![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
134 Cards in this Set
- Front
- Back
|
What is gastro-oesophageal reflux? |
The involuntary passage of gastric contents into the oesophagus |
|
|
How common is gastro-oesophageal reflux? |
Extremely common in infancy |
|
|
Pathophysiology of gastro-oesophageal reflux? |
Caused by inappropriate relaxation of the lower oesophageal sphincter as a result of functional immaturity. A predominantly fluid diet, a mainly horizontal posture and a short intra-abdominal length of oesophagus all contribute |
|
|
When does symptomatic reflux usually resolve? |
By 12 months Presumably due to a combination of maturation of the lower oesophageal sphincter, assumption of the upright position and more solids in the diet |
|
|
What is the clinical picture of normalgastro-oesophageal reflux? |
Recurrent regurgitation or vomiting but the infant is putting on weight normally and otherwise is well |
|
|
What conditions are severe reflux common in? |
Children with cerebral palsy/other neurodevelopmental disorders Preterm infants (especially if they have coexistent bronchopulmonary dysplasia) Following surgery for oesophageal atresia or diaphragmatic hernia |
|
|
What are the investigations used ingastro-oesophageal reflux? |
Usually a clinical diagnosis however investigations can be used if the history is atypical/complications are present/failure to respond to treatment 24-hour oesophageal pH monitoring to quantify the degree of oesophageal reflux 24-hour impedence monitoring (available in some centres) – weakly acidic or non-acid reflux (which may also cause disease) is also measured Endoscopy with oesophageal biopsies – to identify oesophagitis and exclude other causes of vomiting Contrast studies of the upper GI tract – may support diagnosis but are neither sensitive nor specific. May be required to exclude underlying anatomical abnormalities in the oesophagus, stomach and duodenum and to identify malrotation. |
|
|
How is uncomplicated gastro-oesophageal refluxmanaged? |
Parental reassurance, adding inert thickening agents to feeds (e.g. Nestargel, carobel) and positioning in a 30 degree head-up prone position after feeds |
|
|
How is more significant gastro-oesophagealreflux managed? |
Acid suppression with either H2 antagonists (ranitidine) or PPI (omeprazole) Drugs which increase gastric emptying e.g. domperidone may be tried although the evidence for their use is poor Failure to respond to these measures should result in other diagnoses being considered and further investigations being performed |
|
|
When is surgery used in gastro-oesophagealreflux? |
Children with complications unresponsive to intensive medical treatment or oesophageal stricture |
|
|
What operation is performed forgastro-oesophageal reflux? |
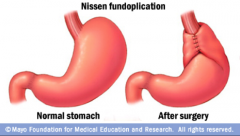
A nissen fundoplication Fundus of the stomach is wrapped around the intra-abdominal oesophagus |
|
|
What are the complications of gastro-oesophagealreflux? |
Failure to thrive (from severe vomiting) Oesophagitis – haematemesis, discomfort on feeding or heartburn, iron deficiency anaemia Barret’s oesophagus Recurrent pulmonary aspiration – recurrent pneumonia, cough or wheeze, apnoea in preterm infants Dystonic neck posturing (Sandifer syndrome) SIDS |
|
|
What are the causes of constipation inpaediatrics? |
Babies: Hischsprung disease, anorectal abnormalities, hypothyroidism, hypercalcaemia Dehydration or reduced fluid intake Anal fissure Older children: may be related to problems with toilet training, unpleasant toilets or stress |
|
|
Definition of constipation? |
The infrequent passage of dry, hardened faeces often accompanied by straining or pain May be accompanied by soiling caused by involuntary passage of faeces (overflow incontinence) or voluntary passage of faeces in an unacceptable place (encoparesis) |
|
|
Findings on examination in a child withconstipation? |
Palpable abdominal mass in a well-looking child NB – PR should only be performed by a paediatric specialist only if a pathological cause is suspected |
