![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
What is Cirrhosis?
What are some of the etiologies (there are many...) |
Final common histologic appearance of liver due to chronic end-stage liver disease.
Etiologies: Viral (Hep B,C) NAFLD Alcoholic Liver Disease Autoimmune liver disease Metabolic (A1AT, Cu, Fe) |
|
|
T or F
Diagnosis of cirrhosis requires biopsy of the liver. T or F Knowing the etiology of the cirrhosis is important in late stage of disease. |
False- sometimes, if there is clear evidence (clinical, labs, and macronodules that can be felt on physical exam) don't need to biopsy.
False- in late stage of disease, etiology doesn't change management. But it can early on (can prevent progression) |
|
|
What is the progression of Cirrhosis (i.e. where does it start and where does it reach in most severe phase)?
What is the "limiting plate"? |
Starts in Portal region --> progress to Periportal region--> goes beyond the limiting plate --> into parenchyma
Limiting plate = ring of hepatocytes abutting the connective tissue of the portal trial |
|
|
What are some physical exam findings suggestive of cirrhosis?
What are some signs of decompensation? |
- palpable left lobe of liver
- shrunken, small liver; nodular - Splenomegaly Decompensation - Jaundice, Ascites, Asterixes (flapping tremor) |
|

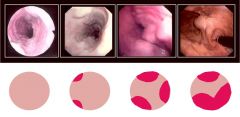
Name the following signs of chronic liver disease and STAGE 1 Cirrhosis.
|
Spider nevi (that blanch if you press on center), White nails, Palmar erythema (can be seen normally in pregnant women), and Gynecomastia
*note: unclear as to why, but cirrhosis is associated with elevated estrogen levels (there is excess aromatization of Androsteindione to E2 --> testicular atrophy, impotence, gynecomastia). |
|

Name the following signs of chronic liver disease and STAGE 2 Cirrhosis. In what kinds of conditions would we see them?
|
Kaiser Fleishcher ring- deposition of copper in Descemet membrane (around cornea) -- Wilson's disease
Xanthelasma or Xanthomas - especially seen in cholestatic disease, ex: Primary Biliary Cholangitis |
|

