![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
Luminal defense and Epithelial barriers make up the _______ immunity of the GI tract.
Describe luminal factors that protect the gut. |
Innate Immunity (First line of defense)
Non-immunologic mxns= lysozyme, HCl, digestive enzymes of pancreas, bile detergents. Intestinal motility and mucous secretion. Colon- host flora, antibacterial peptides (colcins), acidic pH, anaerobic environment. |
|
|
What are the two most important components of the Epithelial barrier/
|
1. Intercellular tight junction complexes (regulate transport of particles and solutes)
2. Epithelial cells ( regulate transport across cell, contain Defensins and anti-microbial peptides) |
|
|
What are the 4 major cell types of the Epithelial Barrier?
What is the mot important cell of the Epithelial Barrier? |
Epithelial cells, Goblet cells, M cells (microfold), Paneth cells
Most important = Epithelial Cell (it secretes IgA, transduces signal from lumen, signals APCs and expresses MHC I & II so it can stimulate immune system by itself). |
|
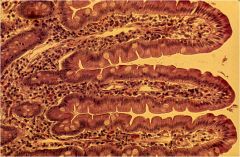
What 3 things do the white cells shown in this image produce that protect against foreign particles?
|
Goblet cells--
1. Mucin glycoprotein 2. Trefoil peptides (antimicrobial, activate NFkB and stimulate EGF receptors, aids in defense). 3. Beta Defensins (pro-inflammatory cytokines, ex: TNF and IL1-b) |
|
|
What special property of Epithelial cells help them clear cytotoxins?
What is the role of Cathelcidins? |
EC has Multidrug resistance gene (eliminates toxic intra-cytoplasmic substances).
Cathelcidins = expressed by PMNs & EC, can neutralize LPS of gram negative bacteria. |
|
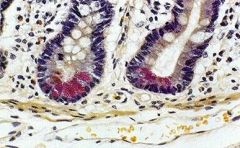
What is the role of the pink cells shown here? Where are they located?
Why do they stain pink? |
Paneth cells- innate immune system. Located at base of small intestine crypts.
Eosinophilic as a result of granules that they release (alpha defensins, beta defensins) |
|
|
What is the role of the ZOT toxin? In what infectious agent does it exist?
What compound implicated in Celiac disease, works in a similar way? |
ZOT = Cholera B toxin (opens tight junctions allowing bacteria to penetrate lamina propria). *Zonulin occludens toxin, disrupts polymerization of actin)
Celiac disease = gliadin (glides in, acts similar to Cholera B) |
|
|
Role of Dendritic cells in defense?
|
Dendritic cells = APCs that lie beneath EC. Sample intestinal environment by sending cytoplasmic projections through tight junctions. Present antigen to T-cell and help activate it.
|
|
|
Where in the GI tract do intestinal macrophages reside?
What lineage are NK cells derived from? What do they secrete? What is their role in self-recognition? |
Macrophages= Peyer's patch, Kupffer cells of liver, and mesenteric nodes
NK cells- from lymphocytic lineage. Secrete INF-g (potent activator of macrophages). Recognize MHCI cells with KIR (killer inhibitor receptor) and inhibit cytotoxicity. |
|
|
What are the four components that make up GALT?
|
Gut associated lymphoid tissue =
Lymphatic tissue, Lamina propria, Intraepithelial Lymphocytes (IELs), and Mesenteric Lymph Nodes |
|
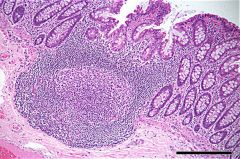
Where do you see most of the structures shown above? What is the function of these structures?
What is the function of the cells found within the surface folds called? |
In small intestine (ileum). Some smaller ones in colon as well.
They are a sampling station for antigens. There are no crypts or villi, instead M-cells (microfold) are there are and they take up antigen and present it to the APCs and macrophages. |
|
|
A mixture of inflammatory cells (T, B, macrophage, NK, eosinophils, mast, etc) are found in the _______ of the GALT.
What is the role of MadCAM-1 in T-cells? |
Lamina propria
MadCAM1 = ligand that binds to T-lymphocyte homing receptor α4β7, and directs CD4+ T cells back to the GALT tissue (specifically to the high endothelial venules that they then enter). *remember, T lymphocytes, once activated leave the peyer's patch, go to mesenteric lymph node and activate B cells, then go through lyphatic and systemic circulation and enter back in to the GALT. |
|
|
In what conditions might you see eosinophils in the lamina propria?
Where are mast cells localized within the lamina propria? How are they stimulated and what do they release? |
Helminthic disease, eosinophilic syndromes. (NAACP)
Mast cells (localized to nerve terminals). Stimulated by IgE and Substance P (neuropeptide). Release histamine, serotonin, proinflammatory cytokines. |
|
|
The plasma cells in the lamina propria mostly secrete what immunoglobulin?
