![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
Proinflammatory triggers stimulate T cells and Macrophages to secrete what?
(leading to inflammation) |
Cytokines (TNFa)
AA metabolites (PG, LT) Growth Factors Oxygen radicals |
|
|
UC vs. CD
Restricted to colon Continuous lesion Superficial layers Th2 cells predominate |
UC
|
|
|
UC vs. CD
Any part of GI tract Patchy lesions Superficial and deep layers Th1 cells predominate Can develop **FISTULAS** |
CD
|
|
|
Where do prostaglandins and
leukotrienes come from? |
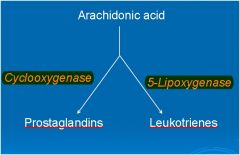
Arachidonic Acid
|
|
|
Differentiate between remission and the acute phase (active disease) of IBD
|
• Active = pain, bloating, bloody diarrhea—use Rx to induce remission
|
|
|
MOA:
Blocks BOTH cyclooxygenase and lipoxygenase = ↓PGs and ↓LTs |
5-Aminosalicytes
Note: **Inhibition of lipoxygenase has MOST beneficial treatment effect!** |
|
|
Drug Class?
Sulfasalazine Olsalazine Balsalazide Mesalamine (oral and rectal) |
5-Aminosalicytes
"-sala" |
|
|
"-sala"
|
5-Aminosalicytes
|
|
|
↓lipoxygenase = ↓ ______ ?
|
Leukotrienes
(This ↓inflammation and PMN chemotaxis) |
|
|
Which 5-ASA agent can be given as both a rectal suppository and enema?
|
Mesalamine
|
|
|
These drugs have:
- Topical effect on the GI tract - Block the production of leukotrienes |
5-ASA
|
|
|
NSAIDs have not been shown
to be beneficial in IBD. What does this imply? |
Getting rid of PGs (by blocking COX-1) does not help in IBD.
Blocking leukotrienes DOES help! |
|
|
How do you prevent
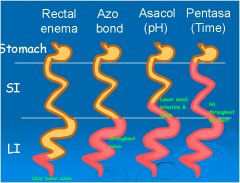
systemic absorption of 5-ASA agents? |
Give as:
-Rectal suppository -Enema -Time released capsule -Conjugated to a carrier |
|
|
Explain conjugated carriers of 5-ASA used to increase absorption in the colon
|
Sulfasalazine – carrier is sulfapyridine
Olsalazine – carrier is another molecule of 5-ASA Balsalazide – carrier is an inert molecule These form an AZO BOND (N=N) which is cleaved by BACTERIAL AZOREDUCTASE in the colon. Then, they are absorbed! |
|
|
What is the rationale for
conjugating 5-ASA with sulfapyridine? |
We don't want 5-ASA being absorbed in the small intestine. We need it to be absorbed in the lower GI/ Colon!
|
|
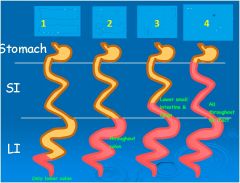
Rectal enema
Azo bond Asacol Pentasa |
|
|
|
Compare the ability of 5-ASA compounds to induce remission and maintain remission in IBD
|
Sulfasalazine/mesalamine = 1st Line/DOC** for BOTH inducing AND maintain remission in Mild-Moderate UC/CD
- Sulfasalazine has the best evidence for inducing remission with CD (vs mesalamine) |
|
|
Clincal Use:
Mild to moderately active ulcerative colitis - Induce remission - Maintenance of remission |
5-ASA
|
|
|
Compare the ability of 5-ASA compounds to treat mild to moderate IBD and severe IBD
|
They don't treat severe IBD!!!
-Give corticosteroids to induce remission -Immunosuppressants to maintain remission |
|
|
sulfasalazine vs. mesalamine
Side Effects: Male infertility |
sulfasalazine
**d/t the sulfapyridine released** (Remember, sulfasalazine is conjugated with sulfapyridine to increase colon absorption.. When the AZO BOND is cleaved, sulfasalazine blocks leukotriene formation and sulfapyridine causes SEs) |
|
|
sulfasalazine vs. mesalamine
Side Effects: o Skin rash o Hemolytic anemia o Agranulocytosis o Pulmonary complications o Hepatitis o Pancreatitis* |
sulfasalazine
**Hypersensitivity reaction from the sulfapyridine released** |
|
|
sulfasalazine vs. mesalamine
Side Effects: -Folic Acid Deficiency |
sulfasalazine
|
|
|
sulfasalazine vs. mesalamine
–Adverse Effects o Headache o Dyspepsia o Skin rash o Diarrhea |
mesalamine
|
|
|
Clinical Use:
o Clinical Use - Moderate to severely active ulcerative colitis or Crohn’s disease ***Induce remission*** o Mild to moderate UC or CD: 2nd line choice** - Severe and/or steroid resistant or dependent UC or CD: 1st line choice** **Not effective for maintaining remission** |
Corticosteroids
|
|
|
A patient with a history of Crohn's Disease is not currently on any medications and is believed to have a fistula. How can you treat?
|
Add Metronidazole (ABX)
|
|
|
A 35-year-old female is diagnosed
with ulcerative colitis. A trial of sulfasalazine is ineffective. She continues to have 3-5 bloody stools per day. What can you do for her? |
Steroids to reduce inflammation
|
|
|
Drug Class?
