![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
85 Cards in this Set
- Front
- Back
|
Based on the mucsularis propria composition, identidy the section of the esophagus:
- skeletal muscle only |
upper 1/3
|
|
|
Based on the mucsularis propria composition, identidy the section of the esophagus:
- smooth muscle only |
middle 1/3
|
|
|
Based on the mucsularis propria composition, identidy the section of the esophagus:
- mixture of skeletal and smooth muscle |
lower 1/3
|
|
|
Meissener's plexus exist in ___ layer where as Aeurbach (myenteric) plexus exist in ____ layer.
|
- Meissener's: submucosa
- Auerbach: between inner circular and outer longitudinal layers of muscularis propria |
|

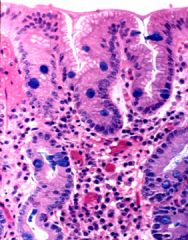
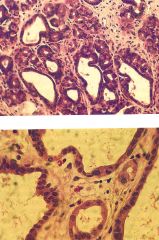
What is this lesion? What is the most common histologic feature of this lesion?
|
ectopia
- gastric type mucosa most common |
|
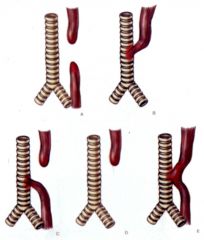
Which is the most common type of esophageal atresia?
|
C
- regurgitation - paroxysmal choking - aspiration of liquid into lungs |
|
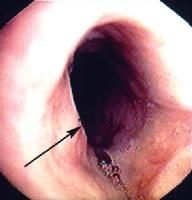
What is this lesion?
- 40 y/o women with glottitis - fe deficiency |
Plummer-Vinson syndrome
- risk of developing squamous carcinoma in oral cavity, hypopharynx, and esophagus |
|

What is this lesion?
|

Schatzi's ring
- circumferential ring in esophagus |
|

What is this lesion? Pathogenesis?
- location: hypopharynx - older person - regurgitation - mass effect in the neck |
This is Zenker's diverticula
- pulsion: weak area at junction of pharyngeal constrictors (Killian's triangle). Increased luminal pressure would then cause diverticulum. |
|
|
What is this lesion?
- nocturnal regurgitation of large volumes of fluid - mass just above LES - motility problem |
epiphrenic diverticula
|
|
|
Pathogenesis of traction diverticula.
|
inflammation -> fibrous scarring of soft tissue adherent to serosa -> pull wall of esophagus outward
|
|
|
Name the three pathogenic mechanism of esophageal diverticula.
|
- congenital
- traction: small, mid esophagus - pulsion |
|

What is this lesion?
- progressive dysphagia - nocturnal regurgitation of food |
achalasia
- degeneration of innervation: primary or secondary to malignancy, amyloidosis, sarcoidosis, other chronic disease. - aperistalsis, incomplete relaxation of LES, increased resting LES tone |
|
|
Which type of hiatal hernia is more common, sliding or rolling (paraesophageal)
|
- sliding (95%): stomach and esophagus bulge through hiatus together
- rolling(5%): stomach herniates alongside esophagus |
|
|
Management for hiatal hernia.
|
- sliding type: medical or surgery (depending on severity of morbidity)
- rolling type: surgery |
|

What is this lesion? Risk factors?
- linear lacerations in esophagus near EG junction |

Mallory-Weiss laceration
- risk factors: alcohol binge drinking, prolonged vomiting |
|
|
What are some complications of Mallory-Weiss laceration?
|
- hemorrhage
- ulceration/perforation - mediastinitis - rupture of esophagus (Boerhaave syndrome) |
|
|
Management for Mallory-Weiss laceration.
|
- supportive: bleeding stops spontaneousely
- may need endoscopic coagulation, balloon temponade or surgery |
|
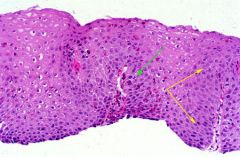
What is this lesion?
- heartburn, chest pain - regurgitation, dysphagia |
mild reflux esophagitis
- reactive squamous hyperplasia - elongated papilla in lamina propria - eosinophils in mucosa |
|
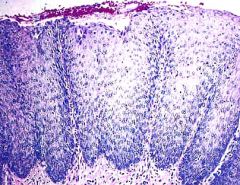
What is this esophageal lesion?
- heart burn, chest pain - dysphagia, regurgitation |
chronic reflux esophagitis
- basal zone hyperplasia - glandular metaplasia (late) |
|
|
Pathogenesis of reflux esophagitis.
|
- decreased LES tone
- sliding hiatal hernia - delayed gastric emptying - reduced capacity fro mucosal repair - slow clearance of refluxed material out of esophagus |
|
|
What are some complications of reflux esophagitis?
|
- ulceration
- stricture - Barret's metaplasia |
|

