![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
365 Cards in this Set
- Front
- Back
|
what is the normal blood concentration of glucose? |
between 3.6-11.0mmol/L
|
|
|
what is the function of glucagon? |
increasing release of glucose from the liver by breakdown of glycogen |
|
|
What are some common symptoms of diabetes? |
Polyuria (increase urination) Polydispia (increased drinking) Weight Loss Weakness Increased infections and impaired healing Blurred vision |
|
|
What is the normal range for FASTING blood glucose? |
3.9 to 6.1 mmol/L |
|
|
What are the two values that help diagnosis diabetes?
|
Random glucose: 11.0 mmol/L + symptoms
Fasting glucose: >6.9mmol/L on 2 occasions |
|
|
what is a downside of tighter gylcemic control?
|
you get fewer complications but you have INCREASED risk of hypoglycemia |
|
|
If a patient is being managed for diabetes, between what are the ideal value of their fasting glucose?
|
4-7mmol/L |
|
|
What are factors that will disturb control of their diabetes?
|
Infection, stress, pregnancy, surgery
|
|
|
How are Type I patients treated? |
Diet/physical activity PLUS |
|
|
Why are type I patients placed on ace inhibitors?
|
ACE inhibitos (Captopril/Ramipril) is used to control nephropathy from increased blood pressure
|
|
|
How are Type II patients treated?
|
1) Diet and Exericse |
|
|
What are the classes of oral hypoglycemics? |
Sulphonylureas (Glyburide) |
|
|
What is a dangerous side effect of sulphonylureas/glyburide |
Can induce hypoglycemia
|
|
|
What is the test used to measure long term diabetic control (3 months)
|
HbA1c which measure glycosylated hemoglobin (how sugar is sticking to blood) |
|
|
What's considered a good HbA1c value? |
<7
|
|
|
What's considered a fair HbA1c value?
|
7-8.9 |
|
|
What's considered a poor HbA1c value?
|
>9.0
|
|
|
What are some macrovascular complications of atherosclerosis? |
Stroke (2-5X increased risk) |
|
|
What are some microvascular complications of atherosclerosis? |
Retinopathy (blindness) (20X increased risk) |
|
|
Complications of diabetes that are not vascular related? |
Neuropathy (numbness, tingling, pain, glove and stocking sensory defects) |
|
|
What emergency is a patient with type I diabetic patient at risk at? |
ketoacidosis, hypoglycemia |
|
|
What is the underlying mechanism behind ketoacidosis?
|
Patient loses excess water, Na, K. Ketones released from the liver cause a metabolic acidosis |
|
|
What can precipitate or cause ketoacidosis? |
infection, insulin error or omission, or could appear in a previously undiagnosed patient |
|
|
How is ketoacidosis treated?
|
insulin, fluid replacement, K replacement
|
|
|
What is the form of ketoacidosis seen in Type II diabetes secondary to dehydration? |
Hyperglycemic hyperosmolar nonketotic state
|
|
|
Some causes of hypoglycemia?
|
overdose of insulin/oral medication or missed meal
|
|
|
What are some drugs that can cause hypoglycemia
|
Sulfonylureas/Glyburide, Glicazide, Chlorpamide |
|
|
What are some symptoms of hypoglycemia?
|
diaphoretic, weak, shaky, palpitations, difficulty thinking, aggressive, vision changes and may lose consciousness
|
|
|
How do we treat hypoglycemia |
Need immediate glucose: juice, candy |
|
|
Based on control/severity/compliance what are some treatment modifications that a dentist may make for a patient with diabetes |
Possibly none. |
|
|
What are some questions that we ask to assess Control Severity Compliance for diabetes |
When were you first Dxed? |
|
|
When is a patient considered brittle?
|
Poor compliance and poor control
Good compliance and poor control (most brittle) |
|
|
When should we be more aggressive with antibiotics in terms of patients with diabetes? |
Patients with high blood sugar
|
|
|
Dental manifestations of diabetes? |
xerostomia |
|
|
What are the normal functions of the liver? |
1. Secretion of bile for fat absorption 2. Glycogen storage (w/insulin in Hb) 3. Break down glycogen (w/glucagon in Hb) 4. RBC breakdown and excretion of bilirubin 5. Synthesis of coagulation factors 6. Synthesis of albumin 7. Drug metabolism |
|
|
What are the two most common causes of hepatitis? |
1. alcoholic 2. viral (A,B,C,D,E) |
|
|
Less common causes of Hepatitis? |
syphilis, TB methotrexate, ketoconazole, Acetaminohpen overdose |
|
|
Symptoms of hepatitis? |
1. Jaundice 2. Abdominal Pain 3. Nausea, vomiting, fever malaise 4. hepatomegaly and Splenomegaly (portal hypertension causes backing up of blood in these areas and turns them big and blue) 5. can be asymptomatic (Non-specific signs are fatigue, weight loss, itchniness, right upper quadrant pain) |
|
|
What is the main transmission method of Hep A and E? |
Fecal-oral (contaminated hands and no handwashing) |
|
|
Sources of Hep A? |
Water and shellfish |
|
|
What is the carrier state of Hep A? |
None. Patients make a full recovery |
|
|
How is Hep B transmitted? |
Percutaneous/permucosal injuries (sex, needlestick injuries)
|
|
|
What are the sources of Hep B? |
Blood and blood products
|
|
|
What is the risk of Hep B contraction? |
6-30% with needlestick |
|
|
What is the risk of being a carrier with hepatitis B? |
5-10% with increased risk of hepatocellular carcinoma and cirrhosis |
|
|
What is the source of transmission for hepatitis C ? |
Percutaenous. Sex (lower risk than B but high risk with anal sex) |
|
|
What is the source of Hepatitis C? |
Blood and blood products |
|
|
What are the high risk groups of patients contracting hep C? |
IV drug users transfusion receipients prior to 1992 Dentists |
|
|
What is the risk of contracting hep C via needlestick injury? |
2-8% |
|
|
What is the incubation period for Hep C? |
14-180 days |
|
|
What is the risk of becoming a carrier for Hep C? |
80-90% risk! and increased risk of hepatocellular carcinoma and cirrhosis |
|
|
What type of viral hepatitis doesn't have a vaccination? |
Hepatitis C! |
|
|
What are some possible questions you can ask to identify a viral hepatitis patient? |
Did other kids at school get it? Did you get it from a needlestick injury? Do you use IV drugs? |
|
|
What is the guideline if you are exposed to Hep B blood through needlestick injury? |
Determine the titre of anti-HBs in the dentist. If adequate: No tx needed If inadequate: dentist needs Hep B immunoglobulin |
|
|
What is the guideline if you are exposed to Hep C blood through needlestick injury? |
Exposed professional gets baseline and fllow up testing for anti-HCV and liver enzymes -Pray |
|
|
How many oz of alcohol per week before someone is considered to have a alcohol problem? |
Males: >12oz/week Females: >9oz/week Someone is considered a alcoholic when they drink more than 2 drinks a day. Big problem if they drink 24 pack a week |
|
|
When taking history to determine alcoholism, how many times should you multiply the answer? |
Always double the reported amount |
|
|
What are the stages of liver failure in a alcoholic? |
Stage 1: Fatty liver Stage 2: Alcoholic hepatitis Final stage: cirrohiss with parenchymal damage and scarring leading to portal hypertension |
|
|
What are some problems with end stage liver disease? |
1: Loss of synthetic functions (No more Vit K coagualation factors: II, VII, IX, X), No more Albumin 2: Portal vein hypertension 3: loss of detoxification function 4: Bone marrow toxicity: anemia, leukopenia and thrombocytopenia (decrease of all blood cell types) 5: endocrine disturbances: testicular atrophy and gynecomastia
|
|
|
What is the consequences of hypoalbuminemia observed in end stage liver disease? |
Edema because fluid moves into the tissues without albumin |
|
|
What causes the jaundice seen in end stage liver disease? |
Elevated bilirubin |
|
|
What test is a general sign that the patient has hepatitis |
AST/ALT (elevated levels) |
|
|
Is INR increased or decreased with end stage liver disease? |
Increased (Lack of clotting factors). So expect increased bleding! |
|
|
How does end stage liver disease affect drug metabolism? |