Prednisone Methyprednisolone Hydrocortisone Budesonide |
Corticosteroids
|
|
|
What is the main problem with
the use of corticosteroids (especially long term)? |
SIDE EFFECTS!
|
|
|
What is the potential
advantage of budesonide vs. prednisone? |
Less Side Effects!!
|
|
|
Name the Corticosteroid:
- Controlled ileal release formula -High affinity for the glucocorticoid receptor -80-90% is eliminated by first pass metabolism in the liver ***Works topically*** **NO SYSTEMIC CONCENTRATION** **LESS SIDE EFFECTS** |
Budesonide
|
|
|
Clincal Use:
- Moderate to severely active ulcerative colitis or Crohn’s disease - Oral, rectal, or parenteral - Induce remission **Not effective at maintaining remission** |
Corticosteroids
|
|
|
This corticosteroid NOT used systemically—d/t HIGH affinity for MC receptors—do NOT want activation here, as it may alter electrolytes
|
Hydrocortisone enema
|
|
|
What corticosteroid has been shown to prolong time to relapse in pts with CD in medically induced remission
|
Budesonide
|
|
|
Describe Steroid Responsive Patients with IBD
|
- Clinical improvement 1-2 weeks
-Remain in remission when drug tapered slowly over weeks or months |
|
|
Describe Steroid Dependent Patients with IBD
|
- Clinical improvement 1-2 weeks
- Relapse when steroid dose is tapered |
|
|
General Class of drugs?
**Thiopurine analogs** - Azathioprine - 6-Mercaptopurine **Methotrexate** **Cyclosporine** |
Immunosuppressive Agents
|
|
|
If a person is unresponsive to steroids,
or is steroid dependent, or has severe disease and goes into remission with steroids, what else can you do? |
Try Immunosuppressive Agents
|
|
|
Why are Azathioprine and 6-mercaptopurine good for maintaining remission?
|
take SIGNIFICANTLY longer for onset of action in inducing remission
~3-6 months MTX and Cyclosporine can take a few weeks and aren't as good for maintenance ---> better for INDUCING REMISSION |
|
|
What are the TNF-a inhibitors for IBD?
|
Infliximab**
Adalimumab Certolizumab Pegol (Monoclonal antibodies to TNF-a) |
|
|
MOA:
- Binds to membrane bound TNF-α on MΦ or activated T cells and induces cell death - Binds to soluble TNF-α and prevents it from binding to the TNF receptor on target cells - This prevents the inflammatory effects of TNF-α in IBD |
Infliximab**
|
|
|
What is entanercept? Is it useful in IBD?
|
Etanercept= the RA Rx
It is a Recombinant TNF-α receptor– not effective for treating IBD |
|
|
Clinical Use:
- For inducing remission in patients UNRESPONSIVE to steroids - For reducing steroid use in pts that are steroid dependent - For MAINTENANCE therapy in severe IBD after inducing remission with steroids - Fistulizing Crohn’s disease |
Immunosuppressant Agents
|
|
|
Clinical Use:
**Moderate to severe Crohn’s disease** • Induce remission • Maintain remission **Fistulizing Crohn’s disease** **Moderate to severe ulcerative colitis** • Induce remission • Maintain remissio |
Biological Response Modifiers- TNF-α inhibitors
(Infliximab is especially helpful in UC!!) |
|
|
Many patients with CD need dosage
adjustments or lose their response to infliximab. Why might that be? |
Development of antibodies to infliximab (remember, it's 25% mouse) as the drug gets into the serum
**Adalimumab** can be used in patients who have lost response to, or are intolerant to infliximab |
|
|
You have induced remission with steroids in a patient that had been diagnosed with Severe UC. What drug can you give next to maintain remission?
|
infliximab !!
Great for inducing and maintaining remission in severe/moderate UC |
|
|
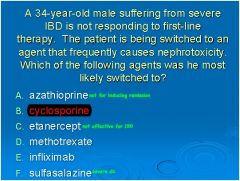
A 34-year-old male suffering from severe IBD is not responding to first-line therapy. The patient is being switched to an agent that frequently causes nephrotoxicity. Which of the following agents was he most likely switched to?
A. azathioprine B. cyclosporine C. etanercept D. methotrexate E. infliximab F. sulfasalazine |
|

