![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
Why should only life threatening injuries in a multitrauma patient be repaired acutely?
|
Trauma is associated with a surge in inflammatory mediators, which peak 2 to 5 days after trauma. leukocytes are “primed” and can be activated easily with further trauma, such as surgery. This may lead to multisystem organ failure or ARDS.
|
|
|
What are some examples of injuries that should be stabilized acutely in severe polytrauma? How is acute stabilization primarily accomplished? (bold)
|
Compartment syndrome, fractures associated with vascular injury, unreduced dislocations, long bone fractures, open fractures, or unstable spine fractures should be stabilized acutely.
Acute stabilization is achieved primarily via external fixation. |
|
|
What are the clinical hallmarks of compartment syndrome?
|
Pain out of proportion to the injury and pain with passive stretching of the muscle.
Pulselessness, parasthesias, and pallor are late findings. |
|
|
Intracompartmental pressure measurements are abnormal at what level? (bold)
How are intraoperative pressures changed (bold)? |
If pressure is within 30 mm of the diastolic pressure (ΔP) or greater than 30 mm of the absolute pressure (the criteria are debated).
Intraoperative diastolic blood pressure during anesthesia is approximately 18 mm Hg lower than “baseline,” potentially giving spurious ΔP values |
|
|
How quickly does neurapraxia from stretch injury recover?
|
Approximately 1mm per day
|
|
|
What nerve has the worst prognosis of partial recover after repair?
|
Peroneal
|
|
|
What bacteria are specifically associated with the following types of bites, although staph and strep are still the most prevalent pathogens?
Cat Dog Human |
Cat - Pasteurella
Dog - Eikenella Human - many (including Eikenella) |
|
|
In a patient with multiple knee ligaments injured following a trauma, what should you suspect and what should your first test be?
|
Suspect knee dislocation and be sure to get ABIs
|
|
|
A reverse arthrocentesis/saline load test can be performed to test for a penetrating injury to a joint and is performed by injecting saline into the joint and observing the injured area for signs of extravasation. What is the minimum amount that must be injected into the knee?
|
At least 155mL must be injected into the knee
|
|
|
What is the most common grading system for open fractures? Describe the grades
|
□ Type I—no periosteal stripping, minimum soft tissue damage, small skin wound (1 cm)
□ Type II—little periosteal stripping, moderate muscle damage, skin wound (1-10 cm) □ Type IIIA—contaminated wound (high-energy gunshot wound, farm injury, shotgun) OR extensive periosteal stripping with large skin wound (>10 cm) □ Type IIIB—same as IIIA but will require flap coverage □ Type IIIC—same as IIIA but with vascular injury that requires repair |
|
|
What is the initial treatment of open fractures?
|
Antibiotics and Debridement
|
|
|
What type of antibiotic is used in the following types of open fractures?
- Type I & II - Type III - Heavily contaminated and farm wounds -Fresh water wounds -Salt water wounds |
Types I and II—first-generation cephalosporin (cefazolin) for 24 hours
Type III—cephalosporin and aminoglycoside for 72 hours AFTER LAST INCISION AND DRAINAGE Heavily contaminated wounds and farm wounds—cephalosporin, aminoglycosides, and high-dose penicillin Fresh water wounds—fluoroquinolones (ciprofloxacin, levofloxacin) or third- or fourth-generation cephalosporin (ceftazidime) Salt water wounds—doxycycline and ceftazidime or a fluoroquinolone |
|
|
What is the goal for timing of coverage of soft tissue of open fractures?
|
Early coverage (<5 days is the goal). However, zone of injury must be well defined before coverage
|
|
|
What type of flap is used for the following open fracture?
Proximal third of the tibia |
Gastroc
|
|
|
What type of flap is used for the following open fracture?
Middle third of the tibia |
Soleus
|
|
|
What type of flap is used for the following open fracture?
Distal third of the tibia |
Free tissue transfer
|
|
|
What type of fractures can external fixation be used for definitive treatment?
|
External fixation may be used definitively for periarticular fractures, articular fractures that cannot be reconstructed, and segmental fractures, but internal fixation is far more common
|
|
|
What are the hallmarks of fat embolus syndrome which is associated with reaming of long bones but can occur with any long bone fracture?
|
Hypoxia, petechial rash on the chest, and tachycardia
|
|
|
What are the 2 types of external bone stimulators and how do they work?
|
Ultrasound—delivers small, cumulative doses of ultrasound energy; thought to induce microfracture and healing response
Electromagnetic—attempts to promote healing by directing integral ion flow at cellular level of bone |
|
|
What are the classifications of nonunions?