metabolism can be both increased AND decreased! Increased metabolism: early (liver compensates by trying to increase first pass metabolism). So drug has LESS effect Decreased metabolism: late liver failure. Loss of hepatic functions. Drugs have increased effect. ANother reason is loss of albumin binding to drugs. More active drugs are available. |
|
|
How is liver disease treated? |
Acute hepatitis: steroids, supportive Chronic hepatitis: interferon End stage: Liver transplant |
|
|
Dental considerations for patients with liver disease? |
Beware of alcoholics with secondary addictions
Caution or avoid hepatically metabolized drugs: ie. NSAIDs, NARCOTICS, ACETAMINOPHEN, benzodiazepines, metronidazole, LOCAL ANAESTHETICS
Bleeding tendencies: May require vitamin K, Fresh frozen plasma or platelets |
|
|
What are the two parts of the adrenal gland? |
1) Cortex 2) Medulla
|
|
|
What does the Adrenal Medulla secrete? |
Part of the sympathetic system, secretes Epi and Norepinephrine |
|
|
What does the Adrenal cortex secrete? |
sex steroids, mineralcorticoids and glucocorticoids |
|
|
What is the function of the mineralcorticoids? |
Control of Na/K/H2O (controls BP) in conjunction with angiotensin/renin system by releasing aldosterone CRUCIAL TO LIFE |
|
|
How does aldosterone help regulate BP? |
Acts on the collecting tubules in the nephrons to collect NA (and therefore H2O) |
|
|
What is the function of glucocorticoids? |
1) Control of carb/protein and fat metabolism 2) Maintains of vascular reactivity by "priming" blood vessels to respond to catecholamine driven vasoconstriction 3) Anti-inflammatory 4) maintenance of homeostasis in response to stress 5) Insulin antagonist (Increases serum glucose and increases hepatic glucose output, initiates lipolysis, proteolysis, gluconeogenesis) 6) inhibits endothelial cell adhesion |
|
|
How long does it take for steroids to come into effect? |
2-4 hours |
|
|
How much glucocorticoids are being released by the body a day? |
20mg (highest released in the morning) |
|
|
How much glucocorticoids is released under stress? |
200mg |
|
|
Under what condition is there inhibited glucorticoids release? |
If the patient is on exogenous steroids |
|
|
What are the three most common adrenal diseases? |
hyperadrenalism hypoadrenalism Patients taken oral steroids |
|
|
What are the two types of hyperadrenalism (cushingoid)? How are they different? |
Cushing's disease: due to excess cortisol production. (Pituitary or adrenal tumour)
Cushing's Syndrome: signs and symptoms of excess steroid secondary to chronic use |
|
|
What are some side effects of excess long term systemic steroids? |
Weight gain, moon face, adrenocortical suppresion, buffalo hump, abdominal straie, acne, hypertension, heart failure, osteoporosis, growth suppresion, diabetes, impaired healing, peptic ulcers, depression, psychosis |
|
|
What are the types of hypoadrenalism? |
Primary insufficiency: Addison's disease where 90% of adrenal cortex is lost due to autoimmune, hemorrhage, infection, tumor or sugery (Both aldosterone AND cortisol deficient)
Secondary: hypothalamic or pituitary disease /exogenous steroids causing suppression of the hypothalamic/pituitary axis leading to atrophy of the adrenal cortex. CORTISOL DEFICIENCY ONLY |
|
|
List some conditions which are managed by steroids |
Rheumatoid arthritis Systemic lupus erythematosis Asthma Inflammatory bowel disease Prevention of organ transplant rejection |
|
|
how much prednisone is equivalent to 20mg of Cortisol? |
5mg Prednisone |
|
|
how much solumedrol is equivalent to 20mg of Cortisol? |
4mg |
|
|
how much decadron is equivalent to 20mg of Cortisol? |
.75mg |
|
|
How much exogenous steroid does a patient need to take before we consider them to be Adrenal suppressed? |
>5mg of Prednisone/day or 20mg Cortisol greater than 2 weeks within the last year. |
|
|
How much exogenous steroid does a patient need to take before we consider them to be immuno suppressed? |
6 months of continual steroid use |
|
|
What are some problems associated with adrenal insufficiency? |
1) Impaired Carb protein and fat metabolism 2) 4H's: Hypoglycemia, Hypovolemia (low fluid), Hyperkalemia (High K+), Hypotension (No priming vessels to E and NE) |
|
|
Signs and Symptoms and Hypoadrenalism? |
Excess Pigmentation (recall addison's disease) Postural hypotension Muscular weakness Nausea, Anorexia, weight loss
|
|
|
What are some possible lab values to diagnose adrenal disorders? |
Tough to do. Some tests are: -Cortical tropic releasing hormone (CRH) stimulation test ACTH stimulation 24 hour urine cortisol |
|
|
What iis the treatment for Adrenal insufficiency? |
1)Treat the cause (tumor/infection) 2) Hormone replacement mineralocorticoid and glucocorticoids
|
|
|
What is the most common regimen prescribed for mineralocorticoid insufficiency? |
Fludrocortisone (Florinef): 0.05-0.1mg daily |
|
|
What is the most common regimen prescirbed for glucocorticoid insufficiency? |
Cortisol: 20mgAM/10mgPM Prednisone: 5mgAM/2.5mg PM (reflects normal diurnal cycle) |
|
|
What is the Medical Emergency that can precipitate for patients with hypoadrenalism? |
Acute Adrenal insufficiency! |
|
|
What are some symptoms of Acute Adrenal Insufficiency? What is it a result of? |
Can be triggered because patient is unable to handle physiological stress 1) Acute refractory hypotension 2) diaphoresis (excessive sweating) 3) dehydration 4) dyspnea, hypothermia 5) hypoglycemia, circulatory collapse, death |
|
|
How is Acute adrenal insufficiency treated? |
-Hydrocortisone 100mg IV bolus -HOSPITAL setting for fluid and electrolyte replacement -correction of hypoglycemia continued IV steroid |
|
|
How can Adrenal Crisis be prevented? |
1) Recognize at risk patients! -Addison's disease -Patient who have/are on suppressive steroids - taking low suppressive dose (Prednisone 10mg or less)
2) Supplement adrenal suppressed patients: give 100mg cortisol (or equivalent) day before/ day of/ day after procedure OR double the existing dose if taking 10mg of prednisone or less |
|
|
What are some modifications that can be made for patients with adrenal disease in a dental appointment? |
1) Assess compliance with steroids 2) Assess need for supplementation 3) Discontinue Ketaconazole and barbituates if possible. they inhibit steroid production 4) AM procedures! (Highest cortisol) 5) Anxiety reduction (Nitrous) 6) Good pain control but avoid NSAIDS (peptic ulcers) 7) Monitor BP 8) Cushingoid patients are prone to fractures (osteoporosis) 9) CUsing leads to diabetes |
|
|
patient is currently taking 7mg Prednisone/day for the last month. Are they Adrenal suppressed, depressed or both? |
Suppressed ONLY! (Not depressed because they are still being supplied with cortisol!) |
|
|
patient has taken 5mg Prednisone/day for 3 weeks couple months ago. They are no longer on the steroids. Are they adrenal suppressed, depressed or both? |
BOTH. Adrenal suppressed and their body also isn't getting any steroids |
|
|
What is suppressed if you take a short course (1 day) of steroids? |
Inflammatory suppression only |
|
|
What is suppressed if you take a long course (2 weeks) of steroids? |
inflammatory AND adrenosuppression |
|
|
What are some important functions of the kidney? |
1) Creates Urine and Controls BP 2) Manages electrolyte balance (Ca2+ and Na+) which affects blood volume 3) Creates erythropoietin which stimulates RBC creation 4) Eliminate drugs and metabolic waste 5) Eliminates Urea, Creatinine 6) Regulate Blood pH 7) Reabsorption of glucose and other important nutrients 8) Activation of Vitamin D 9) Control of PO4 |
|
|
List the steps in the Renal Angiotensin system |
1) Drop in BP 2) Renin is released from the Juxtaglomerular apparatus. 3) Renin catalyzes the production of Angiotensin I from protein circulating in blood 4) ACE (Angiotensin converting enzyme) converts Angiotensin I --> Angiotensin II 5) Angiotensin II is a potent vasoconstrictor. Also stimualtes release of Aldosterone for Na resorption. 6) Increased BP |
|
|
At what point is someone defined to have End stage renal disease? |
Loss of 50 to 75% of nephrons |
|
|
