![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
35 Cards in this Set
- Front
- Back
|
What is the time frame for perinatal diseases?
|
3 months before birth to 1 month after birth.
|
|
|
What is the leading cause of death in infancy? in childhood?
|
infancy (under 1 yr) - Congenital anomalies
Childhood (1-14 yrs) - accidents |
|
|
What is the difference b/t sequence and syndrome in regards to congenital anomalies?
|
Sequence - pattern (cascade) of anomalies; explained by single, localized pathogenic aberration
Syndrome - constellation of congenital anomalies; cannot be explained on basis of single, localized pathogenic defect |
|
|
Define congenital malformations, congenital disruption and congenital deformation.
|
congenital malformation - Primary errors of morphogenesis
congenital disruption - secondary destruction of previously normal structure (e.g. due to aminiotic bands) Congenital deformation - secondary disturbance of development of normal structure. (esp. uterine constraint, e.g. oligohydramnios) |
|
|
What is oligohydraminos (Potter) sequence?
|
Aminotic leak --> oligohydramnios --> fetal compression --> pulmonary hypoplasia, altered facies, positioning defects of feet/hands, breech presentation
|
|
|
What is the most common etiology of congenital anomalies?
|
Idiopathic (unknown)
|
|
|
What is the main difference b/t embryonic period and fetal period?
Which period is most susceptible to teratogenesis? |
Embryonic period - organogenesis
Fetal period - growth and maturation later weeks of embryonic period (weeks 3-9) are most susceptible to teratogenesis |
|
|
What is the normal gestational age?
|
37 to 42 weeks gestational age
|
|
|
what are 2 etiologies of intracrainal hemorrhage during cranial birth injuries?
|
excessive molding of head
Sudden pressure changes (from forceps, expulsion) |
|
|
What is the common underlying cause of SGA (small-for-gestational-age)?
|
Fetal growth restriction (FGR) or intrauterine growth retardation (IUGR)
|
|
|
List 4 predisposing factors of intracranial hemorrhage in infants.
|
1. prolonged labor
2. hypoxia 3. hemorrhagic disorders 4. intracranial vascular anomalies |
|
|
What is Caput succedaneum?
What is Cephalhematoma? How do you differentiate b/t the 2? |
minior cranial injuries
Caput succedaneum - Scalp edema Cephalhematoma - subperiosteal hemorrhage Cephalhematoma stops at suture line. |
|
|
Which infants are at risks for birth injuries?
|
LGA (large for gestational age)- large (esp. head)
Premature, SGA (small for gestational age)- fragile (esp. bones and intracrainal injury) |
|
|
How is perinatal, transcervical infection trasmitted? (2)
|
amniotic fluid inhalation
infected birth canal |
|
|
What are common organisms in transplacental, perinantal infections? (5)
|
TORCH
Toxoplasma Others (Treponema, viruses) Rubella Cytomegalovirus Herpesvirus |
|
|
Define fetal hydrops.
What is the common cause of fetal hydrops? |
fetal accumulation of edema during intrauterine growth.
Hemolytic disease of the newborn |
|
|
What is the etiology of hemolytic disease of the newborn?
Describe the pathogenesis. Consequences? |
Etiology - maternal-fetal blood group incompatibility (Rh- mother and Rh+ baby)
Pathogenesis: Sensitization (1st exposure) - transplacental bleed or blood transfusion Response (2nd exposure) - IgG across placenta --> type II hypersensitivity --> hemolysis Consequences: Anemia --> heart failure --> increased hydrostatic pressure --> edema Hyperbilirubenemia --> jaundice and kernicterus |
|
|
What is cystic hygroma? cause? consequence?
|
Cystic hygroma - anomalous lymphatic drainage
cause - Turner syndrome Consequence - nonimmune hydrops fetalis |
|
|
List 3 causes of fetal anemia.
|
1. homozygous alpha-thalassemia
2. parvovirus B19 infection 3. twin-twin transfusion syndrome |
|
|
Which 2 enzymes are deficient in PKU?
What are some consequences of hyperphenylalaninemia? |
PAH (Phenylalanine hydroxylase) or DHPR (dihydropteridine reductase)
Impaired brain development Decrease pigmentation (hair and skin) and eczema |
|
|
What is maternal PKU?
|
maternal hyperphenylalanemia but the infant's Phe level is normal.
Phe crosses the placenta and teratogenic to the infant b/c the infant's liver is overloaded with Phe and can't metabolize all. |
|
|
Define type 1, type 2, and type 3 PKU.
Which one can be treated with dietary control alone? |
type 1 - decreased PAH (phe hydroxylase)
type 2 - decreased dihydrobiopterin reductase (DHPR) type 3 - decreased dihydrobiopterin synthase (DHPS) type 1 can be treated with dietary control. |
|
|
Which race is most prone to CF?
|
caucasians
1/2500 live births |
|
|
What chromosome is defective in CF?
|
Chromosome 7q
|
|
|
How is the phenotypic variation of CF determined?
Which organ is most subjective to genotypic variation? |
The phenotype is determined by % loss of CFTR function
Pancreas |
|
|
What bacteria commonly infects the respiratory tract of CF patients?
|
Pseudomonas aeruginosa
|
|
|
How does CF affect sweat glands?
Describe the pathogenesis. |
Produces hypertonic sweat.
CF --> dysfunctional Cl- channels --> impaired Na/Cl reabsorption from lumen --> hypertonic sweat |
|
|
How does CF affect the airway?
Describe the pathogenesis. |
viscous mucous, defective ciliary action, luminal obstrcution
impaired Cl secretion into lumen --> increased influx of Na and water into epithelial cell --> dehydrated mucous. |
|
|
How does CF affect the pancreas?
Describe the pathogenesis. |
mucin pluggin of exocrine ducts --> cystic dilation --> atrophy of acini and fibrosis
atrophy of islets of langerhans --> DM |
|
|
How is the lung affected in CF patients?
|
static mucus
hypoxic microenvironment --> production of bioflim --> protection of organism (Pseudomonas aeruginosa) obstruction and defective capillary action: 1. bacterial infection 2. destruction of muscle and elastic tissue 3. permanent dilation of bronchi and bronchioles (bronchiectasis) |
|
|
Describe how the following organs are affected in CF patients:
1. Intestine 2. Liver 3. Salivary glands 4. Male genital tract |
Intestine: viscid mucus --> obstruction (meconium ileus)
Liver: plugging of bile canaliculi --> eventual biliary cirrhosis Salivary glands: similar to pancreatic changes (parotid gland is not affected b/c it's serous gland) male genital tract: azzospermia/infertility usually congenital bilateral absence of vas deferens (CBAVD) |
|
|
What is the old gold standard diagnostic test for CF? new gold standard test?
|
Old - sweat test (hypertonic sweat); still widely used
New - genetic test; too expensive |
|

This is a section of an infant brain.
What is pointed by the arrows? What is a possible cause of this? What symptom can be observed? |
Kernicterus
Hyperbilirubinemia due to hemolytic anemia. Fetal hydrops can be observed |
|

This is a slide of pancreas.
What does the upper arrow indicate? lower arrow? What disease is this? What other disease can be seen in the late stage of this disease |
Upper arrow - cystic dilation
Lower arrow - fibrosis Cystic fibrosis Diabetes mellitus can result when the islets of Langerhans atrophy. |
|
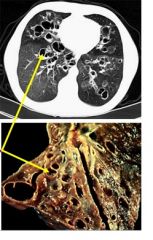
These are pictures of the lung.
What do the arrows indicate? What disease is this? |
Bronchiectasis - permanent dilation of bronchi, bronchioles.
CF |

