![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
84 Cards in this Set
- Front
- Back
|
Basic layers of the gut wall (5) starting from the lumen |
1. Mucosa (includes epithelium and lamina propria) 2. Muscularis Mucosa 3. Submucosa 4. Muscularis Externa (two or three layers of smooth muscle) 5. Serosa |
|
|
Characteristics specific to the layers of the esophagus |
Nonkeratinized, stratified squamous without secretory or absorptive cells (LP undistinguished) Prominent muscularis mucosa Submucosa contains mucous glands, lymphoid cells, blood vessels and is rich is elastic fibers; upper and lower parts will have cardiac glands Proximal 1/3 of the two-layered muscularis externa is striated muscle Adventitia is connective tissue w/blood vessels and nerves that attaches the esophagus to the diaphragm |
|
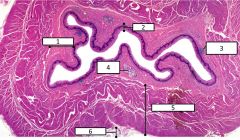
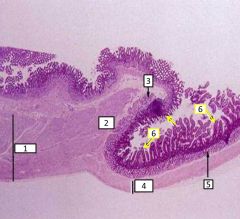
Esophageal features |
1 - submucosal layer 2 - mucosal layer 3 - lymphatic nodule 4 - mucous gland (in the submucosa) 5 - muscularis externa (striated = proximal 1/3) 6 - adventitia |
|
|
Muscularis externa is innervated by... |
vagus (X) nerve |
|
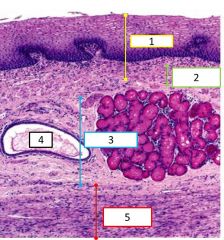
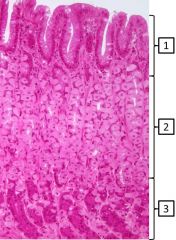
Histological features of the esophagus |
1 - mucosa 2 - muscularis mucosa 3 - submucosa 4 - duct (next to cardiac glands) 5 - muscularis externa |
|
|
What are the two esophageal sphincters and their actions? |
Upper (UES) is associated with the larynx and relaxes during swallowing Lower (LES) is where the stomach meets the esophagus Both are tonically contracted except during swallowing |
|
|
Characteristics specific to the stomach |
Simple columnar epithelium covers the luminal surface and invaginates into the lamina propria to form gastric glands; it contains many types of secretory cells Distinct muscularis mucosa No glands in the submucosa (connective tissue, blood vessels, lymphoid cells) Muscularis externa has 3 layers (inner oblique, middle circular, outer longitudinal)
|
|

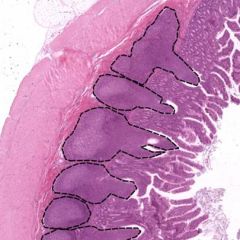
Histology of the stomach - gastric pit is outlined in yellow |
1 - submucosa 2 - fundus 3 - neck 4 - isthmus |
|
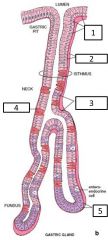
Gastric pit - what are the major cell types or indicated structures at each area? |
1 - surface mucous cells 2 - basal lamina 3 - mucous neck cells 4 - parietal cell (in the neck) 5 - chief cells (in the fundus) |
|
|
What are the four major secretory products from the gastric epithelium? |
Mucous, acid (HCl by parietal cells), proteases (pepsinogen by chief cells), hormones (gastrin by enteroendocrine cells) |
|
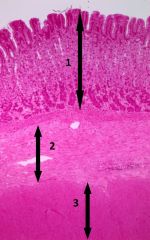
What are the indicated layers of the stomach? |
1 - mucosa 2 - submucosa 3 - muscularis externa |
|
What is/are the predominant cell type(s) in the indicated areas of gastric mucosa? |
1 -surface mucous cells 2 - mucous neck cells, parietal cells 3 - chief cells |
|
|
Where are the stem cells located and what is their turnover rate? |
Most stem cells are located in the isthmus and can replace every cell type in the epithelium Surface cells turnover every 2-3 days but other cell types are longer (months) |
|

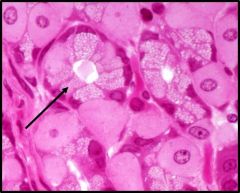
What is this cell and its function? |
Surface mucous cells create mucinogen granules -> granules form a "cap" on surface -> cap combines with water = mucin -> mucous Mucous provides mechanical protection and a bicarbonate barrier to protect the epithelial cells from gastric juices |
|
What is this cell and its function? |
Mucous neck cells have less mucinogen, smaller granules, and no cap. They form a more soluble mucous and are under vagal control |
|

