![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
how do you describe the abdomen in terms of 9 regions?
|

|
|
|
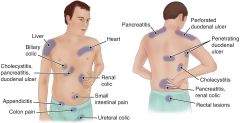
ventral sites of referred pain for:
1.heart 2. renal colic 3. small intestinal pain 4. uretal colic 5. liver 6. bilary colic 7. cholecystitis, pancreatitis, duodenal ulcer 8. appendicitis 9. colon pain |
|
|
|
3 functions of the stomach
|
1. secretes pepsin, renin, lipase, mucus, and HCl for digestion
2. mixes and stores chyme 3. secretes intrinsic factor (necessary for absorption of B12) |
|
|
what is pernicious anemia?
|
deficiency in B12 (because of lack of intrinsic factor)
s/s: parasthesias, tingling, balance, and fall risks. |
|
|
functions of small intestine
|
digest and absorb all amino acids and sugars. (which are transp. to liver via portal vein)
|
|
|
functions of the colon
|
Absorbs fluids and electrolytes
Synthesizes vitamin K using intestinal bacteria Stores fecal material |
|
|
4 functions of the liver (I of II)
|
1. Produces bile (main function), which emulsifies fats and stimulates peristalsis
2. Conveys bile from the gallbladder, where it’s stored, until it enters the duodenum at Oddi’s sphincter through the common bile duct 3. Metabolizes carbohydrates, fats, and proteins 4. Synthesizes coagulation factors (VII, IX, X,) and prothrombin |
|
|
6 more functions of the liver (II of II)
|
1. Stores vitamins A, D, E, K, B12, copper, and iron
2. Detoxifies chemicals 3. Excretes bilirubin 4. Obtains dual blood supply from portal vein and hepatic artery 5. Produces and stores glycogen 6. Promotes erythropoiesis when bone marrow production is insufficient |
|
|
2 functions of gallbladder
|
1. stores bile (90 mL)
2. Mucosa of gallbladder wall absorbs H2O and electrolytes resulting in high concentration of bile salts, bile pigment and cholesterol |
|
|
2 fucntions of the pancreas
|
1. exocrine functions: Amylase: promotes CHO breakdown
Lipase: promotes fat breakdown Trypsin: breaks down proteins 2. endocrine functions: : secretes hormones from the islets of Langerhans a. Insulin: protein hormone promotes storage and utilization of food: primarily glucose and fats b. Glucagon: stimulates glycogenolysis in liver 3. . secretes large amounts of sodium bicarbonate (which neutralizes acid chyme) |
|
|
describe a barium swallow
|
Definition and purpose:
Fluoroscopic procedure using barium as a contrast medium Allows for examination of the pharynx and esophagus after administration of barium Diagnoses hiatal hernia, diverticula and varices Detects strictures, ulcers, tumors, polyps, motility disorders |
|
|
describe nursing interventions before a barium swallow
|
Withhold food and fluids after 6-8 hours
Restricted diet 2-3 days Clear liquid diet 12-24 hours Stop meds 24 hrs. before test Explain the procedure to the patient/remove radiopaque objects |
|
|
describe nursing interventions after a barium swallow
|
Determine if the patient is constipated
Encourage fluids, unless contraindicated Administer laxatives, as prescribed Educate: stools chalky and light colored 2-3 days |
|
|
describe an upper GI series
|
Definition and purpose:
Fluoroscopic procedure using barium as a contrast medium or gastrografin (water soluble contrast medium) Allows for examination of the esophagus, stomach, duodenum, and other portions of the small bowel Gastroesophageal reflux can be assessed during the procedure with client in flat or head down position |
|
|
describe nursing interventions before an upper GI series
|
Withhold food and fluids 6-8 hours/no smoking
Low residue diet 2-3 days Administer clear fluids, cathartics and enemas, as prescribed If Gastrografin is used assess for iodine allergy |
|
|
describe nursing interventions after an upper GI series
|
Inform the patient that stool will be light-colored for up to 3 days
Administer cathartics, fluids, and enemas, as prescribed Assess for partial bowel obstruction. If Gastrografin is used may have significant diarrhea *Contact physician immediately if pt. develops any of the following: difficulty swallowing; epigastric, substernal or shoulder pain; vomiting blood or black tarry stools; or fever |
|
|
describe a lower GI series
|
Definition and purpose:
Fluoroscopic procedure Allows for examination of the large intestine including appendix after administration of a barium enema to visualize anatomic abnormalities including polyps, tumors, Crohn’s disease, fistulas and diverticula |
|
|
nursing interventions before a lower GI series
|
Clear liquid diet day before test/soft low residue diet two days prior
Magnesium citrate/bowel prep night before NPO after midnight Encourage the patient to discuss feelings of embarrassment Administer bowel preparation (laxatives and enemas), as prescribed Assess risk for pregnancy: pelvic exposure Assess ability to turn, hold breath, retain barium* |
|
|
nursing interventions after a lower GI series
|
Determine if the patient is constipated
Encourage fluids, unless contraindicated Administer enemas and laxatives, as prescribed Monitor color and consistency of stool warn pt. of cramps |
|
|
describe Upper GI Endoscopy - Esophagogastroduodenoscopy
|
Definition and purpose:
Procedure using an endoscope Provides direct visualization of the esophagus, stomach, duodenum Detects mucosal inflammations, (reflux, gastritis), tumors, varices, hiatal hernias, polyps, ulcers, and obstruction |
|
|
nursing interventions before Upper GI endoscopy
|
Withhold smoking, food and fluids 6 to 12 hours before the test
Make sure that an informed consent form has been signed Obtain baseline vital signs/assess escort home* Administer sedatives, as prescribed |
|
|
nursing interventions after Upper GI endoscopy
|
Withhold food and fluids until the gag reflex returns (2 to 4 hours)
Assess gag and cough reflexes Assess for signs of bleeding from biopsy site or perforation, dyspnea or dysphagia, aspiration of GI contents |
|
|
3 things that can give you a false positive in Fecal Occult Blood Tests
|
red meat, beets, vitamin C
|
|
|
nursing interventions prior to FOBT
|
-72 hours before test pt. ceases to eat foods that can give a false positive (red meat, beets, vitamin C, etc.)