|
|
What are the red flag symptoms in constipationand what do they suggest? |
Failure to pass meconium within first 24 hours of life – Hirschsprung disease Failure to thrive/growth failure – Hypothyroidism, coeliac disease, other causes
Gross abdominal distension – Hirschsprung disease or other GI dysmotility Abnormal lower limb neurology or deformity – lumbosacral pathology Sacral dimple above natal cleft, over the spine – naevus, hairy patch, central pit or discoloured skin – spina bifida occulta Abnormal appearance/position/patency of anus – abnormal anorectal anatomy Perianal bruising or multiple fissures – sexual abuse Perianal fistulae, abscesses of fissures – perianal Crohn’s disease |
|
|
Differentiate between simple constipation and Hirschsprung's disease |

|
|
|
What is Hirschsprung’s disease? |
The absence of ganglion cells from the myenteric and submucosal plexuses of part of the large bowel resulting in a narrow, contracted segment The abnormal bowel extends from the rectum for a variable distance proximally, ending in normally innervated, dilated colon 75% cases – lesion confined to the rectosigmoid region 10% of cases – whole colon involved |
|
|
How does Hirschsprung’s present? |
Neonatal period (usually) Intestinal obstruction heralded by failure to pass meconium within first 24 hours of life Abdominal distension and later bile-stained vomiting occur |
|
|
Findings on rectal exam in Hirschsprung’s? |
Narrowed segment Withdrawal of the examining finger often releases a gush of liquid stool and flatus Temporary improvement in the obstruction following the dilatation caused by the rectal examination can lead to a delay in diagnosis |
|
|
How does Hirschsprung’s present a. occasionallyin infants and b. in later childhood? |
A: Severe, life-threatening Hirschsprung’s enterocolitis during the first weeks of life, sometimes due to C. difficile B: chronic constipation, usually profound and associated with abdominal distension but usually without soiling, growth failure may also be present |
|
|
How is Hirschsprung’s diagnosed? |
Suction rectal biopsy: demonstrating the absence of ganglion cells, together with the presence of large, acetylcholinesterase-positive nerve trunks Anorectal manometry or barium swallow may be useful to give the surgeon an idea of the length of the aganglionic segment but are not diagnostic |
|
|
Management of Hirschsprung’s disease? |
Surgery: initial colostomy followed by anastomosing normally innervated bowel to the anus |
|
|
FOR MANAGEMENT OF SIMPLE CONSTIPATION LOOK IN TEXTBOOK PAGE 238 |
:) - do it now |
|
|
What are the current guidelines on infant feeding? |
Infants should be breast-fed exclusively for the first 6 months of life |
|
|
When can specialised infant formulas be used? |
Cows milk protein allergy/intolerance Lactose intolerance Cystic fibrosis Neonatal cholestatic liver disease Following neonatal intestinal resection |
|
|
What are the types of specialised formulas available? |
Cow's milk-based formula Hydrolysed Semi-hydrolysed |
|
|
What does failure to thrive mean? |
Sub-optimal weight gain in infants and toddlers |
|
|
What are the categories of causes of failure to thrive? |
Inadequate intake: Organic vs non-organic/environmental Inadequate retention Malabsorption Failure to utilise nutrients Increased requirements |
|
|
Examples of organic causes of inadequate intake causing failure to thrive |
Impaired suck/swallow: oro-motor dysfunction, neuro disorder, cleft palate Chronic illness leading to anorexia e.g. Crohns, CF, liver disease, CKD etc. |
|
|
Examples of non-organic/environmental causes of inadequate intake causing failure to thrive |
Inadequate availability of food Psychosocial deprivation Neglect or child abuse |
|
|
Examples of inadequate retention causing failure to thrive |
Vomiting Severe gastro-oesophageal reflux |
|
|
Examples of malabsorption causing failure to thrive |
Coeliac disease CF Cows milk protein intolerance Cholestatic liver disease Short gut syndroe Post-necrotising enterocolitis |