Th-17 cells have been implicated as being important in what GI disease? |
IgA mostly (some IgM) *note, secretory IgM helps protect those who are deficient in IgA
Th-17 = new line of cells, important in IBD (inflammatory bowel disease) |
|
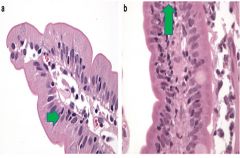
What cells can you make out in this image? How are they distinguished from lymphocytes?
Increased numbers of these cells in the colon have been implicated in __________. Increased numbers of these cells in the small intestine have been implicated in ________. |
Intraepithelial lymphocytes (larger than usual lymphocytes, and they lie between epithelial cells)
Too many IELs in small bowel = Celiac disease Too many IELs in the colon = Lymphocytic colitis |
|
|
What is the role of intraepithelial lymphocytes? Most IEL's are CD___+?
|
They are both cytotoxic and immunoregulatory. Mostly they are CD8+ (suppressor/ cytotoxic type).
|
|
|
What are the largest lymph nodes in the body?
How are lymphocytes directed to peripheral lymph nodes? to mucosal tissues? |
Mesenteric lymph nodes (they serve as an area for dendritic cells to encounter and activate T and B cells, the T cells then pass through circulation and enter MALT).
α4β7 directs to mucosal tissue L-selectin directs to peripheral lymph nodes |
|
|
What is the structure of the principal antibody in intestinal mucosal secretions?
Where is the sIgA receptor found? |
Secretory IgA --> dimer containing two IgA's linked by a J-chain. *note, there are 2 subclasses, IgA1 and IgA2
sIgA receptor in intestines, biliary tract, lactating breast (provide initial IgA protection to neonate), saliva, and sweat. |
|
|
Describe how IgA becomes secretory IgA.
|
IgA is taken up by poly-Ig receptor (basolateral surface of epithelial cell). The receptor binds the J-chain.
IgA is endocytosed, transported in vesicle to lumen, and receptor is cleaved leaving reusable transmembrane portion. |
|
|
What is the difference in structure between serum and secretory IgA?
Which subtype is more commonly found in serum? What is the major source of Serum IgA vs. Secretory IgA? |
Serum IgA = monomeric (vs. sIgA which is dimeric)
Serum IgA is made in the bone marrow and IgA1 is most common subtype *note sIgA is made mostly in intestine and IgA2 is most common subtype |
|
|
How does IgA aid in defense?
|
Enhances non-specific defense (lactoferrin, lactoperoxidase). It inhibits Bacterial adhesion, neutralizes toxins.
Note- not a potent activator of complement |
|
|
A lymphocyte can become one of what three choices?
What is central vs. peripheral tolerance? |
Tolerance, Ignorance (no response from lymphocyte), or Activation (full response)
Central tolerance = immature lympho develop when they encounter antigens in thymus and BM Peripheral = MATURE lympho encounter antigen in PERIPHERY |
|
|
Would you expect an increased immune response to someone who was fed a soluble protein antigen and then received it systemically or someone who received an antigen systemically without being fed?
|
Feeding a soluble antigen beforehand reduces the immune response when the antigen is injected later on.
|
|
|
Name two inhibitory cytokines secreted by T-regulatory cells.
Besides T-regs, what are other key cell players of tolerance? |
IL-10 and TGF-B = inhibitory cytokines
CD8+ suppressor cells, IELs (have both cytotoxic and immunoregulatory function, and Myeloid derives suppressor cells (MDSCs = macrophages) |
|
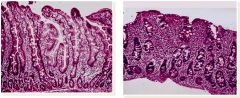
What are the three characteristic changes seen on the right histologic specimen (left is normal)?
What is the disease? |
Celiac disease=
1. Villous atrophy, 2. Crypt Hyperplasia, 3. Increased IEL's (seen as increase in blue staining cells) |
|
|
Describe the pathogenesis of Celiac disease (what happens when a patient eats wheat?)
|
Wheat/Rye/Barley --> gliadin --> able to glide through epithelium because of increased intestinal permeability --> encounters TTG which activates gliadin (deaminates it) --> this binds to HLADQ2/8 --> stimulates T and B cell release
You get antibodies to Tissue Transglutaminase |
|

A patient is having weight loss, abdominal pain, and diarrhea. They have developed a papular vesicular rash on their extensor surface that is incredibly itchy. What is the treatment?
|
Patient is having malabsorption from celiac disease. This is associated with Dermatitis herpetiformis.
Gluten free diet & dapsone (for the skin condition) |
|
|
How do you test for Celiac disease? What concomitant test should you order?
|

1st- serum Ttg antibody test (usualyl ELISA) = most cost effective. (serum antibody to IgA endomysial is $$$$)
*always get an IgA level (because IgA deficiency is common in these patients so you want to make sure IgA ttg isn't falsely low) 2nd- endoscopy with a biopsy (because false positive serology can occur) |