What are some typical causes of renal failure? |
Diabetes (34%) Hypertension (25%) Chronic glomerulonephritis (16%) other: polycystic kidney disease, SLE, neoplasms, AIDs, etc. |
|
|
Name the 9 tests that are used to assess renal failure |
1) Urinalaysis: presence of protein or blood. 2) Increased Creatinine 3) Increase Blood Urea Nitrogen 4) Increased K+/Decreased Na 5) Anemia/thrombocytopenia 6) Increased PTT/INR 7) Decreased Creatinine clearance 8)GFR decrease (measured indirectly) 9) Blood pH decreased (more H+ in blood, must be combined with another test to indicate renal failure) |
|
|
What is the normal GFR rate? |
100-150mL/min |
|
|
What does the Glomerular filtration rate have to be in order to be classified as Renal insufficient? |
50-90ml/min |
|
|
What does the Glomerular filtration rate have to be in order to be classified as moderate renal failure? |
10-50mL/min |
|
|
What does the Glomerular filtration rate have to be in order to be classified as severe renal failure? |
<10mL/min |
|
|
Stages of Renal failure? |
1) Diminished Renal Reserve: mild increase in blood creatinine and 10-20% decrease in GFR 2) Renal Insufficiency: Increase in BUN and 20-50% decline in GFR 3) Renal Failure: Uremia and >50% decline in GFR with loss of excretory, endocrine and metabolic function |
|
|
How many nephrons need to be lost before Kidneys are no longer able to compensate? |
50%-75% |
|
|
What is polyuria? |
Abornmally large passage of urine, seen after 50-75% of nephrons are lost |
|
|
What usually follows polyuria in renal failure? |
uremia (high NH3 in blood) |
|
|
What are some characteristics of Uremia? |
Fluid overload leading to hypertension Congestive Heart Failure Pulmonary Edema Urea build up Metabolic Acidosis Hyponatremia (low Na)/Hyperkalemia (Too much K+) Anemia WBC dysfunction (decreased immunity) Platelet and Factor coagulopathy Renal Osteodystrophy: decreased Vitamin D and 2ndary hyperparathyroidism |
|
|
How is Renal Failure managed? |
1. Conservative care: fluid, K, Na, Protein and phosphate 2. Recombinant human erythropoietin 3. Treat underlying disease (diabetes, hypertension, CHF, infection etc.) 4. Avoid nephrotoxic drugs 5. Dialysis (severe cases) |
|
|
What are the two types of dialysis? |
Peritoneal dialysis (10%) and hemodialysis (most severe and 90% of all dialysis) |
|
|
How does Peritoneal dialysis work? |
Uses mesenteric capillary bed to act like a giant bowman's capsule. Pulls fluid and excess ammonia into Peritoneal fluid. Uses hyertonic solution, indwelling catheter and frequent exchanges |
|
|
How does Hemodialysis work? |
A surgical fistula is created (vein to vein or vein to artery) on one of their arms. They need to take heparin. Patients go in for dialysis 2 to 3 days, 3-4 hours per session. |
|
|
What is the survival rate of someone on Hemodialysis? |
1 year survival is 78% 5 year survival is 28% |
|
|
What is a potential complication of having a surgical fistula? |
May cause a shear force on veins that may cause endothelitis |
|
|
How does heparin work? |
supercharges anti-thrombin 3 which is a normal anti-coagulant |
|
|
What are two medications that kidney transplant patients usually have to take? |
cyclosporin and calcium channel blockers (and steroids) |
|
|
What is a side effect of taking cyclosporin? |
Gingival hyperplasia. It is also nephrotoxic |
|
|
What are some precautions that need to made for a patient with renal failure? |
1) Monitor BP: avoid fistula arm 2) Assess for anemia (Low EPO) 3) Increased risk of bleeding (heparin). So plan around dialysis. DON'T DO PROCEDURES ON SAME DAY AS DIALYSIS 4) Increased risk of infection! 5) Avoid High dose NSAIDS or Acetaminophen. Prescribe opiates or small doses 6) Remember they have clearance issues 7) Reduce dose of nephrotoxic drugs 8) consider oral complications 9) Consider prophylatic antibiotics for fistula |
|
|
What are some oral complications associated with Renal failure? |
Xerostomia, candidiasis, gingival bleeding/petechaie, osteodystrophy (Lack of Vitamin D and hypothyroid calcium deficiency causes of release of parathyroid hormone.) BRITTLE JAWS! CAREFUL WITH EXTRACTIONS! |
|
|
What are some nephrotoxic drugs? |
tetracycline, metronidazole, acyclovir, penicillins and cephalosporins
|
|
|
What is a antibiotic that is generally not nephrotoxic? |
Clindamycin |
|
|
What is something a dentist can do to trigger an asthma attack? |
NSAIDs Induce stress Use injectables with sulfite |
|
|
How is asthma diagnosed? |
Observed clinically Pulmonary function studies (+/- methacholine challenge) |
|
|
What is typical treatment (from first line to last resort?) |
1) Short acting beta agonist prn 2) steroid puffer 3) Long acting beta agonist 4) Leukotriene receptor agonist 5) Oral steroids 6) Methylxanthines (if desparate) |
|
|
What class of drugs is Ventolin (Salbutamol) and Bricanyl (terbutaline)? |
Short acting beta agonist |
|
|
What is the worst side effect of Short acting beta agonists? |
Tremors (which is not really all that serious) |
|
|
What class of drugs are Flovent (fluticasone), Pulmicort (budesonide) Qvar (beclomethasone) |
Steroid puffers |
|
|
What is a oral complication with using steroid puffers? |
Fungal infection |
|
|
If a patient is using a steroid puffer, what is that indicative of? |
severe asthma |
|
|
What class of drugs does Serevent (salmeterol) and Oxeze (formoterol) belong to? |
Long acting beta agonist |
|
|
How long does Short acting beta agonists usually last for? |
4 hours |
|
|
What class of drugs does Singulair (montelukast) Accolate (Zafinlukast) belong to? When are they usually prescribed? |
Leukotriene receptor antagonists. Usually for mild asthmatics only (most cases are severe or moderate) |
|
|
What class of drugs are theodur (theophylline) and Uniphyl (theophylline) part of? If a patient is on this what is it usually indicative of? |
Methylxanthines Patient has either: 1) Really old school doctor who hasn't kept up to date with asthma medications OR 2) Nothing else works for the patient (be careful with these patients!). 3) Pill works for 12 hours but there are some side effects |
|
|
What usually triggers acute exacerbation of asthma? |
Viral attack |
|
|
What is the treatment of acute exacerbation of viral induced asthma? |
IV fluids Beta agonist IV steroids (12-24 hours to kick in) Oxygen |
|
|
What is a good question you should ask a patient with asthma to determine their level of severity? |
1) How often do you need your Ventoline/Bricanly? 2) What is the frequency of your asthma attacks? 3) How many puffers do you have? 4) Do you know what triggers your asthma attack? |
|
|
COPD can be divided into two groups: Chronic bronchitis and Emphysema. |
Chronic bronchitits: produce sputum. Usually heavyset
Emphysema: Alveoli have become one large sac (less efficient gas exchange). These patients are skinny because they have to expend a lot of energy to breath. |
|
|
Signs and symptoms of Emphysema? |
Sputum (Pure asthmatics don't produce sputum!) SOB Wheezing
|
|
|
What's a good way to figure out a patient has undiagnosed COPD? |
Ask their significant other! Patients often under report their symptoms. Ask the significant other if the patient coughs a lot |
|
|
How is COPD normally diagnosed? |
With pulmonary function studies (FEV1 test). mild: >80% FEV1 Moderate: <80% Severe: <50% Very severe: <30% or <50% with chronic respiratory failure. |
|
|
Patient is taking the following medications: Atrovent (ipratropium) OR Spiriva (tiotropium)
|
COPD (prevents mucous production) |
|
|
What is the first line treatment usually for patients with COPD? |
Anti-cholinergics with short acting beta agonists
(Puffers/drugs for COPD are very similar to Asthmatic drugs but COPD have anti-cholinergic puffers on top of everything else asthma patient may have to use) |
|
|
Severe COPD patients may use oxygen but what is the problem with that? |
Shortens life span due to pulmonary artery constriction. The right side lungs fail, followed by the right side. Too much oxygen can be dangerous |
|
|
How are acute exacerbations of COPD treated?