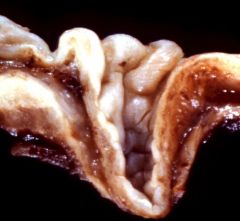
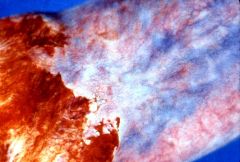
What is this esophageal lesion?
|
infectious esophagitis (candida)
- seen in immunocompromised |
|

What is this esophageal lesion?
|
infectious esophagitis (HSV)
- grondglass nuclei (cowdry bodies) - multinucleated cells - seen in immunocompromised |
|
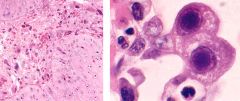
What is this esophageal lesion?
|
infectious esophagitis (CMV)
- owls eye intranuclear inclusions - seen in immunocompromised |
|

What is this esophageal lesion?
|
chemical esophagitis (arsenic)
|
|
|
Pathogenesis of Barrett's esophagus.
|
acid reflux -> inflammation -> chronic mucosal injury -> columnar metaplasia (more acid resistant)
|
|
|
What is the major concern of Barrett's esophagus?
|
40x risk for adenocarcinoma
|
|
|
What are the 2 criteria needed to make the diagnosis of Barrett's esophagus?
|
- endoscopic evidence of glandular mucosa above EG
- biopsy prove of metaplasia from squamous to columnar epithelium |
|
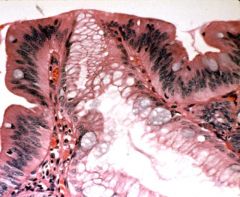
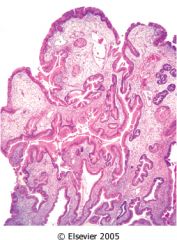
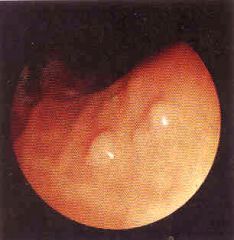
What is this esophageal lesion? management?
- gross: gray hatched areas - symptoms: chronic heartburn |
Barrett's esophagus
- low grade dysplasia (crowded nuclei) - confirm by 2nd pathologist, then endoscopy every year |
|
What is this esophageal lesion? management?
- gross: gray hatched areas - symptoms: chronic heartburn |
Barrett's esophagus
- metaplasia only - endoscopy every 3-5 yrs |
|
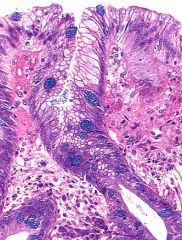
What is this lesion? management?
- chronic heartburn - gross: gray hatched areas |
Barrett's esophagus
- high grade dysplasia (cells trying to form glands) - confirm by 2nd pathologist, then esophagestomy or endoscopic ablative therapy |
|
What is this esophageal lesion? pathpgenesis? management?
- no symptoms |
esophageal varices
- cirrhosis -> portal HTN -> development of collateral bypass channels - replace intravascular volume, give blood, stop bleeding |
|
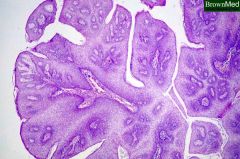
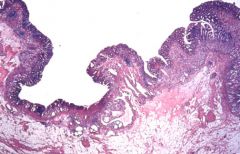
What is this esophageal lesion?
- fronds of thickened squamous epithelium supported by connective tissue cores |
squamous papilloma
- respiratory tract should also be examined for HPV related papilloma |
|
|
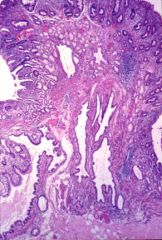
What is this esophageal lesion?
- epithelial hyperplasia - abundant vascularized connective tissue surfaced by squamous epithelium |
fibrovascular polyp
|
|
|
Which is more common in the U.S, squamous or adenocarcinoma of the esophagus? what about the world?
|
US: 50% each
World: 90% squamous, 10% adenocarcinoma |
|
|
What are some promotors of squamous carcinoma of the esophagus?
|
- vitamin A, B1, B2, B6
|
|
|
What are some risk factors for squamous carcinoma of the esophagus?
|
- alcohol
- tobacco - achalsia - chronic esophgitis - Plummer-Vinson syndrome |
|
|
Pathogenesis/carcinogenesis of squamous carcinoma of the esophagus.
|
TP53 -> LOH (low grade intraepithelial neoplasia) -> overexpression of cyclin D1 -> multiple LOH
|
|
|
Pathogenesis/carcinogenesis of adenocarcinoma of the esophagus.
|
- Barrett's esophagus
- overexpression of p53 and point ,mutations in p53 |
|
|
Risk factors for adencarcinoma of the esophagus.
|
- chronic reflux esophagitis
- tobacco - obesity |
|
|
Which has better 5 yr survival, squamous or adenocarcinoma of the esophagus?
|
squamous carcinoma
|
|
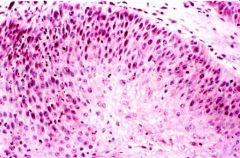
What is this esophageal lesion?
|
squamous carcinoma in situ
|
|
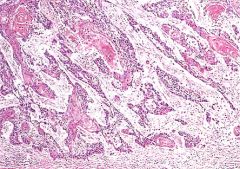
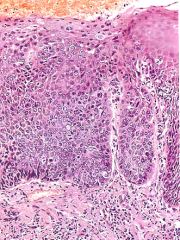
What is this esophageal lesion?
|
invasive squamous carcinoma
|
|