|
|
Examples of failure to utilise nutrients causing failure to thrive |
Syndromes Chromosomal disorders e.g. Downs syndrome Extreme prematurity Congenital infection Metabolic disorders Storage disorders Amino and organic acid disorders |
|
|
Examples of increased requirements causing failure to thrive |
Thyrotoxicosis CF Malignancy Chronic infection (HIV) Congenital heart disease |
|
|
What are the tools that can be used for nutritional assessment? |
Anthropometry: weight, height, mid-arm circumference, skinfold thickness Lab: low plasma albumin, low concentrations of specific minerals/vitamins Food intake: dietary recall, diary Immunodeficiency: low lymphocyte count, impaired cell-mediated immunity |
|
|
What does the WHO recommend nutritional status to be expressed as? |
Weight for height Mid upper-arm circumference (MUAC) Height for age |
|
|
What is Kwashiorkor? |
Severe protein malnutrition |
|
|
Clinical presentation of Kwashiorkor? |
Generalised oedema and severe wasting 'Flaky-paint' skin rash with hyperkeratosis and desquamation Distended abdomen and enlarged liver Angular stomatitis Hair which is sparse and depigmented Diarrhoea, hypothermia, bradycardia and hypotension Low plasma albumin, potassium, glucose and magnesium |
|
|
What is coeliac disease? |
An enteropathy in which the gliadin fraction of gluten provokes a damaging immunological response in the proximal small intestine mucosa Causes villi to be come progressively shorter and then absent, leaving a flat mucosa. |
|
|
What is the classical presentation of coeliac? |
At 8-24 months after the introduction of wheat-containing weaning foods. Failure to thrive, abdominal distension, buttock wasting (and other muscles), abnormal stools and general irritiability |
|
|
What are the other presentations of coeliac? |
Mild, non-specific GI symptoms Anaemia (iron and/or folate deficiency) Growth failure/short stature Found on screening |
|
|
What are the investigations used to diagnose coeliac? |
Serology (screening) tests - IgA tissue transglutaminase antibodies and endomysial antibodies Small intestinal biopsy performed endoscopically: demonstrates mucosal changes - increased intraepithelial lymphocytes and a variable degree of villous atrophy and crypt hypertrophy |
|
|
How is coeliac disease managed? |
A diet free from wheat, rye and barley (gluten-free) Supervision by a dietician is essential In children who had a doubtful initial biopsy/response to gluten-free diet OR children who presented <2 years, a gluten challenge is required later in childhood to demonstrate disease |
|
|
What are food allergies and food intolerances? |
Allergy: A pathological immune response is mounted against a specific food protein. Usually IgE mediated but may be non-IgE mediated. Intolerance: A non-immunological hypersensitivity reaction to a specific food |
|
|
What are the symptoms of gastritis? |
Abdominal pain Nausea |
|
|
What are the causes of gastritis? |
Helicobacter pylori ++ Other infections: bacteria, parasites, viral Non-infective causes (less so in children) |
|
|
What type of gastritis does H pylori cause? |
Nodular antral gastritis |
|
|
How can H pylori gastritis be investigated for? |
Gastric antral biopsies 13C breath test Stool antigen for H pylori |
|
|
What are the symptoms of duodenal ulcers in children? |
Epigastric pain that wakes them at night |
|
|
How should peptic ulceration be treated in children? |
PPI and if H pylori eradication therapy (amoxicillin and metronidazole or clarithromycin) |
|
|
What is the cause of IBD? |
Environmental triggers in a genetically predisposed individual |
|
|
Features of Crohns? |
Growth failure Delayed puberty Classical presentation (25%): abdo pain, diarrhoea, weight loss General ill health: fever, lethargy, weight loss Extra-intestinal manifestations: oral lesions or perianal skin tags, uveitis, arthralgia, erythema nodosum In older children, lethargy and general ill health without GI symptoms can be presentation |
|
|