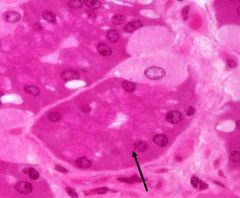
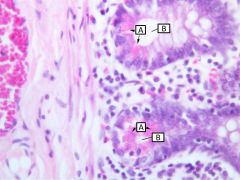
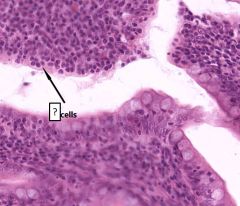
What are these cell types and the function of A? |
A - parietal cell (fried egg appearance with prominent nucleus and eosinophilic cytoplasm) produces HCl B - mucous neck cell |
|
|
How does a parietal cell produce acid without damaging itself? |
The H+ and Cl- are delivered to the lumen by secretory vesicles where they then combine for HCl |
|
|
How does the function of the parietal cell determine its appearance? |
The cytoplasm is eosinophilic because the vesicle transport process is mediated by an ATP-dependent H+/K+ proton pump in the canalicular membrane requiring mitochondria = eosinophilia |
|

Cell type and its characteristics |
Enteroendocrine cells are present throughout the gland but most prominent in the base. They contain small, poorly preserved, light colored granules. Each cell is specialized to one type of hormonal secretion |
|
|
Enteroendocrine cell secretions by GI segment |
Stomach = histamine, gastrin, VIP, somatostatin Duodenum/jejunum = gastrin (mostly duodenum), CCK, secretin, VIP, GIP, motilin, somatostatin Ileum = minorly CCK and secretin, VIP, somatostatin Colon = VIP, somatostatin |
|
Cell type and its function |
Chief cells are protein secreting so they have abundant rough ER basally (basophilic appearance). The apical surfaces are more eosinophilic because of the secretory (zymogen) granules with enzyme precursors. Secretions are pepsinogen (converted to pepsin on contact w/gastric juices) and a weak lipase. |
|
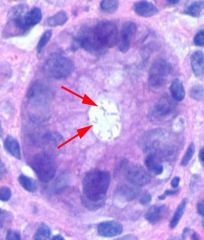
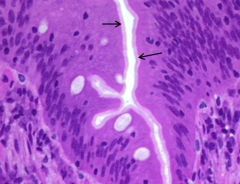
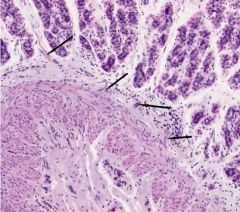
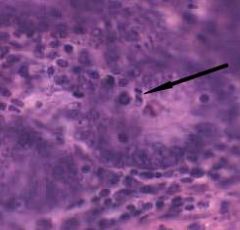
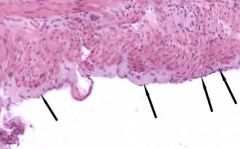
What is this pathology and what is indicated by the arrows? |
H pylori invasion of the mucosa - arrows point to the organism |
|
Gastroduodenal junction |
1 - Muscularis externa is thick in the pyloric stomach 2 - Pyloric sphincter formed by ME 3 - Brunner's glands in the submucosa 4 - ME is thinner in the duodenum 5 - Brunner's glands in the submucosa 6 - Mucosa has become villi in the duodenum |
|
|
What are the identifying characteristics of the small intestine? |
mucosa evaginates as villi simple columnar epithelium invaginates into lamina propria to form glands (crypts of lieberkuhn) muscularis mucosa is distinct only the duodenum has submucosal glands ME is 2 layers (inner circular and outer longitudinal) |
|
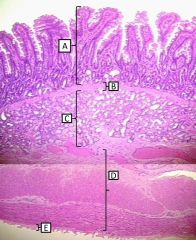
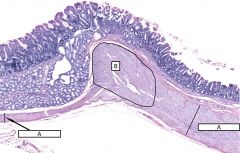
Histological layers of the duodenum |
A - mucosa B - muscularis mucosa C - submucosa (with brunner's glands) D - muscularis externa E - serosa |
|
|
What four specializations does the small intestine have to increase surface area for absorption? |
Plicae circularis (submucosa and mucosa), villi/crypts (in/e-vaginations of the mucosa), microvilli of absorptive cells on apical surface of the villi, Glycocalyx are projections of glycoproteins from the apical plasma membrane |
|
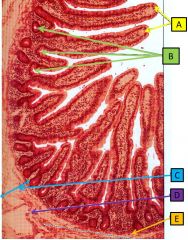
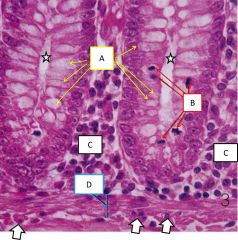
Jejunum |
A - villi B - glands C - submucosa D - vein E - muscularis mucosa |
|
|
Non-secretory cell types in intestinal epithelium |
stem cells, intermediate cells, enterocytes (absorptive cells) |
|
|
Secretory cell types in intestinal epithelium |
Enterocytes (produce digestive enzymes), goblet cells (mucus), paneth cells (lysozyme), enteroendocrine cells (secretions vary by location) |
|
|
What cell is responsible for absorption in the small intestine and how is it accomplished? |
The enterocytes in the intestinal epithelium absorb water para and trans-cellularly. Organic molecules are taken up by active transporters (transcellularly). |
|
|
What is the function of smooth ER in the absorptive enterocyte? |
It packages nutrients to be transported through the cytoplasm - when the enterocyte is more active it will have more sER |
|
|
Functional significance of Brunner's glands in the duodenum |
They secrete bicarbonate to protect mucosa and neutralize secretions from the stomach |
|
|
How do goblet cells contribute to the barrier function of the GI tract? |
Carbohydrates on mucin bind bacteria to prevent colonization and improve clearance The reduced diffusion of hydrophobic molecules across mucus slows exposure of damaging chemicals/toxins to the epithelium |
|
What are the characteristics and functions of these cells (Paneth cells)? |
Paneth cells are found in intestinal crypts; have basophilic basal cytoplasm and intensely acidophilic apical secretory granules to secrete lysozyme and phospholipase A2 that have antimicrobial activity. They defend against microbes by secreting defensins when exposed to bacteria or their products. |
|
Identify |
A - Paneth cells B - intestinal gland |
|
What is the identified structure and what is it formed from? |
Brush border - formed by microvilli of absorptive cells |
|
Cell type? |
Enteroendocrine cells |
|
|
Regional histological characteristics of the three areas of small intestine |
Duodenum has Brunner's glands Jejunum is the main absorptive site so it has the most extensive plicae and complex villi Ileum has the greatest amount of lymphoid tissue (Peyer's patches) |
|
What part of small intestine and how did you know? |
Ileum because of the amount of lymphoid tissue and more goblet cells than jejunum |
|
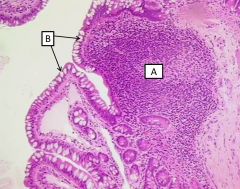
Identify cell/structure |
A - Peyer's patch extending through the muscularis mucosa B - Goblet cells |
|
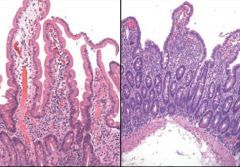
Which is normal duodenal mucosa and what is the pictured pathology? |
Left is normal - right is celiac's disease (villous atrophy, crypt hyperplasia, intraepithelial lymphocytosis) |
|
|
What are the identifying characteristics of the large intestine? |
Absence of plicae or mucosal villi Simple columnar epithelium with goblet and absorptive cells Intestinal crypts are deeper (go to MM) than in small intestine and are spaced evenly Presence of scattered lymphoid nodules in the lamina propria Outer longitudinal layer of muscularis externa forms tenia coli |
|