What signs of chronic liver disease are seen here (STAGE 4 cirrhosis)?
|

Caput Medusae (dilated abdominal wall veins), and Ascites. Muscle wasting (from poor nutrition).
Hyperestrogenemia also causes loss of body hair. *note above: Dupuytren's contractures (of palmar aponeurosis- associated with Stage 3 Cirrhosis) |
|
|
What lab findings are suggestive of cirrhosis?
What imaging studies would you use to test for cirrhosis? |
LFTs might be elevated (AST/ALT > 1 especially seen in Alcoholic Liver Disease)
- ↓ albumin, ↑ PT/INR, ↑ bilirubin - Thrombocytopenia (↓ platelet count from splenomegaly) U/S (fluid in liver), CT belly (shows shrunken liver, enlarged spleen, venous collaterals). Nuclear studies (show uptake of radiolabled colloid) |
|
|
Which of the following statements are true about cirrhosis?
A. Understanding the etiology of late disease may dramatically alter management B. Understanding the etiology of early disease may dramatically alter management C. There is little value to confirming the diagnosis of genetically inherited disease process in late stage disease D. Most cirrhosis in the US is caused by unknown causes |
B. Understanding the etiology of early disease may dramatically alter management
*may decrease the progression of disease |
|
|
Which of the following statements about Cirrhosis are true?
A. Cirrhosis can only be diagnosed by liver biopsy B. Liver function tests can help determine the etiology of cirrhosis C. Cirrhosis represents a group of physical and laboratory findings that are final pathway for numerous chronic liver diseases D. Physical findings in cirrhosis are unique to cirrhosis and not seen in other diseases |
C. Cirrhosis represents a group of physical and laboratory findings that are a final pathway for numerous chronic liver diseases
|
|
|
What does the Child-Pugh classification system tell you? What about MELD?
|
Child-Pugh --> gives you 2-year survival scores (based on presence of ascites, encephalopathy, bilirubin, PT (INR), albumin)
MELD --> algorithm that predicts 3 year mortality (uses numbers, bili, INR, creat) |
|
|
Most forms of cirrhosis will eventually progress to HCC (hepatocellular carcinoma) except ______.
What are some complications of portal hypertension? |
Wilson's disease (doesn't tend to progress to HCC)
Varices (distended veins), Ascites, bacterial peritonitis, Hepatorenal syndrome (HRS), and Hepatopulmonary syndrome |
|
|
What makes up the blood supply TO the liver? What is the pressure of each component of this system?
What three things make up the bile duct? Ischemic insult to the liver will most affect what zone of the liver? |
Portal vein (2/3rd of inflow, low pressure 7 mmHg), and Hepatic artery (1/3rd of inflow, high pressure 100 mmHg).
Portal triad = Hepatic artery + Portal vein + Bile Duct. Ischemic injury will affect region near central vein, i.e. Zone 3, (because it is farthest away) from the portal triad. |
|
|
2 Formula's for portal blood flow:
Ohm's law Poiseuille's law |
Ohms ΔP = F x R (flow x resistance)
Poiseuille's R = 8nL / πr^4 |
|
|
How does portal hypertension develop?
|
1. Increased Resistance to portal flow (fibrosis, active vasoconstriction)
2. Increased inflow from portal veins (splanchnic vasodilation --> low effective blood volume --> activation of Renin/Ag --> plasma volume expansion |
|
|
Portal hypertension is contributed to by which of the following?
A. Decreased resistance to portal flow B. Hepatic vascular endothelial vasodilation C. Splanchnic vasoconstriction D. Increased portal venous inflow |
D. Increased portal venous inflow
*remember, increased resistance to portal flow, hepatic vascular VASOCONSTRICTION, and splanchnic VASODILATION will lead to increased venous inflow |
|
|
Contributors to decreased effective circulating blood volume in cirrhosis include:
A. Portosystemic shunts B. Endotoxemia C. Increased splanchnic and systemic NO synthesis D. Splanchnic dilation E. All of the above |
E. All of the above
Portosystemic shunt, Endotoxemia/Bacteria, Increased splanchnic NO synthesis, splanchnic dilation --> can cause low splenic effective blood volume (leading to volume expansion). |
|
|
Give and example of each of the following:
1. Pre-sinusoidal 2. Sinusoidal 3. Post-sinusoidal 4. Post-hepatic |
1. Pre-sinusoidal: Extrahepatic = portal vein thrombosis, compression. Intrahepatic = sarcoid, PBC
2. Sinusoidal: cirrhosis, alcoholic hepatitis 3. Post-sinusoidal: Budd Chiari syndrome, VOD (veno-occlusive disease) 4. Post-hepatic: Congestive heart failure, Restrictive cardiomyopathy (R-sided pressure --> back pressure) |
|
|
How do you measure Portal Hypertension (pressure)?
How can you use this to determine if a patient's varices will bleed? |
Do a wedge pressure (within the hepatic veins)= WHVP
and a Free hepatic venous pressure (i.e. hepatic veins leading to IVC) = FHVP HVPG (Hepatic venous pressure gradient) = WHVP - FHVP HVPG >12 = varices may bleed |
|
|
What is the WHVP, FHVP, and HVPG (hepatic venous pressure gradient) in the following types of portal HTN-
Pre-hepatic Pre-sinusoidal Sinusoidal Post-sinusoidal Post-hepatic |
Pre-hepatic = all normal
Pre-sinusoidal = all normal Sinusoidal = ↑ WHVP, normal FHVP, ↑ HVPG Post-sinusoidal = ↑ WHVP, normal FHVP, ↑ HVPG Post-hepatic = ↑WHVP, ↑FHVP, normal HVPG (because it cancels out) |
|
|
How does portal HTN lead to the development of varices?
What is the danger of GE (gastroesophageal varices)? |
Portal HTN --> high volume, and high pressure blood tries to go through past of least resistance.
Flows through portal-systemic collaterals where blood pressure is lowest (may recanalize embryonic veins leading to caput medusae, or cause GE varices). GE varices can bleed --> mortality |
|
What action would be appropriate if you found no evidence of varices on upper endoscopy?
What if someone had a grade I (2nd panel) varices? |
No varices--> do EGDs every 2-3 years (or ever year if decompensated)
Grade I varices --> Primary prophylaxis (medications such as B-blockers, nitrates) |
|
|
How do meds such as propranolol and nadolol work to treat GE varices?
|
↓ portal pressure --> ↓ variceal wall tension and less likely to bleed
Non-cardiospecific B- blockers --> block splanchinc vasodilation (B2) causing arteriolar vasoconstriction. Decrease portal inflow. Block cardiac receptors (B1) --> leading to ↓ heart rate and cardiac output. Decrease portal inflow. |
|
|
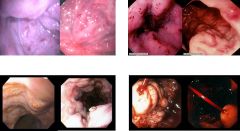
How do nitrates help in portal hypertension?
What procedure is shown above and for what grade of esophageal varices would it be appropriate? |
Nitrates- non liver specific VENODILATORS, decrease MAP (can ↑ mortality if used alone)
This is Banding (or endoscoping ligation)- basically chocking the varix with a band till it necroses. Used in Grade 2-3 varices or in case of Acute bleed. |
|
|
What are different procedural (non-pharmacologic) ways that you can treat a bleeding varices?
|
- temporary balloon tamponade (the helmet technique where you blow up balloon and use it to compress vessel in stomach).
- endoscopic sclerotherapy - esophageal variceal (band) ligation - Splenorenal shunt (join splenic vein to left renal vein, ↓ pressure in portal system)- controls bleeding in 90% of patients |
|
|
What is TIPSS?
How do somatostatin analogs and Vasopressin help decrease risk of bleeding varices? |
TIPSS = IR procedure (transjugular intrahepatic photosystemic shunt). Shunt put between hepatic vein and portal vein. ↓ Pressure in portal system.
Somatostatin analog (Octreotide)- inhibit GI hormones (VIP, gastrin, etc.) that normally cause splanchnic vasodilation. Vasopressin - vasoconstriction (give with NTG because it can constrict the heart blood vessels as well). |
|
What do the following endoscopic signs have in common?
|
They are "Red signs" (predictors of variceal bleeding)- ex: Red wale sign, Cherry Red spots, Mamilla sign (platelet plug), and Active bleed
|
|
|
Therapy for esophageal varices involves:
A. Agents that increase portal inflow B. Agents that increase the HVPG C. Nonselective beta-blockers which lead to splanchnic arteriolar vasoconstriction and decrease in portal inflow D. Nitrates which increase MAP and portal inflow |
C. Nonselective beta blockers which lead to splanchnic arteriolar vasoconstriction and decrease portal inflow
|
|
|
Therapy of bleeding esophageal varices may include:
A. Balloons which directly compress the blood vessels B. Octreotide which blocks hormones which cause splanchnic vasoconstriction C. Vasopressin analogues/vasoconstrictors D. Endoscopic techniques to stop bleeding E. All of the above |
E. All of the above
|
|
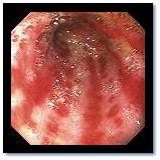
What is this condition? Where in the body is it seen?
|
Gastric antral vascular ectasia (GAVE)- i.e. Watermelon stomach. Dilated blood vessels seen in the stomach.
Can be a result of portal hypertension. Tends to be localized in the ANTRUM of the STOMACH. |