What can Crohns be misdiagnosed as? |
Psychological problems Anorexia nervosa |
|
|
Pathophysiology of Crohns? |
A transmural, focal, subacute or chronic inflammatory disease most commonly affecting the distal ileum or proximal colon. Initially there are areas of acutely inflamed, thickened bowel. Subsequently, strictures of the bowel and fistulae may develop between adjacent bowel loops, between bowel and skin or to other organs e.g. vagina, bladder |
|
|
How is a diagnosis of Crohns made? |
Raised inflammatory markers (ESR, CRP, platelet count) Iron deficiency anaemia Low serum albumin Upper GI endoscopy Ileocolonoscopy Small bowel imaging: narrowing, fissuring, mucosal irregularities and bowel wall thickening |
|
|
What is the histological hallmark of Crohns? |
Non-caseating epithelioid cell granulomata (not seen in up to 30% at presentation) |
|
|
How is remission induced in Crohns? |
Nutritional therapy: replace normal diet with whole protein modular feeds (polymeric diet) for 6-8 weeks (effective in 75%) Systemic steroids used if ineffective |
|
|
What treatments can be used to maintain remission? |
Immunosuppressants: azathioprine, mercaptopurine, methotrexate Anti-TNF: infliximab, adalimumab |
|
|
What treatment are used in Crohns to help correct growth failure? |
Long-term supplementary enteral nutrition to correct growth failure |
|
|
When is surgery used in Crohns? |
Complications: obstruction, fistulae, abscess formation or severe localised disease unresponsive to medical treatment |
|
|
Prognosis for Crohns? |
In general, long-term prognosis for disease beginning in childhood is good and most patients lead normal life despite occasional relapses |
|
|
How does UC characteristically present? |
Rectal bleeding Diarrhoea Colicky pain Weight loss and growth failure may occur but less frequent than in Crohns |
|
|
What are the extraintestinal complications of UC? |
Erythema nodosum Arthritis |
|
|
How is UC diagnosed? |
Upper GI endoscopy and ileocolonoscopy (Small bowel imaging to rule out Crohns) |
|
|
What is the difference between UC in adults and children? |
Most adults only have distal colon affected 90% children have pancolitis |
|
|
What does histology in UC show? |
Mucosal inflammation Crypt damage (cryptitis, architectural distortion, abscesses and crypt loss) Ulceration |
|
|
How is UC treated? |
Mild disease: aminosalicylates (balsalazide and mesalazine) are used for induction and maintenance Disease confined to rectum and sigmoid: topical steroids More aggressive/extensive disease: systemic steroids for acute exascerbations and immunodmodulatory therapy (e.g. azathioprine) to maintain remission alone or in combination with low dose corticosteroids |
|
|
How is severe fulminating UC treated? |
Medical emergency IV fluids and steroids Ciclosporin if above doesnt induce remission |
|
|
When may surgery be used in UC and what surgery? |
Severe fulminating disease which may be complicated by a toxic megacolon Chronic poorly controlled disease Colectomy with an ileostomy or ileorectal pouch |
|
|
What is there an increased incidence of with UC? |
Adenocarcinoma of the colon in adults (regular colonscopic screening is performed after 10 years from diagnosis) |
|
|
What are the causative organisms in gastroenteritis? |
Rotavirus (most common) Campylobacter jejuni Shigella Salmonella Cholera Enterotoxigenic E coli Outbreaks: adenovirus, norovirus, calicivirus, coronavirus, astrovirus |
|
|
What symptom suggests a bacterial rather than a viral cause of gastroenteritis? |
Blood in the stool |
|
|
Symptom suggestive of campylobacter jejuni gastroenteritis? |
Severe abdo pain |
|
|
Symptoms suggesting shigella or salmonella gastroenteritis? |
Dysenteric type infection Blood and pus in stool Pain Tenesmus High fever (just shigella) |
|
|
Symptom suggesting cholera or E coli gastroenteritis? |
Profuse, rapidly dehydrating diarrhoea |
|
|
Presentation of gastroenteritis? |
Sudden change to loose or watery stools often accompanied by vomiting |
|
|
