![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
41 Cards in this Set
- Front
- Back
|
What is the mode of transmission of hepatitis B?
|
vertical transmission (common worldwide but uncommon in Africa)
- related to the HBV replicative state of the mother (90% HbeAg+, 30% HbeAg−ve) horizontal transmission(common in africa) IV route-transfusion, IVDU. Sexual contacts. |
|
|
Can you transmit hep B from breastfeeding?
|
No
|
|
|
what is the hep B virus?
|
A DNA virus-partially double stranded.
|
|
|
Is the virus itself cytopathic?
|
No.HBV is not directly cytopathic.The liver damage produced is by the cellular immune response of the host.
|
|
|
Which genotype has the worse outcome.
|
Genotype C.
|
|
|
which genotype is more responsive to interferon?
|
Genotype A and B.
|
|
|
What happens in a precore mutation of Hepatitis B?
|
No production of HBeAg
HBsAg non affected. To detect infectivity, HBV DNA must always be measured. |
|
|
What did the REVEAL study show?
|
The study showed that the risk of HCC was related to levels of HBV DNA rather than a raised ALT.
|
|
|
What is the body's immune response to Hep b infection?
|
Th1 response clears the virus
Th2 response is responsible for the chronicity of the disease. |
|
|
What are the phases of chronic HBV infection?
|
Replicative phase
Integrated phase |
|
|
what happens in the replicative phase?
|
Active viral replication
HBeAg and HBV DNA positive. patient is highly infectious. |
|
|
what happens in the integrated phase?
|
the viral genome integrates with host DNA.
HBeAg negative. HBV DNA low HBeAb positive. |
|
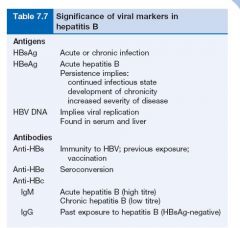
What is the significance of viral markers in Hep B
|
As per table 7.7.
|
|
|
What is the marker of acute hep B infection?
|
Presence of anti-HBc IgM.
|
|
|
Which marker is the most sensitive index of viral replication?
|
HBV DNA
|
|

Interpret the following graft.
|

Antigens:
HBsAg appears in the blood from about 6 weeks to 3 months after an acute infection and then disappears. HBeAg rises early and usually declines rapidly. Antibodies: Anti-HBc is the first antibody to appear and high titres of IgM anti-HBc suggest an acute and continuing viral replication. It persists for many months. IgM anti-HBc may be the only serological indicator of recent HBV infection in a period when HBsAg has disappeared and anti-HBs is not detectable in the serum. Anti-HBe appears after the anti-HBc and its appearance relates to a decreased infectivity, i.e. a low risk. Anti-HBs appears late and indicates immunity. |
|
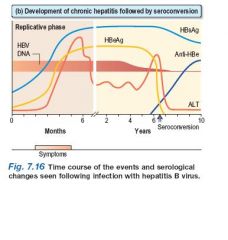
Interpret the following graft.
|
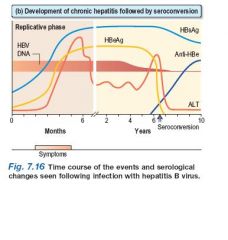
(b) Development of chronic hepatitis followed by
seroconversion HBsAg persists and indicates a chronic infection (or carrier state). HBeAg persists and correlates with increased severity and infectivity and the development of chronic liver disease. When anti-HBe develops (seroconversion) the Ag disappears and there is a rise in ALT. HBV DNA suggests continual viral replication. |
|
|
What is the treatment for acute hepatitis?
|
Mainly symptomatic.1-10% progress to inactive chronic HBV infection.
|
|
|
what are the viral markers of inactive chronic HBV infection?
|
HBsAg positive
HBeAg negative HBe Ab positive HBV DNA in low levels. normal or slightly raised ALT,AST. |
|
|
what are the viral markers of active chronic HBV infection?