|
Usually due to bacterial triggers. Therefore the treatment regimen is as follows: 1. antibiotics 2. Steroids (oral) 3. Bronchodilators 4. Oxygen |
|
|
What should a dentist be aware of for a patient with COPD? |
1. Encourage patient to quit smoking 2. Monitor their oxygen levels/breathing rate. May require more oxygen? 3. What for respiratory depression with medicaitons like Benzodiazepines and narcotics!! |
|
|
Why shouldn't a COPD patient be prescribed benzodiazepines and narcotics? |
Can cause respiratory depression
|
|
|
What is CO2 narcosis and how can a dentist cause it? |
COPD patients have high CO2 retention, so the medulla stops monitoring CO2 levels because the levels are constantly high. As an alternative, the medulla relies on oxygen levels to determine breathing rate. If a COPD patient gets too much oxygen, the medulla will detect it and stop breathing. With no breathing and an already high CO2 level you get CO2 narcosis. (IMPORTANT CONCEPT TO MEMORIZE. HAS BEEN TESTED BY LA POINTE. He asked whether or not you should give oxygen to a COPD patient who has a cold. |
|
|
What are the three hormones that the thyroid glance produces? |
T3 (triiodothyronine) T4 (Thyroxine) Calcitonin |
|
|
Which is the most potent form of thyroid hormone? |
T3. |
|
|
Explain how T3 (thyroid hormone) is produced in the body |
20% is created directly from the thyroid itself 80% is converted from T4s. T4s are created in the thyroid and then undergoes deiodination in the periphery to become T3s |
|
|
What is the function of thyroid hormones? |
1) Controls oxidative metabolism and basal metabolic rate 2) Growth and maturation of tissues -Amount produced/released depends on the surrounding environment |
|
|
When is thyroid hormone release upregulated? |
in response to physiological stress (cold, illness etc) |
|
|
When is thyroid hormone release downregulated? |
negative feedback in response to increased thyroid hormones |
|
|
Explain the thyroid hormone release mechanism in response to stress/cold/decreasing thyroid hormone |
1. Thyroid releases Thyroid releasing hormone (TRH) which goes to the anterior pituitary 2. Anterior pituitary releases Thyroid Stimulating hormone (TSH) which acts on the Thyroid gland 3. Thyroid releases T4 (Thyroxine) |
|
|
What hormone is used to assess the thyroid? |
Serum Thyroid stimulating hormone!
|
|
|
What does a high concentration of TSH signify? |
HYPOthyroidism (Anterior pituitary constantly trying to stimulate thyroid) |
|
|
What does a low concentration of TSH signify? |
HYPERthyroidism (No need for more thyroid stimulation) |
|
|
What are some reasons for HYPERthyroidism? |
1) Autoimmune (Grave's disease) 2) Multinodular goiter 3) Thyroid adenoma 4) Subacute thyroiditis 5) Ingestion of Thyroid hormone (OD/Factitial/Food) 5) Anteroid pituitary disease |
|
|
What is the underlying mechanism behind Grave's disease? |
Hyperthyroidism caused by antibodies produced to target the TSH receptor on the thyroid. You get Constant release of T3s and T4 |
|
|
How much more prevalent is grave's disease in women compared to men? |
7:1 female: male |
|
|
What are the signs and symptoms of Grave's disease? |

1) Nervousness, irritability, tremor fatigue, heat intolerance, weight loss, rosy complexion tachycardia, palpitations, atrial fribrilation, myxedema (red, raised puffy areas), dyspnea due to muscle weakness, diarrhea, wide stare, lid lag. Grave's opthalmopathy (edema and inflammation of the extra-ocular muscles).
|
|
|
T/F Grave's opthmalmopathy can persist even if hyperthyroid is cured |
True. May cause blindness! |
|
|
What are the two drugs used to treat hyperthyroidism? |
1) propylthiouracil: blocks hormone synthesis in the thyroid and conversion of T4 --> T3 in the periphery 2) Beta-Blocker helps control the adrenergic symptoms (Tachycardia and Afib) |
|
|
What are two invasive methods to treat Grave's disease? |
1) Radioiodine ablation 2) Thyroidectomy Both cases: patients become hypothyroid (which is then simply treated with synthroid) |
|
|
What acute crisis is a patient with hyperthyroidism at risk of developing? |
thyroid storm/thyrotoxic crisis |
|
|
Who are at risk of developing thyroid storm? |
-->More likely in patients who have long standing or poorly treated disease in patients with goiter and eye signs --> Precipitated by trauma, infection or surgery (kicks the hyperthyroid over the edge) -->Epinephrine (controversial) |
|
|
Signs and Symptoms of Thyroid storm? |
Extremel restlessness Nausea, vomiting, abdominal pain fever, diaphoresis tachycardia, arrhythmia pulomary edema, congestive heart failure Stupor, coma, hypotension..death |
|
|
How is thyroid storm treated? |
1) Propylthiouracil 2) Potassium iodide (Thyro-Block) 3) Propranolol 4) Glucocorticoids 5) IV glucose, Vitamin B complex 6) Wet packs, ice packs, fans |
|
|
How should a dentist modify his appointment for a poorly controlled hyperthyroid patient? |
1) Be aware of signs and symptoms 2) assess compliance with medications 3) Avoid epi 4) refer to MD if concerns exist 5) prevent and manage infection 6) be alert S&S of thyroid storm 7) Treat as normal if well controlled |
|
|
What are some causes of hypothyroidism? |
1) Congenital agenesis or hypoplastic 2) autoimmune (Hashimoto's thyroiditis) 3) iodine deficiency with goitre (No iodine=no thyroid hormone release) 4) iodine excess (can kill thyroid) 5) post-radio ablation 6) post-surgical ablation 7) anterior pituitary disease |
|
|
What are some signs and symptoms of hypothyroidism? |
1) Congenital Neonatal cretinism 2) Slowing of mental and physical activity, weakness 3) Cold intolerance 4) Constipation, weight gain 5) Loss of outer 1/3 of the eyebrows 6) puffy eyelids 7) Hoarse voice 8) Myxedema |
|
|
What is the treatment of hypothyroidism? |
1) T4 (L-thyroxin, Synthroid) 2) Titrated until patient has normal TSH |
|
|
What is the crisis form of hypothyroid? |
Myxedematous Coma |
|
|
What are some risk factors that may trigger a hypothyroid patient into myxedematous coma? |
1) Seen in untreated or non-compliant patients 2) Precipated by cold, trauma, surgery, infections and CNS depressants 3) More common in winter (need it in winter but body can't supply) |
|
|
What are signs and symptoms of myxedematous coma? |
severe myxedema, bradycardia, severe hypotension |
|
|
What are some treatment options for myxedematous coma? |
IV T4, Steroids, CPR |
|
|
What are some modifications that a dentist should make for a patient with myxedematous coma? |
1) be aware of signs and symptoms 2) assess compliance with medications 3) in poorly controlled or newly diagnosed: use CNS depressants with caution! 4) refer to MD if concerns exist 5) prevent and manage infection 6) be alert to S&S of myxedematous coma 7) treat as normal if well controlled with caution |
|
|
What are some benign thyroid masses? |
Goitre due to iodine deficiency enlargmement due to graves disease Thyroiditis thyroglossal duct cyst benign adenoma |
|
|
What are some malignant thyroid masses |
follicular carcinoma papillary carcinoma anaplastic carcinoma other carcinoma |
|
|
In what demographic does finding a thyroid nodule have a increased risk for cancer |