What disorders can masquerade gastroenteritis? |
Systemic infection: meningitis, septicaemia Local infections: resp tract, hep A, UTI, otitis med Surgical disorders: pyloric stenosis, intus, append, NEC, Hirschprung Metabolic: DKA Renal: HUS Other: coeliac, cows milk protein intol, adrenal insufficiency |
|
|
What is the most serious complication of gastroenteritis? |
DEHYDRATION |
|
|
Which children are at increased risk of dehydration? |
Infants (particularly <6m or low birthweight) Passed >6 diarrhoeal stools in 24h Vomited 3+ times in 24h Unable to tolerate/not offered extra fluids Malnutrition |
|
|
Why are infants at particular risk of dehydration? |
Greater surface area to weight ratio leading to greater insensible water loss Higher basal fluid requirements Immature renal tubular reabsorption Unable to obtain fluids for themselves |
|
|
What is the most accurate measure of dehydration in gastroenteritis and how are the results classified? |
Degree of weight loss during the diarrhoeal illness No clinically detectable dehydration: <5% body weight Clinical dehydration: 5-10% body weight Shock: >10% body weight |
|
|
What are the red flags signs in a clinically dehydrated child/infant for shock? |
Deteriorating general appearance Altered responsiveness e.g. lethargic Sunken eyes Tachycardia Tachypnoea Reduced skin turgor |
|
|
What investigations are used in gastroenteritis? |
Usually one Plasma electrolytes, urea, creatinine and glucose if IV fluids required or features suggesting hypernatremia Blood cultures if abx used |
|
|
Management of gastroenteritis? |
**Treat the dehydration if present** Supportive ?Abx Increased nutritional intake following diarrhoeal illness |
|
|
When are antibiotics indicated in gastroenteritis? |
Suspected/confirmed sepsis Extra-intestinal spread of bacterial infection Salmonella gastroenteritis if <6m Malnourished children Immunocompromised Specific bacterial/protozoal infections: C. diff associated with pseudomembranous colitis, cholera, shigellosis, giardiasis |
|
|
When are anti-emetics and anti-diarrhoeal drugs used in gastroenteritis? |
Never They are ineffective, may prolong excretion of bacteria in stools, have SEs, add unnecessarily to cost |
|
|
Explain IV therapy for rehydration |
Resus fluids: 20 ml/kg over less than 10 minutes. Then maintenance fluids: 4-2-1 rule 0-10kg: 4ml/kg/hr 10-20kg: 2ml/kg/hr 20+ kg: 1ml/kg/hr |
|
|
Signs of shock? |
Appears unwell or deteriorating Decreased level of consciousness Decreased urine output Pale or mottled skin Cold extremities Grossly sunken eyes Dry mucous membranes Tachycardia Tachypnoea Weak peripheral pulses Prolonged cap refill time Reduced skin turgor Hypotension |
|
|
Define functional abdominal pain (aka recurrent abdo pain) |
Pain sufficient to interrupt normal activities and lasts for at least 3 months |
|
|
Characteristic presentation of functional abdominal pain |
Periumbilical pain Child is otherwise entirely well |
|
|
What are the causes of functional abdominal pain? |
>90% no structural cause identified GI: IBS, constipation, non-ulcer dyspepsia, abdominal migraine, gastritis and peptic ulceration, IBD, malrotation Gynae: dysmenorrhoea, ovarian cysts, PID Psycho: bullying, abuse, stress etc. HPB: hepatitis, gall stones, pancreatitis Urinary: UTI, pelvi-ureteric junction obstruction |
|
|
What are the S&S that suggest organic disease causing recurrent abdominal pain? |
Epigastric pain at night and haematemesis (duodenal ulcer) Diarrhoea, weight loss, growth failure, blood in stools (IBD) Vomiting (pancreatitis) Jaundice (liver disease) Dysuria, secondary enuresis (UTI) Bilious vomiting and abdo distension (malrotation) |
|
|
Management of functional abdominal pain |
Identify any serious cause without subjecting the child to unnecessary investigation while providing reassurance to the child and parents |
|
|
Investigations in functional abdominal pain |
Urine microscopy and culture (mandatory) Abdo USS: rule out gall stones and PUJ obstruction |
|
|
Long-term prognosis of functional abdominal pain |