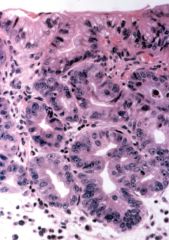
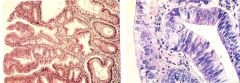
What is this esophageal lesion?
|
adenocarcinoma (right side)
metaplasia (left side) |
|
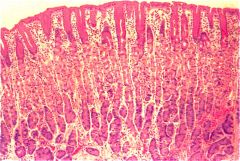
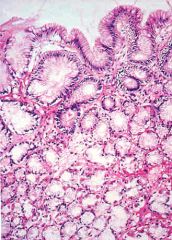
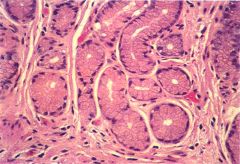
Which part of stomach is this?
|
body
- glands with parietal and chief cells |
|
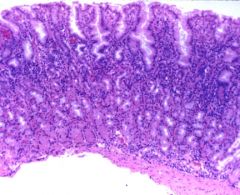
Which part of stomach is this?
|
antrum
- glands with mucinous cells |
|

What are some acquired causes of this stomach condition?
|
pyloric stenosis
- chronic gastritis - PUD - chronic inflammation |
|
|
What does this infant have?
- vomiting in the 3rd week - hypertrophy of muscularis mucosa of the stomach |

congenital pyloric stenosis
|
|

What is this stomach lesion?
|

acute gastritis
- eroded epithelium due to infiltrating and damaging epithelial cells - gross: punctate areas of mucosal hemorrhage |
|
|
Name some causes of acute gastritis.
|
- ischemic gastritis: shock
- corrosive gastritis: toxin (acid, alkali) - drug induced: NSAIDs, alcohol - smoking - chemo - uremia - bacterial or viral infection - severe stress |
|
|
What the most common site for PUD?
|
duodenum
|
|
|
How to differentiate begin and malignant PUD?
|
biopsy is the only way
|
|
|
Pathogenensis of PUD.
|
- imbalance of mucosal defense vs. damage agents
- H. pylori (GNR, flagella): urease, protease, phospholipase, PAF - attract neutrophils that release MPO |
|
|
How does chronic NSAIDS use contribute to PUD?
|
supress PGE that supress stomach acid secretion.
|
|
|
How does cigarette smoking contribute to PUD?
|
ischemia -> impair blood flow and healing of erosions
|
|
|
How does steroids contribute to PUD?
|
impair mucosal defense
|
|