in a patients of young age in a male with a history of radiation exposure with concomitant dysnea, dysphagia or dysphonia (hoarseness, due to compression of recurrent laryngeal nerve) be a hard fixed lump be a single nodule have a demonstrated growth |
|
|
What are some assessment methods for checking thyroid function |
1) History 2) Clinical examination 3) thyroid function tests 4) Thyroid scan 5) fine needle aspiration biopsy (Best way to find out) |
|
|
What are some manifestations of atherosclerosis? |
1) Coronary Artery disease (Angina/MI) 2) Cerebral Vascular disease (Stroke) 3) Peripheral vascular disease |
|
|
What are some risk factors for atherosclerosis? |
1) Hypertension 2) Diabetes 3) Hyperlipidemia 4)Smoking 5) Family History (Only significant if family member had it at <55 years) |
|
|
Explain how bp is measured step by step |
Measure hypertension 2cm above the median cubital. Other important factors include: proper timing, position (below the heart and tight), proper cuff size. Feel the radial artery and increase pressure until you can’t feel the radial artery. Inflate 20 points above that. Then deflate. The first time you hear “boop boop” is your systolic. Then deflate. When the “boop boop” disappears it’s diastolic |
|
|
What are some things that can artificially raise blood pressure? |
coffee and smoking before appointment White coat syndrome
|
|
|
At what BP is a person considered to be hypertensive? |
140/90 |
|
|
What are some signs and symptoms of hypertension? |
Asymptomatic or end organ damage |
|
|
What are some organs that can fail due to hypertension |
kidney, brain, heart,eyes |
|
|
What are some non-pharmalogical treatments for hypertension? |
limit salt intake weight loss regular exercise limit alcohol (2 cups a day or less) smoking cessation |
|
|
What are the typical pharmalogical tx for hypertension? |
1) Diuretics 2) ACE inhibitors/ARB 3) CCB 4) Beta blockers 5) Miscellaneous |
|
|
What class of drugs is Hydrochlorthiazide, Chlorthalidone and Indapamide part of? |
Diuretics |
|
|
What class of drugs contain the end in "pril" |
ACE inhibitors |
|
|
What class of drugs end with "Sartan" or "Sarten"? |
ARBs |
|
|
What class of drugs end with "olol"? |
Beta blockers |
|
|
What class of drugs are verapamil, dilitiazem Nifedipine, Felodipine, Amlodipine? |
Calcium Channel Blockers |
|
|
What are some modifications that a dentist should make for patients with hypertension/atherosclerosis |
AVOID SURGERY IF DIASTOLIC >100 1) Take anti-hypertensive therapy day of surgery. 2) ask "How often do you take your BP and what is your usual number?" 3) Be aware of any complications that the patient might have from hypertension 4) Emotional stress/and or pain will increase BP 5) Minimize use of vasopressors! 6) be aware of postural hypotension (Don't let them get up too fast)
|
|
|
What do you do if a patient reports "being lightheaded" when they get up from your chair |
Ask the patient to lie down so they can recover. |
|
|
What is the main difference between a MI and angina? |
TIME. MI is >20 minutes |
|
|
What is the etiology behind angina? |
A compromise in coronary blood flow |
|
|
What are some common medications that a patient with angina might take? |
Beta blockers CCB Nitrates Antiplatelet drug (ie. Plavix) Statin |
|
|
What is a common side effect of Nitrate patches? |
Whomping headaches |
|
|
What is a medication that you may give to a patient who is currently having a heart attack |
2 aspirins (It's ok even if the patient is already on Warfarin) |
|
|
What class of drugs does Nitrodur and Minitran belong to? |
Nitrate patches |
|
|
What class of drugs are clopidegrel, tricagrelor and Prasugrel part of? |
Antiplatelet agents |
|
|
What are the two types of stents used in angioplasty? |
Bare Metal and Drug eluding |
|
|
What is the main difference between bare metal and drug eluding stent. |
The length of time that the patient must be on antiplatelet drugs. Bare metal: 3 months Drug eluding: 1 year
|
|
|
Why is a unstable Angina significant? |
it's a medical emergency! (50% change of MI) |
|
|
How is unstable angina defined? |
when a patient reports erratic angina (change in duration, intensity) |
|
|
What should you do if a patient reports unstable angina? |
Give 2 aspirins and send to the emergency room |
|
|
what is the etiology of myocardial infarction? |
acute occlusion of a coronary artery. |
|
|
If a patient previously had a heart attack what medication may they be on? |
Same drugs used to treat angina and +/- ACE inhibitor |
|
|
If a patient gets angina after walking more than 2 blocks or 1 flight of stairs, where do they fall on the CCS scale? |
CCS II |
|
|
If a patient gets angina after walking less than 2 blocks or 1 flight of stairs, where do they fall on the CCS scale? |
CCS III |
|
|
If a patient gets angina at rest, where do they fall on the CCS scale? |
CCS IV |
|
|
Which patients on the CCS scale of angina severity should NOT be operated on? |
Class III and IV |
|
|
Should a patient discontinue their heart medication before a dental procedure? |
No. Especially Beta blockers! Make sure they take all their medications as normal. |
|
|
What factors can exacerbate angina in patients with ischemic heart disease? |
pain(be careful with injection), vasopressors, emotional stress, |
|
|
What is the definition of congestive heart failure? |
heart can not pump sufficient blood to meet the metabolic demands of the tissues. |
|
|
What are some possible etiologies behind congestive heart failure |
Ischemic heart disease hypertension Valvular heart disease , cardiomyopathies, toxins |
|
|
What are some signs and symptoms of left side congestive heart failure? |
Shortness of breath because fluid builds up upstream (lungs) of the pump. More severe than right failure |
|
|
What are some signs and symptoms of right side congestive heart failure? |
Blood pooling in the body |
|
|
What are two drugs that are strong indicators that a patient may be suffering from congestive heart failure? |
Spironolactone and digoxin |
|
|
What are some considerations a dentist should make for a patient with congestive heart failure? |
1)Assess severity of heart failure 2)continue medications preoperatively 3)Avoid exacerbating factors, especially vasopressors and excessive fluids 4) Avoid supine position as it may precipitate orthopnea |
|
|
What is a heart murmur? |
is an abnormal heart sound generated by a dysnfunctional valve |
|
|
What are the two types of valve dysfunctions? |
Stenosis: Valve only opens halfway Insufficiency: Leakage |
|
|
What are the 3 causes of valvular heart disease? Which one is the most common? |
Congenital, rheumatic, degenerative --> Degenerative is most common now |
|
|
What are some signs and symptoms of valvular heart disease? |
1) Asymptomatic 2) Heart failure 3) angina 4) endocarditis --> Most people don't have symptoms until the heart fails. |
|
|
What is the typical treatment of valvular heart disease? |
Medical management of angina and/or heart failure Repair/replacement of valve (tissue vs. mechanical) |
|
|
What are some things a dentist should be aware of when treating a patient with valvular HD? |