About 1/2 of affected children become rapidly free of symptoms 1/4 symptoms take a while to resolve 1/4 symptoms continue or return in adulthood as migraine, IBS or functional dyspepsia |
|
|
Which age range does toddler diarrhoea affect? |
3-5y |
|
|
Presentation of toddler diarrhoea? |
Stools of varying consistency: some well formed and some explosive and loose Presence of undigested veg in stool Child otherwise well and thriving Increased flatulence |
|
|
Management of toddler diarrhoea? |
Advise diet high in fat and fibre Avoid fruit juice Reassurance from more serious causes of diarrhoea |
|
|
What is mesenteric adenitis? |
Inflammation of the mesenteric lymph nodes (cluster of three or more lymph nodes, each measuring 5 mm or greater detected in the right lower quadrant mesentery) May be acute or chronic, depending on the causative agent, |
|
|
Presentation of mesenteric adenitis? |
Can mimic appendicitis Abdominal pain - Often right lower quadrant (RLQ) but may be more diffuse Fever Diarrhoea Malaise Anorexia Concomitant or antecedent upper respiratory tract infection Nausea and vomiting (which generally precedes abdominal pain, as compared to the sequence in appendicitis) |
|
|
Causes of mesenteric adenitis |
Beta-hemolytic streptococcus, Staphylococcus species, Escherichia coli, Streptococcus viridans, Yersinia species (responsible for most cases currently), Mycobacterium tuberculosis, Giardia lamblia, Non– Salmonella typhoid. Viruses, such as coxsackieviruses (A and B), rubeola virus, and adenovirus Infectious Epstein-Barr virus (EBV), acute human immunodeficiency virus (HIV) infection, and catscratch disease (CSD). |
|
|
Ddx of mesenteric adenitis? |
Meckel diverticulitis Intestinal duplication Regional enteritis Intussusception Intestinal lymphoma Other causes of acute abdomen (eg, porphyria, sickle cell vaso-occlusive crises, cecal tumor, familial Mediterranean fever) |
|
|
What is biliary atresia? |
A progressive disease in which there is destruction or absence of the extrahepatic biliary tree and intrahepatic biliary ducts |
|
|
Presentation of biliary atresia |
Prolonged (persistent) jaundice (mild) Normal birthweight but fail to thrive Following meconium passage, stools are pale Dark urine Hepatomegaly Splenomegaly secondary to portal HTN |
|
|
Investigations in biliary atresia |
LFTs of little value Fasting abdo USS may show contracted/absent gallbladder Radioisotope scan with TIBIDA shows good uptake by liver but no excretion into bowel Liver biopsy - features of extrahepatic obstruction but features overlap with neonatal hepatitis Diagnosis made at laparotomy by operative cholangiography which fails to outline a normal biliary tree |
|
|
Management of biliary atresia? |
Kasai procedure: hepatoportoenterostomy (jejunum anastomosed to porta hepatis to bypass fibrotic ducts) If performed <60 days, 80% of children achieve bile drainage |
|
|
Aetiology of viral hepatitis? |
Hep A, B, C, D, E Epstein-barr virus |
|
|
Presentation of viral hepatitis? |
Nausea and vomiting Abdo pain Lethargy Jaundice (30-50% have no jaundice) Large, tender liver Splenomeg common |
|
|
Importance of checking stools in a baby with jaundice? |
If jaundice is conjugated hyperbilirubinaemia (AKA there is a bile duct problem) – the baby will pass dark urine and pale stools, as conjugated bilirubin is water soluble |
|
|
Causes of jaundice in babies <24h old |
Usually haemolytic disorders: Rhesus incompatibility ABO incompatibility G6PD deficiency Spherocytosis, pyruvate kinase deficiency Congenital infection |
|
|
Causes of jaundice in 24h - 2w |
Physiological Breast milk jaundice Infection, particularly UTI Haemolysis: G6PD def, ABO incompat etc. Bruising and polycythaemia can exascerbate j Crigler-Najjar (v rare) |
|
|
Causes of unconjugated jaundice >2w (persistent jaundice) |
Physiological or breast milk jaundice Infection (especially UTI) Congenital hypothyroidism Haemolytic anaemia High GI obstruction eg. pyloric stenosis |
|
|
Causes of conjugated jaundice >2 w (prolonged) |