|
Tenia coli formed by longitudinal smooth muscle |
|
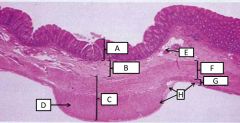
Histological features of the colon |
A - mucosa B - submucosa C - muscularis externa D - tenia coli (thick longitudinal ME) E - blood vessel F - circular ME G - longitudinal ME H - serosa |
|
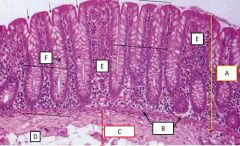
Mucosa of the large intestine |
A - mucosa B - muscularis mucosa C - submucosa D - adipose cells E - lamina propria F - goblet cell (in crypt) |
|
|
What are the key cell types in the epithelium of the large intestine? |
absorptive enterocytes, goblet cells, stem cells (deep in crypt), enteroendocrine cells |
|
|
What are the key cell types in the lamina propria of the large intestine? |
Fibroblasts, scattered lymphocytes (mostly T cells), small lymphoid nodules containing B cells, eosinophils, muciphages |
|

|
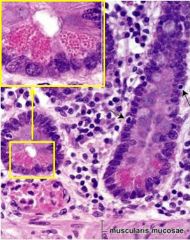
A - plasma cell B - enteroendocrine cell C - gland/crypt |
|