|
HBs Ag positive
HBe Ag positive** HBV DNA positive. Raised AST,ALT Liver biopsy shows chronic hepatitis. ** unless a mutant virus is involved. |
|
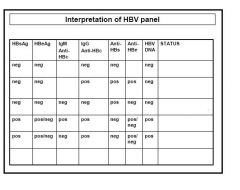
Interpret these HBV panels
|
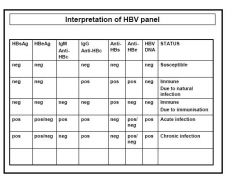
Main features:
1) Active Hep B infection-Must be HBsAg positive and IgM HBcAb positive. 2) Chronic Hep B infection-Must be HBsAg positive and IgM HBcAb negative. 3) Past Hep B infection Must have HBsAg negative, HBeAb positive, IgG HBcAb positive. 4) Previous Hep B vaccination: Must have HBsAg negative, IgG HBcAb negative. HINT: First look at HBsAg. Secondly look at: IgM HBcAb, if HBsAg +ve. IgG HBcAb, if HBsAg -ve. |
|
|
Who to treat?
|
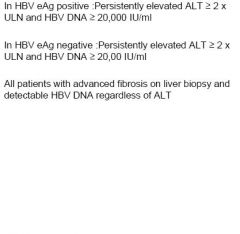
|
|
|
what is the aim of treatment?
|
Seroconversion of HBeAg
Reduction of HBV DNA to undetectable levels by PCR. |
|
|
Name the antiviral agents for treatment of Hep B?
|
Pegylated Interferon
Lamivudine Adefovir Tenofovir Entecavir (PILATE) |
|
|
which patients should not receive interferon?
|
Patients with cirrhosis.(Child-Pugh category C status)
|
|
|
what are the side effects of interferon?
|
flu-like illness
malaise headache myalgia depression reversible hair loss bone marrow depression |
|
|
what factors predicts good response to treatment?
|
short duration of disease
high ALT,AST Active liver disease on histology Low HBV DNA levels Absence of immunosuppression Female Adult acquired Delta virus negative Rapidity of response to oral therapy. |
|
|
If a patient responds poorly to interferon,(ie: HBeAg negative disease) what is the next option?
|
Lamivudine
-But by 4 years 80% develop viral resistance due to YMDD mutant. Entecavir more effective than lamivudine. Tenofovir is effective against lamivudine resistant virus. |
|
|
how long is the duration of treatment with interferon?
|
1 year.
|
|
|
What is the reason for viral resistance?
|
Monotherapy.
|
|
|
What is the reason for not responding to Lamivudine by 4 years of treatment?
|
80% develop resistance due to YMDD mutant.
|
|
|
How to confirm a co-infection of HDV and HBV?
|
Confirmed by finding serum IgM anti-HDV in the presence of IgM anti-HBc.
|
|
|
What is the early marker of HDV infection?
|
HDV RNA
|
|
|
what type of virus is the Hepatitis D virus?
|
RNA virus.
|
|
|
what is the significance of Hep D virus co-infection with Hep B?
|
Acute HBV and HDV co-infection tends to be more severe than acute HBV infection alone.
Likely to result in fulminant hepatitis. treatment is with interferon for 12 months.but response is poor. |
|
|
In cell injury, what type of immune response is stimulated?
|
T cell response.
|
|
|
What are the extrahepatic manifestations of Hep B infection?
|
Serum sickness like syndrome
Polyarteritis nodosa Glomerular disease |
|
|
What is the percentage of patients with chronic hep b that will progress to cirrhosis?
|
20% will develop cirrhosis.
|
|
|
A patient receives vaccination for Hep B with 6 doses but is still HBs Ab negative.
Now comes in contact with a patient with active Hep B. What should be the next step? |
Assume non protected.
Treat with HB immunoglobulin. |
|
|
A patient has had 3 doses of Hep B vaccine and is found to be HBs Ab negative.
What should be the next step? |
Give added doses.
(95-99% achieve titre anti-HBs >10mlU/ml after 3 doses.) 50% will respond to added doses. (Up to 6 doses) |
|
|
A patient received 3 doses of Hep B vaccine 10 years ago and was found to be HBs Ab positive.
Repeat testing the following year reveals he is now HBs Ab negative. What should happen next? |
No action required.
Anti-HBs titre falls with time 60% of responders will have no antibodies at 12 months They are still immune.No need for boosters. |