Bile duct obstruction: biliary atresia, choledocal cyst Neonatal hepatitis (loads of things) |
|
|
Where is the problem in unconjugated jaundice? |
Pre-hepatic Hepatocellular |
|
|
Where is the problem in conjugated jaundice? |
Hepatocellular Intrahepatic obstruction Extrahepatic obstruction |
|
|
What % of newborn infants are jaundiced and why? |
50% Marked physiological release of Hb from RBC breakdown because of high Hb conc at birth RBC life span much shorter (70 days) than adult Hepatic bilirubin metabolism is less efficient in first few days of life |
|
|
Why is neonatal jaundice important? |
May be a sign of another disorder Unconjugated bilirubin can be deposited in the brain causing kernicterus |
|
|
What is kernicterus? |
An encephalopathy resulting from the deposition of unconjugated bilirubin (fat soluble so crosses BBB) in the basal ganglia and brain stem Neurotoxic effects vary from transient disturbance to severe damage and death Acute: lethargy and poor feeding Severe cases: irritability, increased muscle tone -> arched back (opisthotonos), seizures and coma |
|
|
When do babies become clinically jaundiced? |
When bilirubin levels reach 80 umol/L |
|
|
How can jaundice be investigated? |
Look for jaundice: blanch skin with finger If jaundiced - transcutaneous bilirubin meter or blood sample to check bilirubin levels A high transcutaneous bilirubin level must be checked with a blood lab measurement |
|
|
How is jaundice managed? |
Encourage hydration (poor milk intake and dehydration may exascerbate jaundice) Phototherapy Exchange transfusion |
|
|
How does phototherapy work in jaundice? |
Light from the blue-green band of the visible spectrum converts unconjugated bilirubin into a harmless water-soluble pigment excreted predominantly in urine Delivered by an over-head light source - this is disruptive to normal nursing |
|
|
SEs of phototherapy for jaundice? |
Temperature instability as child undressed Macular rash and bronze discolouration of the skin if conjugated jaundice |
|
|
When is exchange transfusion required for jaundice? |
If the bilirubin rises to levels which are considered potentially dangerous |
|
|
How will an infant with rhesus haemolytic disease present if not identified antenatally and monitored/managed? |
Anaemia Hydrops Hepatosplenomegaly Rapidly developing severe jaundice |
|
|
Features of ABO incompatibility causing jaundice |
Jaundice usually peaks 12-72h Can cause severe jaundice but not as severe as rhesus Infants Hb level is usually normal or only slightly reduced Coombs test: direct antibody test that demonstrates anitbody on surface of RBCs is positive |
|
|
Features of congenital infection causing jaundice |
Conjugated jaundice Other abnormal clinical signs: growth restriction, hepatosplenomegaly and thrombocytopenic purpura |
|
|
Explain breast milk jaundice |
Jaundice more common and more prolonged in breast-fed infants Unconjugated Multifactorial but may involve increased enterohepatic circulation of bilirubin |
|
|
Features of infection causing jaundice |
An infected baby may develop an unconjugated hyperbilirubinaemia from poor fluid intake, haemolysis, reduced hepatic function and an increase in the enterohepatic circulation In particular a UTI may present this way |
|
|
What is malabsorption? |
Any disorder affecting the digestion or absorption of nutrients |
|
|
How does malabsorption manifest? |
Abnormal stools Failure to thrive or poor growth Specific nutrient deficiencies (either singly or in combination) |
|
|
DDx of malabsorption |
Mucosal issues: Coeliac Crohns Folate and B12 deficiency Infection: TB and parasites (ask about foreign travel) Amyloidosis Inadequate digestion: CF Chronic pancreatitis Lactose intolerance Pancreatic insufficiency Drugs Endocrine/metabolic Hyperthyroidism Adrenal insufficiency DM Hypoparathyroidism Acute gastroenteritis may cause transient malabsorption |
|
|
Investigations in malabsorption |
Stool analysis Urinalysis FBC etc. Coeliac serological screening test |