Stress of surgery could exacerbate angina and/or heart failure. May require antibiotic prophylaxis to prevent endocarditis May require anticoagulation (consult with patient cardiologist/physician) |
|
|
for a patient with a previous history of endocarditis, which dental procedures require endocarditis prophylaxis? |
Dental procedures that disrupt the mucosa |
|
|
Which patients require antibiotic prophylaxis? |
1) Patients with prosthetic valves 2) Prior endocarditis 3) unrepaired cyanotic congenital heart disease 4) valvulopathy in heart transplant 5) Patients with joint replacement |
|
|
What is the typical antibiotic and dosage given for antibiotic prophylaxis? |
Amoxicillin: 2 grams orally 30-60 minutes preoperatively w |
|
|
if you need to give antibiotic prophylaxis but the patient is allergic to penicillin? |
Clindamycin: 600 mg orally 30-60 minutes preoperatively |
|
|
define arrhythmia |
is a problem with rate or rhythm of the heartbeat due to disturbance in any part of the conduction pathway (definition from the National Institutes of Health) |
|
|
What are some signs and symptoms of tachy-arrythmia? |
palpitations (biggest problem), lightheadedness, chest pain and/or SOB (shortness of breath) |
|
|
What are some signs and symptoms of brady-arrythmia? |
weakness, lightheadedness, SOB and/or syncope. |
|
|
Patient is on amiodarone. What condition do they most likely have? |
arrhythmia |
|
|
Patients with a ICD (implantable cardioverter defibrillator) have what condition? |
Tach-arrhythmia |
|
|
What medications might a patient with tachy-arrhythmia take? |
Beta-blocker Calcium channel blocker Digoxin Amiodarone anticogulation |
|
|
What are things that a dentist should be aware of for a patient with arrythmia ? |
1) Minimize use of sympathomimetics (ie. Adrenaline in local anaesthetic). Stimulates heart and stimulate arrhythmia 4) Maintain cardiac medications peri-procedure |
|
|
What are some causes for syncope? |
Postural hypotension Vasovagal (very common in the dental office) Arrhythmia (especially brady) |
|
|
What are some things that a dentist can do to avoid causing syncope? |
Avoid sudden upright positioning to minimize postural hypotension. (Especially with elderly patients. Their baroreceptor reflex is delayed so if you move them up too quickly there is a quick drop in blood pressure that can cause fainting). |
|
|
List some common GI diseases/disorders |
Gastro Esophageal Reflux Disease (GERD) Peptic Ulcer Disease (PUD) Inflammatory Bowel Disease (BID) Pseudomembranous colitis Irritable Bowel Syndrome (IBS) |
|
|
What is GERD? |
reflux of acidic gastric contents into the esophagus |
|
|
What are some complications associated with GERD? |
1)Ulceration: Constant reflux causes esophageal bleeding, inflammation, healing and scarring. 2) Stricture (tightening of esophagus) 3) Bleeding 4) Iron Deficiency anemia (secondary due to bleeding) 5) Dysphagia (trouble swallowing due to scarring) 6) Odynophagia: painful swallowing 7) Barrett's epithelium: increase risk of esophageal cancer |
|
|
What is most common symptom of GERD? |
Heartburn |
|
|
What are some atypical symptoms of GERD? |
cough, asthma, hoarseness, chest pain, aphthous ulcers, hiccups, dental erosions |
|
|
What are some warnings of a GERD patient beginning to get stricture? |
dysphagia, early satiety, weight loss, bleeding |
|
|
What are some questions you can ask to help figure out the presence/severity of GERD? |
Do you have heartburn? How often? How often do you cough? (Indication of barf getting into the lengths) Does sleeping flat make the heartburn worse? |
|
|
What are some lifestyle modifications for GERD? |
Diet, meal timing, Increase Head of Bed (HOB) by 6 inches with pillows Decrease in: fat, cola, chocolate, coffee, alcohol, smoking |
|
|
What are drugs that a GERD patient might take? |
1) Antacids/Calcium bicarbonate 2) H2 Blockers 3) Proton Pump inhibitors 4) Prokinetic agents |
|
|
What class of drugs does ranitidine, cimetidine and famotidine belong to? |
H2 Blockers (the -ines!) |
|
|
What class of medications does omperazole, Iasoprazole belong to? |
Proton Pump inhibitors (the azoles) |
|
|
What class of cdrugs does bethanechol belong to? |
Prokinetic agent |
|
|
What are some considerations that dentist need to make for a patient with GERD? |
1) Our job as dentists is to identify GERD, locate it in the mouth and refer back to physicians 2) Risk of aspiration with positioning or sedation 3) Dental changes due to oral acid reflux 4) Worsening symptoms |
|
|
What can dentists do that can worsen GERD? |
1) Prescribe NSAIDs 2) Lie them down in Supine position, they’re likely to get barf burp. 3) If we sedate them, it takes away their cough reflex and so barf gets into the lungs = suffocation! 4) Steroids can cause GERD over time |
|
|
Where can peptic ulcer disease occur? Which location is most common? |
20% stomach or 80%duodenum |
|
|
What is the prevalence of PUD? |
5-10% of population 100 patients in a 2000 patient practice |
|
|
What are some common etiologies for PUD? |
1) H. pylori (70-90%). 2) acid hypersecretion 3) cigarette smoking/alcohol 4) NSAID use (15-20%) 5) psychological and physical stress 6) age 30-50 7) steroid use |
|
|
What is the pathophysiology of PUD? |
H. Pylori produces urease which converts urea to NH3 and CO2 This initiates an inflammatory cascade which causes mucosal breakdown often in association with co-factors |
|
|
What are some complications of PUD? |
1) Hemorrhage..worse if on Warfarin/Coumadin 2) Perforation..peritonitis 3) Scarring...pyloric stenosis (cutting off of the pyloric sphincter from duodenum) 4) Malignant transformation: carcinoma or lymphoma |
|
|
What are some signs and symptoms of PUD? |
Pain Relief by antacids, milk or food Melena (blood in stool) due to bleeding Worsening symptoms may indicate complications such as perforation or pyloric outlet obstruction |
|
|
How is PUD diagnosed? |
1) Signs and symptoms 2) Urea Breath Test 13C (office) or 14C (lab) for Dx and response to treatment 3) Double contrast barium radiograph 4) Fibreoptic endoscopy: visualization and biopsy |
|
|
What is the treatment for PUD if NOT due to H.pylori |
H2 antagonists Proton pump inhibitors |
|
|
What is the treatment for PUD if due to H.pylori |
Triple Therapy! Antibiotics: Tetracycline and metronidazole (together) OR Amoxicillin and clarithromycin (together)
+ Proton pump inhibitors/ H2 antagonists
also may use pepto-bismol |
|
|
although triple therapy for PUD is 92-99% successful, what are some reasons treatment fails? |
Noncompliance with drug therapy Continued used of NSAIDs, alcohol, smoking Continued ingestion of spicy foods Continued stressful lifestyle |
|
|
What are some dental modifications that should be made with patient with PUD? |
Be alert of signs and symptoms. Use acetaminophen for pain control over NSAIDs whenever possible! --> If prescribing NSAIDs, consider prescribing PPIs or Misoprostol (Cytotec-protects the stomach lining!) |
|
|
Under what conditions should NSAIDs be absolutely avoided for a PUD patient? |
If the patient is over 75 patient has a history of bleeding Concomitant steroid use |
|
|
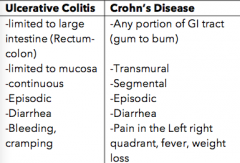