-7 days before test, pt. stops NSAIDS, ASAs, anticoagulants - teaching about menstruation, toilet bowl cleaners |
|
|
describe the fecal fat test
|
Definition and purpose:
Measures fat content number and size of fat droplets can be determined as well as type of fat excretion. >7gm’s of fecal fat in 24 hrs is abnormal (but non-specific for disease) in stool. Conditions causing fat in stool: CF, Celiac disease, Crohn’s, Diabetes, PUD, Viral Hepatitis, Pancreatic Insufficiency/obstruction |
|
|
describe nursing interventions prior to fecal fat test
|
Advise the patient to restrict alcohol intake and maintain a high-fat diet of 50-150 grams of fat per day for 3 days before examination and during stool collection.
Refrigerate weighed specimen container Document current medications: cimetidine decreases fecal fat Other drugs cause steatorrhea as a result of mucosal damage; colchicine, kanamycin, neomycin, methotrexate Use of herbal laxitives, barium, suppositories, lubricants (sexual) in the perianal area for 3 days before can increase fecal fat |
|
|
what is steatorrhea?
|
improper digestion of fats, usu. due to lack of secretions.
|
|
|
common pathogenic agents found in stool culture
|
Common bacterial pathogens: salmonella, shigella, campylobacter, yersinia, escherichia coli, clostridium and staphylococcus
Common parasitic pathogens: include ascaris(hookworm), strongyloides (tapeworm) Parasites are not cultured, but are identified microscopically in a test called "Stool Ova and Parasites." Protozoan pathogen: giardia |
|
|
how long does a stool culture usually take?
|
Stool culture usually takes 72 hours or longer to complete, but some organisms may take several weeks to grow in a culture.
|
|
|
describe a proctosigmoidoscopy
|
Definition and purpose:
Procedure using a lighted scope either rigid or flexible sigmoidoscope Provides direct visualization for the sigmoid colon, rectum, and anal canal Determines cause of pain and rectal prolapse, blood, pus, mucus in stool Remove hemorrhoids by laser therapy Similar to colonoscopy but less extensive study No BA Swallow or Upper GI in preceding 48 hours |
|
|
nursing interventions prior to proctosigmoidoscopy
|
Encourage the patient to discuss feelings of embarrassment
Inform the patient that the procedure requires a side-lying position Administer bowel preparation, as prescribed, enema HS or AM of test Low residue diet several days, clear fluids evening before (clear liquids for 12 to 24 hours beforehand. A clear liquid diet means fat-free bouillon or broth, gelatin, strained fruit juice, water, plain coffee, plain tea, or diet soda). NPO 8 hours before test No BA Swallow or Upper GI in preceding 48 hours Place obtained written informed consent in the patient’s chart Document iron intake/ no iron 1 wk. before procedure No anticoagulants 14 days before procedure |
|
|
nursing interventions after proctosigmoidoscopy
|
Check the patient for bleeding and signs of colon perforation
Monitor the patient’s vital signs |
|
|
how would you describe a low-residue diet?
|
Low residue diet: low fiber, no skin, no seeds, foods that do not require a lot of mechanical digestion.