|

|
|
|
What are the 4 treatments for segmental bone loss?
|
treatment with bone graft, interposition free tissue transfer (free-fibula transfer), bone transport (Ilizarov or Taylor spatial frame), and amputation
|
|
|
What can be used as prophylaxis for heterotopic ossification?
|
Indomethacin 25 mg orally three times a day or indomethacin (sustained release) 75 mg orally daily for 6 weeks may be effective in preventing heterotopic bone formation
|
|
|
How much radiation is required if using radiation for heterotopic ossification?
|
Radiation therapy (600-700 cGy) given 24 hours before or up to 72 hours after surgery
|
|
|
How can fractures caused by low-energy gunshot wounds be treated?
|
Can be treated as a closed fracture but should get single-dose, first-generation cephalosporin and local wound care
|
|
|
What determines the strain in fracture healing?
What determines type type of healing? |
Stability determines the strain
Strain determines the type of healing |
|
|
What leads to callus formation with healing bone?
How does a maturing callus change strain and stability? |
Micromotion at the fracture site under physiologic load
Strain decreases as callus matures, leading to increased stability |
|
|
What happens if too much motion is present at a fracture site?
|
If there is too much motion, callus becomes hypertrophic as it tries to spread out force and hypertrophic nonunion can result.
|
|
|
What are 4 examples of fixation that leads to relative stability and callus formation at the site of fracture?
|
Casts, External Fixators, IM nails, Bridge plates
|
|
|
What is the difference between relative and absolute stability with fracture healing? How does the healing differ?
|
Relative stability has micromotion at the fracture site. Absolute stability has no motion at the fracture site under physiologic load
With relative stability, micromotion leads to callus formation; With absolute stability bone heals through direct healing and there is no callus. Strain is low or zero with absolute stability |
|
|
Which takes longer to heal, absolute or relative stability?
|
Healing times are longer with absolute stability and are more difficulty to confirm by radiography. Implants must have longer fatigue life
|
|
|
What are 3 examples of absolute stability implants?
|
Lag screws, Compression plates, and rigid locked plates (in nonbridging mode)
|
|
|
What are the differences in healing of diaphyseal (cortical) and cancellous (metaphyseal) fractures? Which heals more rapidly? Which has a lower strain? Which is more amenable to compression techniques?
|
1. Diaphyseal (cortical)
▪ Decreased blood supply leads to longer healing times. ▪ Bone is more amenable to compression techniques (in short oblique/transverse fractures). ▪ Strain is concentrated over a smaller surface area. 2. Cancellous (metaphyseal) ▪ Larger surface area and better blood supply ▪ Strain is lower as forces spread out over larger area. ▪ Healing is more rapid. ▪ However, joint surfaces tolerate very little malreduction (<2 mm) so there is often increased time to weight bear versus diaphyseal fractures. |
|
|
Lag screws provide what type of stability?
Why is a plate typically needed to protect/neutralize the deforming forces of a lag screw? |
Lag screws provide rigid interfragmentary compression (abssolute stability).
Force is concentrated over a small area (around the screw) |
|
|
What type of screw compresses a plate to bone but does not provide interfragmentary compression?
|
Position screws. Friction between screw, plate, and bone resists pullout or bending
|
|
|
As far as bending stability is concerned, which matters more, plate length or number of screws?
What is important for torsional stability? |
Plate length
Position of the screw is important for torsional stability (need end hole filled) |
|
|
How do longer plates affedt strain?
Are plates load bearing? How does this affect stress shielding and why is this important to know if the plate is removed? |

Longer plates spread the strain over a greater area (increased working length)
Yes, plates are load bearing. The area that is covered by the plate is stress-shielded and it would be important to protect this area if a plate had to be removed |
|
|
When properly applied, what type of stability does a compression plate provide?
|
The plate design (oval holes) or use of a compression device allows compressioin plates to apply compression across a fracture. When properly applied, this provides absolute stability
|
|
|
How does the fact that compression plates rely on friction between the plate and bone affect the type of screws that should be used?
|
These plates need at least some nonlocking screws
|
|
|
How would you eliminate gapping opposite a compression plate?
|
Pre-bending
|
|
|
What is the insertion order for the screws of a compression plate?
|

1. Neutral position
2. Compression on opposite side of the fracture 3. Lag screw (if placing through plate) |
|
|
What does tight contact of a compression plate to bone when initially applied cause?
|
Decreased periosteal blood flow and temporary osteopenia
|
|
|
Bridge plating is made primarily for what types of fractures?