|
A - absorptive cells (predominate apically) B - goblet cells (predominate deeper) C - lamina propria |
|
Base of mucosal gland in large intestine |
A - goblet cells B - mitotic figures C - lamina propria D - muscularis mucosa arrows point to smooth muscle nuclei in the MM stars indicate the gland |
|
|
What are absorbed and secreted in the large intestine? |
Absorbed: water, sodium ions, chloride ions Secreted: bicarbonate ions, mucous |
|
|
How is chloride absorbed? How is this good for pH? |
chloride is exchanged for bicarb at the apical surface; the secreted bicarb will neutralize acids generated by microbial fermentation |
|
|
What controls secretion from goblet cells? |
Both tactile stimuli from the lumenal contents and parasympathetic innervation |
|
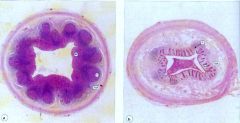
Which appendix cross section is from a child? |
The one on the left is from a child - on the right the lymphoid tissue has been replaced by fibrotic connective tissue |
|

Rectoanal junction |
A - colorectal zone (simple columnar epithelium) B - anal transitional zone (end of the MM) C - squamous zone (stratified squamous epithelium) The internal sphincter is smooth muscle (termination of muscularis externa) and the external is striated skeletal |
|
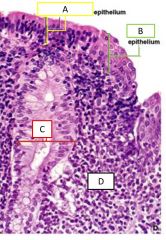
Close up of the anal transitional zone |
A - simple columnar epithelium B - stratified squamous epithelium C - anal gland (secretes mucus) D - lamina propria |
|
Lymphoid follicle - general structure |
B and T cells are in discrete zones which only have efferent lymphatics. The epithelium overlying peyer's patches contains cuboidal cells and intraepithelial lymphocytes (A). Some epithelial cells are microid cells aka M cells (B) which can transfer antigens between the patch and the lumen. |
|
|
How do M cells function immulogically? |
They have MHC2 molecules that present antigens to T cells |
|
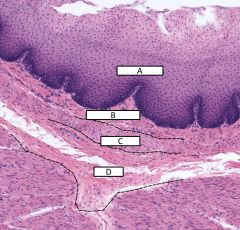
Layers of the esophagus |
A - epithelium of mucosa B - lamina propria of mucosa C - muscularis mucosa D - submucosa |
|
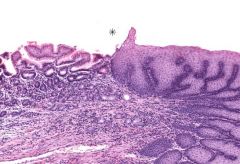
identify this transition |
transition from esophagus (on right) to stomach (on left) |
|
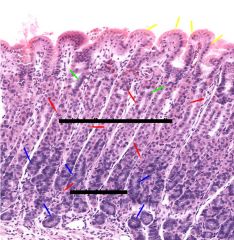
what specific region of the stomach is this? cell types? |
fudic/corpus region yellow = surface mucus cells green = mucus neck cells red = parietal cells blue = chief cells |
|
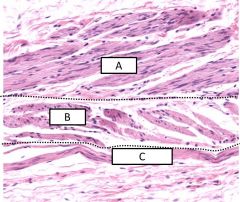
3 layers of muscle in the stomach - lumen is up |
A - inner oblique B - middle circular C - outer longitudinal |
|
fundus of the stomach |
strands of smooth muscle extend from the muscularis mucosa into the lamina propria - contraction helps propel secretions from the glands into the lumen of the stomach |
|

|
Structure 1 = duodenum Structure 2 = stomach A = Brunner's glands B = villi |
|
What is this structure? Characterize. |
The pyloric sphincter (B) is produced by a thickening of the circular layer of the muscularis externa (A) |
|
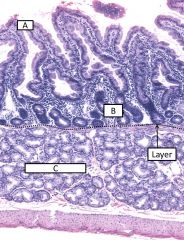
Also, what part of the small bowel is this and how do you know? |
A - villi B - crypts (glands) Layer - muscularis mucosa C - brunners glands
The duodenum is the only part of the small bowel with glands on either side of the MM |
|
|
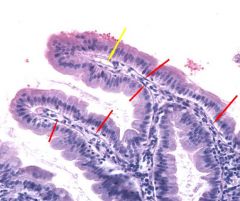
red - intestinal epithelium below the villi yellow - lacteal (lymphatic capillary) within the villus |
|
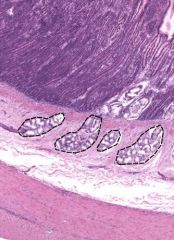
outline structure? where is this? |
Brunner's glands in the submucosa of the duodenum - can tell that you are further from the pyloric sphincter because the glands are less extensive |
|
Arrows point to one cell type - what are the other two cell types expected in this area? |
Lamina propria of the duodenal villus contains smooth muscle cells (arrows) indicating that the villus is mobile - should also contain fibroblasts and lymphocytes |
|
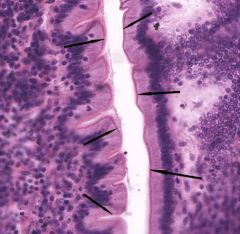
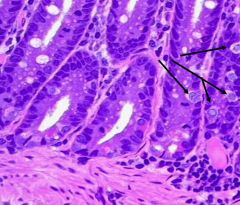
What is the indicated structure and what forms it? |
Apical surface of the intestinal epithelium in the jejunum (and duodenum) has a brightly stained eosinophilic brush border (arrows) representing microvilli extensions of absorptive cells |
|
Intestine - where specifically would this indicated figure be located? |
Arrow indicates a mitotic figure; dividing stem cells in the intestine are located on the epithelium in the deepest portion of the crypts |
|