What is this stomach lesion?
|

gastric ulcer
|
|

What is this stomach lesion? pathogenesis?
|
stress ulcer (small <1cm red-brown shallow ulcers)
- impaired oxygenation of mucosa -> ischemia - central stimulation of vagal nuclei -> acid hypersecretion |
|
|
In what population would you more likely to see stress ulcer?
|
- people with illness requiring intensive care
- need to prophylax these patients for stress ulcer |
|
|
What are some causes of chronic gastritis?
|
- H. pylori
- antoimmune - toxins: alcohol, cigarette abuse - bile reflux - motor/mechanical: atony, obstruction, bezoar |
|
|
How does chronic gastritis lead to adenocarcinoma of the stomach?
|
chronic inflammation -> epithelial atrophy -> chronic epithelial regeneration -> intestinal type metaplasia -> epithelial dysplasia -> adenocarcinoma
|
|
|
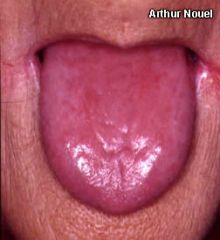
Pathogenesis of this condition:
- chronic gastitis - pernicious anemia |
autoimmune cause of chronic gastritis
- anti-parietal cell and anti-IF -> destruction of parietal cells -> glandular atrophy, decreased HCl and IF -> pernicious anemia |
|
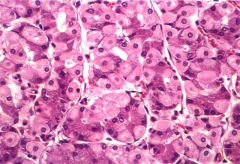
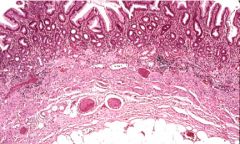
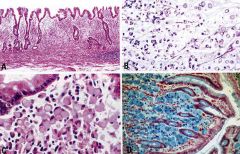
Describe this biopsy of the stomach.
|
chronic superficial gastritis
|
|
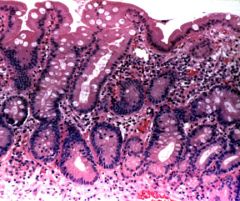
Describe this biopsy of the stomach.
|
chronic atrophic gastritis
- thin mucosa - whole mucosa infiltrated with neutrophils |
|
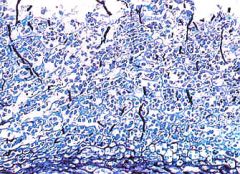
Describe this biopsy of the stomach.
|
chronic gastritis with intestinal metaplasia
- acidic mucin stain |
|
What is this stomach lesion?
- enlarged rugae - diarrhea, protein loosing, wt loss, epigastric pain |
Menetrier disease
- hyperplasia of foveola mucus secreting cells with atrophy of deeper glands -> excessive mucus secretion |
|
|
What is this stomach lesion?
- enlarged rugae - hyperplasia of parietal and chief cells in glands of the body - increased HCl secretion and PUD |
hyperplasia-hypersecretory gastropathy
|
|
|
What is this stomach lesion?
- enlarged rugae - diffuse hyperplasia of gastric glands in the body - intractable, chronic recurrent PUD - mass in duodenum |
Zollinger-Ellison syndrome
- gastrin-producing tumor in duodenum -> diffuse hyperplasia of gastric glands in the body -> excessive HCl -> PUD |
|
What is this stomach lesion?
- polyp in the stomach |

hyperplastic polyp
- hyperplasia of gastric epithelium - no dysplasia - no risk for cancer |
|
What is this stomach lesion?
- multiple smooth bumps in mucosa - hyperplasia and cystic dilation of body type glands lined by parietal and chief cells |
Fundic gland polyp
- no risk for cancer |
|
What is this stomach lesion?
- tubular branching glands with intact basement membrane - lined by dysplastic cells |

gastric adenoma
|
|

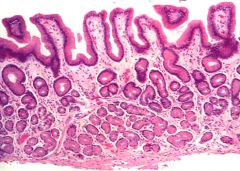
What is this stomach lesion?
|
early gastric adenocarcinoma (intramucosal)
|
|

What is this stomach lesion?
|
early adenocarcinoma (submucosal)
- invading submucosa |
|

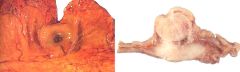
What is this stomach lesion?
- wt loss, anemia, pain, bleeding - intestinal type epithelium |

late adenocarcinoma (ulcerated)
|
|

What is this stomach lesion?
- wt loss, anemia, pain, bleeding - intestinal type epithelium |
late adenocarcinoma (fungating)
|
|
What is this stomach lesion?
- often associated with linitis plastica (diffuse infiltrative adenocarcinoma) |
late adenocarcinoma (single ring cell type)
- mucinous |
|
|
Name some risk factors for gastric adenocarcinma in the following categories:
- environmental - host - genetic |
- environmental: H. pylori, nitrates in water and preserved foods, lack of fruits and vegetables, smoking
- host: chronic gastritis, partial gastrectomy (reflux of alkaline fluids), gastric dysplasia - genetic: type A blood, famili history, HNPCC |
|
|
Prognosis of gastric carcinoma based on stage:
T1 |
95% 5 yr survival
|
|
|
Prognosis of gastric carcinoma based on stage:
T2 |
70% 5 yr survival
|
|
|
Prognosis of gastric carcinoma based on stage:
T3 |
50% 5 yr survival
|
|
|
T/F: Most patients with gastric carcinoma beyond stage T1 are rarely cured.
|
T.
most have lymph node metastases at the time of diagnose. |
|

What is this stomach lesion?
- H pylori postive - trisomy 3, or t(11,18) |
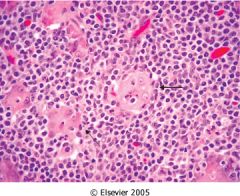
MALT - resistant to antibiotics
- mucosa infiltrated by lymphocytes |
|

What is this stomach lesion?
|
GIST (gatrointestinal stromal tumors)
- submucosal tumor which elevates and ulcerates mucosa - spindle cell mesenchymal neoplasms - treat with STI571 (tyrosine kinase inhibitor) - use CD117 (c-KIT tyrosine kinase receptor) to guide treatment |
|
|
How to manage GIST patients?
|
- c-KIT tyrosine kinase receptor gene -> CD117 to guide treatment choice
- treat with STI571 (tyrosine kinase inhibitor) |