What type of stability does bridge plating provide? |
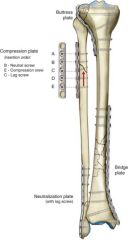
Primarily for comminuted fractures. The plate bridges the comminution with fixation above and below the fracture
Provides relative stability |
|
|
Should screws be placed close to the fracture with bridge plating?
What is the difference between nonlocking and locking screws with bridge plating techniques? |
No, screws should not be placed close to the fracture.
Nonlocking screws compress the plate to bone so can be used to lag in fragments. Locking screws provide angular stability in short metaphyseal segments or in osteoporotic bone |
|
|
What type of plating is typically used with depressed metaphyseal/articular fractures that have been reduced and why?
What type of stability is provided to metaphyseal fragments? |
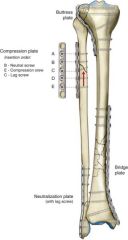
Buttress plating. This provides support at 90 degree angle to the fracture
Can provide absolute stability to metaphyseal fragments |
|
|
What type of plating can be used to preserve biology at the fracture site by avoiding exposure of the fracture site leading to decreased soft tissue and biologic compromise and preserving more of the blood supply?
What mode is typically used (though not absolutely required) and what is the disadvantage of using this technique? |
Submuscular/percutaneous plating. This is typically used with bridge mode
The disadvantage is this is more prone to malreduction/malrotation |
|
|
In locked plating the screws have threads that fit into corresponding threads on the plate. How does this change the failure pattern?
|
These fail simultaneously rather than sequentially
|
|
|
What is the difference in the friction component of locked and non-locked plates?
|
Locked plates do not rely on friction between the plate and the bone for stability. Locked plates provide a fixed angle construct similar to blade plates
|
|
|
What type of plating is most useful in unstable, short segment metaphyseal fractures and osteoporotic bone?
|
Locked plating
|
|
|
What type of fracture patterns are specifically supported by data for the use of locked plates? (bold)
|
Periprosthetic fractures
Proximal humeral fractures Intraarticular distal femur and proximal tibia Humeral shaft nonunion in the elderly |
|
|
Unicortical locked screws are typically used for what type of bone? How does pullout strength compare to bicortical locked screws in good quality diaphyseal bone?
|
Typically used in metaphyseal bone.
Pullout strength is similar to bicortical locked screws in good quality diaphyseal bone, but indications for use there are limited. |
|
|
How does torsional strength between unicortical locked and bicortical locked screws compare? (bold)
What is the biggest advantage for use of bicortical locked screws? |
Unicortical locked screws are weaker in torsion
Biggest advantage for use of bicortical locked screws is in oseoporotic diaphyseal bone |
|
|
Multiaxial screws may provide increased options for fixation when working around what type of fracture? Is there any advantage in pullout or strength
|
Increased options with periprosthetic fractures. No advantage in pullout or strength
|
|
|
What is the term for use of both locking and nonlocking screws in combination? (bold)
What advantage does this technique provide? |
Hybridization. It allows for both compression and fixed-angle support
|
|
|
Do IM nails provide absolute or relative stability?
|
These are load-sharing devices, they provide relative stability
|
|
|
What 3 properties determine the stiffness of an IM nail?
|
Material, size, and wall thickness
|
|
|
Which is greater for increased stiffness of an IM nail, stainless or titanium?
Increased diameter leads to increased stiffness in an IM nail at a ration of radius to the power of what in bending and torsion How does a larger wall thickness change the stiffness of an IM nail? |
Stainless is greater than titanium
Radius to the power of 3 in bending and 4 in torsion Larger wall thickness --> Stiffer nail |
|
|
How does the radius of curvature of a femoral nail compare to the anatomic radius of curvature? (bold)
What effect would a large mismatch of radius of curvature between a femoral nail and the anatomic have? |
The radius of curvature is typically less than anatomic which leads to improved frictional fixation
A large mismatch of curvature leads to difficult insertion, increased risk of intraoperative fracture, and malreduction in extension |
|
|
Nails resist which deformity very well? Interlocks are required to resist what deformities?
|
Nails resist bending very well. Interlocks are required to resist torsion and compression
|
|
|
What is the definition of working length of a nail? (bold)
How could increased working length of a nail lead to delayed union? |
The portion of a nail that is unsupported by bone when loaded
Increased workign length leads to increased interfragmentary motion which could lead to delayed union |
|
|
What is the advantage of an intramedullary position as far as lever arm is concerned? This is especially useful in what type of fracture versus plate and screw contructs?
|
Advantage of intramedullary position is decreased lever arm for bending forces (especially useful in pertrochanteric fractures versus plate and screw construct
|