|
|
|
describe a colonoscopy
|
Invasive procedure with multi-channel instrument
Allows for: direct visualization (and biopsy/excision of small tumors/polyps of the large intestine from anus to cecum, insufflation of air, aspiration of fluid, passage of laser beam for obliteration of tissue and control of bleeding. Contraindications: uncooperative pt., medically suspected colon perforation |
|
|
nursing interventions prior to a colonoscopy
|
Encourage the patient to discuss feelings of embarrassment
Inform the patient that the procedure requires a side-lying position Administer bowel preparation, as prescribed, enema HS or AM of test Low residue diet several days, clear fluids evening before (clear liquids for 12 to 24 hours beforehand. A clear liquid diet means fat-free bouillon or broth, gelatin, strained fruit juice, water, plain coffee, plain tea, or diet soda). NPO 8 hours before test No BA Swallow or Upper GI in preceding 48 hours Place obtained written informed consent in the patient’s chart Document iron intake/ no iron 1 wk. before procedure No anticoagulants 14 days before procedure (same as sigmoidoscopy) |
|
|
nursing interventions after colonoscopy
|
. Post: after the procedure, monitor for gross bleeding, expect slight rectal bleeding for 2 days after removal of polyps or biopsy specimens.
|
|
|
risk factors for colorectal cancer
|
1. age over 50
2. colorectal polyps 3. family history of colorectal cancer 4. genetic alterations 5. personal history of colorectal cancer (also women with overian, uterine, or breast cancer) 6. ulcerative colitis or crohn's disease 7. diet (high fat, low fiber) 8. cigarette smoking |
|
|
colonoscopy: teach pt. to contact physician immediately if....
|
experience severe abdominal pain, fever, bloody bowel movements, dizziness, or weakness afterward.
|
|
|
what is a vasovagal reaction and what are the nursing interventions?
|
Vasovagal reaction: dropping bp, slowing HR.
Interventions: open IV, trendelenberg position, |
|
|
describe the gastric acid stimulation test
|
Used to determine response to substances administered to induce gastric acid production.
Pentagastrin is usual drug of choice to induce gastric acid, pepsin, intrinsic factor production Basal and then peak samples are examined for volume, ph and amount of acid secreted Aspiration of the contents of the stomach through an oral/nasogastric (NG) tube, specimen collection takes 60-120 minutes. Peak specimens are collected over 60 mins. as four 15 min. specimens Used to differentiate causes of hypergastrinemia including Zollinger-Ellison Syndrome (elevated levels of gastrin from pancreatic tumor) gastritis, peptic ulcers,) Most often used to assess the effect of antiulcer therapy |
|
|
nursing interventions before the gastric acid stimulation test
|
Withhold food after evening meal, water 1 hr. before the test Avoid exposure to sight, smell, thought of food before and during test
Instruct the patient not to smoke/chew gum 12 hours before the test Withhold medications that can increase gastric secretions for 72 hours before the procedure: ETOH, nicotine, steroids, |
|
|
nursing interventions after gastric acid stimulation
|
Obtain the patient’s vital signs
Note reactions to gastric acid stimulant |
|
|
nursing interventions prior to ultrasonography
|
Withhold food and fluids for 8 to 12 hours before the procedure
Determine the patient’s ability to lie still during the procedure Ask the patient not to smoke or chew gum for 8 to12 hours before the test Administer enemas, as prescribed Remove abdominal dressings |
|
|
key symptoms of a GI disorder
|
Weight changes
Rectal bleeding Jaundice Hematemesis nausea vomiting anorexia |
|
|
assessment findings of appendicitis
|
Abdominal pain, generalized or localized in the right upper abdomen, eventually localizing in the right lower abdomen (McBurney’s point)
Anorexia Nausea and vomiting Board-like abdominal rigidity Retractive respirations Rebound tenderness: refers to pain upon removal of pressure rather than application of pressure to the abdomen. Low-grade fever (late sign) Constipation (although diarrhea is also possible) Tachycardia Sudden cessation of pain (indicates rupture) |
|
|
diagnostic test findings of appendicitis
|
White blood cell (WBC) count is moderately elevated, with increased immature cells.
Ultrasound of the abdomen and pelvis shows a non-perforated, inflamed appendix CT scan: abscess or enlarged appendix |
|
|
nursing interventions for appendicitis
|
Withhold food and fluids
Administer I.V. fluids/ensure IV access Assess GI status and fluid balance Maintain position, patency, and low suction of NG tube Keep the patient in low Fowler’s position Monitor and record vital signs, I/O, and laboratory studies Administer medications: antibiotics/analgesics Allay the patient’s anxiety verbally and with medications Maintain bed rest Never administer cathartics or enemas because they may rupture the appendix Never apply heat to the right lower abdomen; this may cause the appendix to rupture Individualize home care instructions: Follow activity restrictions Recognize signs and symptoms of infection |
|
|
interventions for periotonitis secondary to appendix rupture.
|
treatment involves GI intubation, parenteral replacement of fluids and electrolytes, and administration of antibiotics
|