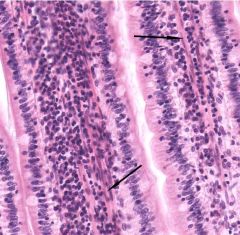
Jejunum - what cells are represented by the indicated nuclei? |
nuclei in the apical portion of the epithelium represent intraepithelial lymphocytes that have migrated up from the lamina propria into the epithelium to monitor for invading pathogens |
|

Ileum - how do you know that it is this portion of the small bowel? identify arrows |
Epithelium exhibits fewer microfolds and contains many more goblet cells (yellow) than the jejunum The absorptive cells still maintain some brush border (pink) and smooth muscle is still apparent in the core of the villus (red) |
|
Identify - location - characterize |
Peyer's patches in the ileum are lymphoid nodules with lightly stained germinal centers; some extend past the muscularis mucosa into the lamina propria Lymphoid tissue patches are throughout the GI tract but in the ileum they are large enough to be seen grossly |
|
Ileum identify cell - location - characterize |
Epithelium overlying the lymphoid nodules (which has a different pattern than epithelium in the rest of the ileum) contains M cells that transport antigens and Igs across the epithelial barrier |
|

Layers of the large bowl |
A - mucosa B - muscularis mucosa C - submucosa D1 - muscularis externa - inner circular layer D2 - muscularis externa - outer longitudinal layer |
|
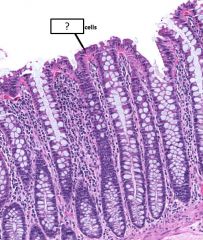
cell - how does the amount of these cells indicate which part of the GI tract it is |
Goblet cells are much more abundant in the large intestine than the small |
|

|
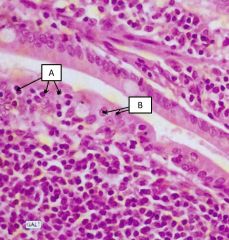
Submucosal (Meissner's) plexus = enteric NS in colon |
|

|
Myenteric (Auerbach's) plexus = enteric NS in colon |
|
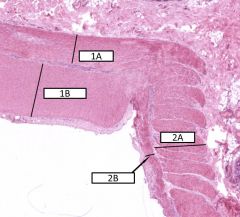
Cross section of the colon - structures and what happening with parts 1 and 2? |
1A - inner circular 1B - outer longitudinal (thicker at this portion because of the tenia coli) 2A - inner circular 2B - outer longitudinal |
|
colon (outer wall) |
Outer portion of the colon wall serosa is lined by mesothelial cells (arrows) |
|
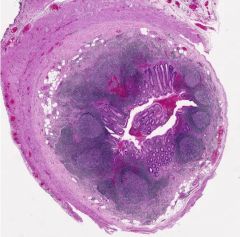
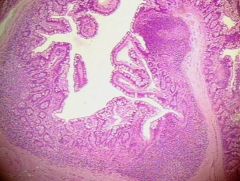
Structure? |
Appendix in a child - note abundant lymphoid tissue |
|
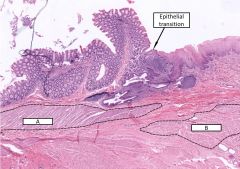
What cells make up A and B? Describe the epithelial transition |
A - internal sphincter - smooth muscle (the last part of the muscularis mucosa in the GI tract) B - external sphincter - skeletal muscle Transition from the invaginating, simple columnar epithelium of the rectum (with lots of goblet cells) to the simple squamous epithelium of the anal mucosa |
|

Anus |
Yellow - serous glands Black - hair follicles Epithelium is keratinized stratified squamous epithelium |

