balantidium coli
|
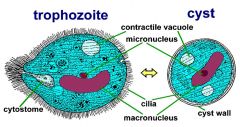
Who am I?
|
|
|
Blastocyctis hominis
- big blob - vacuole - smaller blobs ontop - nuclei |
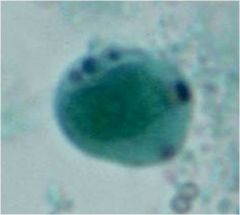
Who am I? What is the big blob in the middle and smaller blobs on top?
|
|
|
What is the presumed pathology of blastocystis hominis?
|
pathology debated
GI symptoms (diarrhea, cramping, etc) in some cases treatment alleviates symptoms - life cylce and mode of transmission unknown - presumed fecal oral |