What are some differences between ulcerative colitis and Crohn's disease? |
|
|
|
What is toxic megacolon? |
Patients with ulcerative colitis have peristalsis problems which can lead to toxic megacolon (which is the potential for the intestines to explode) |
|
|
What are some oral manifestations of Crohn's? |
Ulcers in the mouth |
|
|
What are some complications of Ulcerative colitis? |
Anemia, malabsorption toxic megacolon malignant transformation more likely |
|
|
What are some complications of Crohn's disease? |
Anemia, malabsorption Fistulae, stricture Surgery more likely |
|
|
What are some treatment options for inflammatory bowel disease? |
1) Supportive Therapy: rest, fluids, lytes, nutritional supplementation 3) Immunosuppressives: methotrexate, cyclosporine 4) Antibiotics:Flagyl/Cipro |
|
|
What are some dental concerns for Inflammatory bowel disease? |
) Potential for adrenocortical suppression with steroids. Patient no longer is capable of handling stress properly. Might need supplemental prednisone Cyclosporin: used for dampening immune system but also causes renal damage. 5)Opportunistic infections / lymphoma due to immuno- suppression |
|
|
What GI disease can be caused by taking broad spectrum antibiotics? |
Pseudomembranous Colitis |
|
|
What is the organism responsible for pseudomembranous colitis? |
C. difficile |
|
|
What are some signs and symptoms of pseudomembranous colitis? |
Toxins produced by C. difficile cause pseudomembranes across the bowel. This can induce potentially lethal colitis, diarrhea. This leads to dehydration, ion disturbance and sepsis Typically develop in 4 to 10 days and you get profuse, watery diarrhea, bloody diarrhea, fever, abdominal pain and even death |
|
|
What is the risk of triggering pseudomebranous colitis if clindamycin is prescribed? |
2-20% (AVOID IF THEY"VE HAD PSEUDOMEMBRANOUS COLITIS BEFORE) |
|
|
What is the risk of triggering pseudomebranous colitis if amoxicillin is prescribed? |
5-9% |
|
|
What is the risk of triggering pseudomebranous colitis if cephalosporin is prescribed? |
<2% |
|
|
How is pseudomembranous colitis typically diagnosed? |
enterotoxin found in stool |
|
|
What is the treatment for Pseudomembranous colitis? |
Stop the offending antibiotic. Prescribe Flagyl or Vancomycin for treatment |
|
|
What questions does a dentist need to ask when they are faced with a patient with bleeding disorder? |
1) How severe is this patient’s bleeding disorder 2) Is it safe to manage without an expert advice 3) Does this patient need transfusions or anti- fibrinolytic medication? 4) Does the patient need to be assessed by a specialized dental center? |
|
|
describe the basic hemostatic process |
1) reflex vasoconstriction to ↓Blood Flow |
|
|
What are the two classifications of arthritis? |
Autoimmune: Rheumatoid arthritis Non-autoimmune: Osteoarthritis |
|
|
What is the typical age of onset for rheumatoid arthritis? |
30-50 years old |
|
|
Which gender is more likely to suffer rheumatoid arthritis? |
Females. (3:1 ratio between females and males) |
|
|
What are some signs and symptoms that indicate that a patient may have rheumatoid arthritis? |
-Morning stiffness (>1HR) -Hand joint arthritis |
|
|
Patient is on prednisone, Ibuprofen, Methotrexate and infliximab for a systemic condition. What condition is the patient likely suffering from? |
severe Rheumatoid arthritis (severe because methotrexate is only prescribed if nothing works. Really bad side effects) |
|
|
What class of drug does methotrexate and cyclosporin belong to? |
Immunosuppressive drugs |
|
|
What class of drugs are etanercept & infliximab a part of ? |
TNF-Alpha inhibitors |
|
|
Rheumatoid Arthritis patient taking prednisone, ASA, methotrexate, infliximab. What are some possible complications with associated with taking these drugs? |
ASA: peptic ulcers, bleeding Steroids: immunosuppression, adrenal suppression, Osteoporosis Methotrexate: toxic, so can have all sorts of systemic side effects including Bone marrow toxicity. Infliximab: increased risk of malignancy
|
|
|
What are some dental considerations when managing a patient with rheumatoid arthritis? |
Worse in the AM so try afternoon appointments! Short appointments with position changes Ensure comfort: pillows, etc. Immune suppression |
|
|
Rheumatoid Arthritis patient taking prednisone, ASA, methotrexate, infliximab. What are some modifications that you should make to your dental appointment based on those medications? |
1) Don't prescribe additional NSAIDs 2) May require cortical supplementation 3) TmJ may be involved. >50% of patients have pain/trismus so they may require soft diet.
|
|
|
What other autoimmune disease is rheumatoid arthritis linked with? |
Sjogren's syndrome |
|
|
What are some signs and symptoms of sjogren's syndrome? |
Dry eyes Dry mouth: increased caries, candida. Increased risk of lymphoma |
|
|
What are 3 drugs routinely prescribed to patients with osteoporosis? |
Calcium Vitamin D Bisphosphonates |
|
|
Which type of bisphosphonate is the least potent? |
Fosamax |
|
|
How long is the half life of bisphosphonates? |
10 years |
|
|
Patients on bisphosphonates are at risk of what disease? |
Bisphosphonate related osteonecrosis of the Jaw (BRONJ) |
|
|
Why do bisphosphonates increase risk for bronj? |
Bisphosphonates inhibits osteoclasts. In most cases this is good because it maintains or build up bone density. Normally, if bone is injured, Osteoclasts eat up dead bone. However, if a patient on strong dose bisphosphonates gets their tooth extracted (or via any dental procedure), they can get exposed to bacteremia, which leads to infection of the jaw. The osteoclasts don’t clean up the jaw and you end up with Bisphosphonate related Osteonecrosis of the Jaw (BRONJ). |
|
|
Which Class of Bisphosphonates patients are generally safe to do work on? |
Class A: Uncomplicated osteoporosis with oral fosamax 1/week Class B: RA patient on steroids + Fosamax (Class B...cover with antibiotics. Not sure if this is still done) |
|
|
Which Class of Bisphosphonates patients are at high risk of BRONJ? |
Class C: Patient on Zometa and other IV bisphosphonates (REFER!!) Class C+: Patient on Denosumab (1/2 life is 30 days) but still high risk!! |
|
|
Which type of seizures are dangerous to epilepsy patients? |
Grand mal seizures |
|
|
Which type of seizures are less dangerous to epilepsy patients? |
Non-convulsive (petit mal, partial complex seizures). No motor component involved |
|
|
What are some things that can trigger seizures in an epilepsy patient? |
-Forgetting to take anti-convulsant -Stress -Sleep disturbance -Hypoglycemia -Alcohol withdrawal -Other meds |
|
|
For prolonged seizure episodes (>10 minutes), what can be administered to the patient as a way to stop the sure? What do you have to be careful with regards to that medication? |
Ativan 0.05-1mg/kg IM. Be careful with respiratory depression. Be prepared to air via manual ventilator |
|
|
What are some precautions should you make for a patient with epilepsy? |
Patient must take their anticonvulsant meds -Assess frequency, triggers, patterns of epilepsy -Consider consulting neurologist or family physician |
|
|
Which demographic tends to have prologned seizures?
|
kids ( should be treated)
|
|
|
What are some methods of preventing seizures? |
-Get patients to take their anticonvulsant medication -If GA, anesthetist should be aware of seizure tendency -Check patient's pre-op convulsant levels (frequency, triggers, duration) -Consult with patient MD |
|
|
Pathophysiology of Parkinson's disease? |
a movement disorder of unknown cause that primarily affects the pigmented, dopamine containing neurons of the substantia nigra |
|
|
What are three most common manifestations of Parkinson's disease? |
Bradykinesia (slowness of movement) Rigidity Tremor (at rest) -20% of patients will also have dementia |
|
|
Why should you never take a parkinson patient off their meds pre-op? |
1) Puts the patient at much higher risk of aspiration and pneumonia 2) May develop neuroleptic malignant syndrome |
|
|
What is Neuroleptic malignant syndrome? |
Occurs if you do a sudden withdrawal of dopaminergic meds. Symptoms: Fever, movement disorder-rigidity, Altered mentation |
|
|
What are patients with Parkinsons at higher risk of developing post-op? |
Aspiration and pneumonia |
|
|
Why should you avoid giving Major tranquilizers to patients with Parkinson's disease? |
Can worsen the patient's Parkinsons! |
|
|
What is the most common cause of dementia? |
Alzheimer's |
|
|
What is a key defining feature of Alzheimer's disease? |
KRAFT (Can't remember a f***ing thing) and Most Alzheimer's patients aren't aware of their memory problems |
|
|
What is Cooper's rule of memory disturbance (regarding Alzheimer's?) |
As long as you're worried about your memory you have nothing to worry about |
|
|
list some medications that are prescribed to treat Alzheimer's and what is their mechanism of action |
Donepizil (Aricept) Rivastigmine( Exelon) Galatamine (Reminyl) MOA: Inhibits cholinesterase |
|
|
Some considerations when managing patients with Alzheimer's? |
-Greater risk of post-operative confusion (esepecially hospitalized patients) -Continuous presence of family member has a calming effect -Avoid low lighting (can lead to hallucinations) -avoid night time sedation (major tranquilizer amy be better choice) |
|
|
What is a Transient Ischemic attack? What is significant about it? |
Focal neurologic abnormalities of sudden onset and brief duration(usually minutes, never more than a few hours) that reflect dysfunction inthe distribution of either in the internal carotid-middle cerebral or the vertebral-basilar arterial system. Warning sign that stroke is going to happen |
|
|
What is often given as the first line tx of stroke? |
tPA (tissue plasminogen activator). Needs to be given within IV 3 hours of onset of stroke symptoms. Given intra-arterially within 6 hours. |
|
|
What are some meds that are often prescribed to patients who are at risk of stroke? |
Aspirin (81 or 325) Antiplatelet agents: Ticlopidine, Clopidogrel (Plavix) Warfarin (vitamin K reductase inhibitor, anticoagulant) Dabigatran (Pradaxa, factor II inhibitor, cannot be tested with INR) |
|
|
How long should you delay any elective procedures on a patient who has just had a stroke? |
2-3 months |
|
|
Should you stop a patient's aspirin before minor oral surgery? |
No! Just apply pressure / local measures. |
|
|
What value increases if there is a problem with the intrinsic pathway? |
Increase in aPTT (increased activated partial thromboplastin time) |
|
|
What value increases if there is a problem with the extrinsic pathway? |
Increase in PT (INR) PT= Prothrombin time |
|
|
What value increases if there is a problem with the common pathway? |
Increased aPTT and PT |
|
|
What is the MOA of Aspirin? |
Disrupts COX pathway (inhibits TxA2) that permanently inhibits platelet activation and aggregation. Effect cannot be measured using INR or aPTT. |
|
|
Why is it pointless to stop Aspirin the day before a extraction?
|
Platelets takes 7 days on average to turnover. |
|
|
What is the MOA of Clopidogrel and Ticlopidine? |
Inhibits ADP receptor, which normally binds ADP and activates platelets in the event of trauma. |
|
|
What medications might someone with MS be taking? |
Prednisone (usually not sufficient to cause adrenal suppression) and interferons. |
|
|
What is autonomic dysreflexia?
|
Seen in spinal cord lesions. When stimuli such as bladder distension or pressure sores can result in increased sympathetic output (e.g. sweating, hypertension etc.). |
|
|
What are some medications to treat spasticity? |
Diazepam (benzodiazepine CNS depressant), Baclofen (topical muscle relaxer), Tizanidine (alpha 2 adrenergic agonist). |
|
|
What are some major types of cerebrovascular disease? |
Cerebral insufficiency Infarction Hemorrhage Ateriovenous malformation Stroke: 80% involve the carotid system (most survivors die of atherosclerosis / myocardial disease) |
|
|
What is the standard treatment for someone with bipolar disorder? |
Antidepressants and lithium. |
|
|
What is depression? |
Affective disorder. Results in mood, loss of interest, weight gain / loss, sleep disorder, fatigue, worthlessness / hopelessness, loss of concentration, suicidal. Feel bad all the time. Can be triggered by stress or excessive grief over an extended period of time. Frequently associated with chronic pain. |
|
|
What are amitriptilline and elavil? |
Tricyclic antidepressants. Cause xerostomia. Use topical fluoride and need good oral hygiene. |
|
|
What are prozac and zoloft? |
Selective serotonin reuptake inhibitors (SSRIs). Increase serotonin in the synapse to help with depression. Also used for anxiety. Need to follow up with these patients. |
|
|
What are phenylzine and nardil? |
MAO inhibitors. Prevents the break down of monoamines in the cell. Can result in neuroleptic malignant syndrome if there is a stimuli that triggers neurotransmitter release. |
|
|
What treatment modifications would you make for someone with anxiety?
|
Give them the power to choose Assist with NO, benzodiazepines and local anesthetics |
|
|
What is Munchausen's syndrome?
|
Seen in bipolar disorder. Individual fakes illness for secondary gain or use their children to get attention. |
|
|
What is disulphram / antabuse? |
Drug used for alcoholism. Forces alcoholics to stop drinking (if they do while on this drug they will feel very sick). |
|
|
What is the treatment for trigeminal neuralgia? |
Anticonvulsant (carbamazepine) Antispasmodic (baclofen) Surgery |
|
|
What is the mechanism of action of warfarin? |
Vitamin K antagonist (inhibits vitamin K reductase) and interferes with functioning of factors II, VII, IX and X. |
|
|
What is the mechanism of action of rivaroxaban and apixaban? |
Direct factor Xa inhibitors. Apixaban is not approved in Canada. Antidote is anadaxanet. Direct oral anticoagulants have faster onset, less interactions, fixed dose, no monitoring and predictable anticoagulation. Cannot be measured using INR or aPPT. For minor dental procedures, keep on. For major dental procedures stop 1-3 days prior. |
|
|
What is the mechanism of action of dabigatran? |
Direct thrombin inhibitor. Idaracizumamab is the antidote. 80% renal clearance. Direct oral anticoagulants have faster onset, less interactions, fixed dose, no monitoring and predictable anticoagulation.Cannot be measured using INR or aPPT. For minor dental procedures, keep on. For major dental procedures stop 1-3 days prior. |
|
|
What is the mechanism of action of tranexamic aid? |
Inhibits production of plasmin (anti-thrombolytic, promotes clot). Used as oral, mouthwash (do not swallow; possible systemic effects), or IV. |
|
|
What is vonWillebrand disease? |
X-linked dominant condition with quantitative or qualitative abnormalities in vWF. Treated with factor first infusion and DDAVP (desmopressin) which stimulates release of vWF from endothelial cells. |
|
|
What is hemophilia A and B? |
A (factor VIII deficiency) B (factor IX deficiency) Treated with factor first infusion. |
|
|
What treatment modifications do you make for a patient with a bleeding disorder?
|
Factor first transfusion for larger procedures Consult hematologist |
|
|
What is idiopathic / immune thrombocytopenic purpura (ITP)? |
Bleeding disorder in which the immune system destroys platelets. Have higher risk of infection. Treat with platelet transfusion and 2g amoxicillin 2 hours before procedure. |
|
|
At what point is someone neutropenic? |
< 500 / mm3 |
|
|
At what CD4+ cell count is an individual considered to have AIDS? |
< 200 /mm3. (< 50 / mm3 is where most AIDS related deaths occur). |
|
|
What is leprosy? |
A chronic infection of skin and peripheral nerves that causes distal anesthesia of the extremities. |
|
|
What is in your emergency kit? |
Oxygen (5-6 L / min), EPI (0.5-1 mL of 1:1000 IM), nitroglycerin (0.3-0.4 tablets), ventolin puffer, benadryl (50 mg IM or PO), smarties, glucagon (1 mg IM), aspirin (325 mg chew) and lorazepam (1 mg SL). Also contains oxygen bottle, regulator, gas tubing, airways and face masks, ball valve bag, needles, syringes, tape, flashlight, tonsil suction tip and file cards with emergency protocols and drug dosages. |

