![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
97 Cards in this Set
- Front
- Back
|
Case: A 35 year old asthmatic woman complains of chronic nasal congestion that is worse int he spring and the fall.
What is the most likely diagnosis? |
Allergic rhinitis |
|
|
Case: A 35 year old asthmatic woman complains of chronic nasal congestion that is worse int he spring and the fall.
What is the next step in management of this patient? |
Treat with antihistamines, decongestants, or intranasal steroids. These treatments can also be used in combination with each other. |
|
|
Case: A 35 year old asthmatic woman complains of chronic nasal congestion that is worse int he spring and the fall.
What are important considerations and possible complications of therapy? |
Recognition and reduction of potential allergen exposure will yield more success in management than pharmacotherapy alone. Excessive use of topical decongestants can cause rebound congestion. |
|
|
What is the classic history associated with allergies? |
- Itchy eyes - Nasal congestion and discharge - Seasonal in nature (worse in spring and fall) |
|
|
What are the classic physical exam findings associated with allergies? |
- Swollen (boggy) mucosa of nasal turbinates with a pale, bluish-gray color - Thin and watery secretions |
|
|
What treatment of allergic rhinitis offers the most consistent symptomatic relief? |
Nasal corticosteroids |
|
|
What is allergic rhinitis? |
Inflammation of the nasal passages caused by allergic reaction to airborne substances |
|
|
What is anaphylaxis? |
Rapidly progressing, life-threatening allergic reaction, mediated by immunoglobulin E (IgE) immediate hypersensitivity reaction |
|
|
What is "rhinitis"? |
Inflammation of the nasal membranes - characterized by sneezing, nasal congestion, nasal itching, and rhinorrhea
Eyes, ears, sinuses, and throat can also be involved |
|
|
What is the most common cause of rhinitis? |
Allergic (in up to 20% of population) |
|
|
What causes allergic rhinitis? |
Exposure to certain foreign proteins leads to allergic sensitization --> production of IgE directed against these proteins --> IgE coats surface of mast cells (in nasal mucosa) --> when specific allergen is inhaled into nose it can bind to the IgE int he mast cells, leading to the delayed release of a number of mediators |
|
|
What mediators get released immediately in an allergic reaction? |
- Histamine - Tryptase - Chymase - Kinase |
|
|
What mediators get released from mast cells in an allergic reaction? |
- Leukotrienes - Prostaglandin D2 |
|
|
What causes congestion in allergic rhinitis? |
Vasodilation |
|
|
What causes increased secretions in allergic rhinitis? |
Stimulation of mucus glands |
|
|
What causes sneezing and itching in allergic rhinitis? |
Stimulation of sensory nerves |
|
|
What is the function of the mediators that are released immediately after exposure to an allergen? |
Over the next 4-8 hours, mediators recruit neutrophils, eosinophils, lymphocytes, and macrophages to mucosa --> these cause more congestion and mucus production that may persist for hours or days |
|
|
What are the systemic effects following allergen exposure? |
- Fatigue - Sleepiness - Malaise |
|
|
What historical facts should you assess in a patient you think may have allergic rhinitis? |
- Try to identify specific triggers - Ask about the nature, duration, and time course of symptoms - Ask about recent use of medications - Ask about family history of allergic diseases, environmental exposures, and comorbid conditions - Time pattern of symptoms |
|
|
If a patient has allergic rhinitis all year, what is this called? |
Perennial Rhinitis |
|
|
If a patient has allergic rhinitis during specific seasons, what is it called? |
Seasonal Rhinitis |
|
|
If a patient has allergic rhinitis in relation to a workplace, what is it called? |
Occupational Rhinitis |
|
|
What are potential trigger factors of allergic rhinitis? |
- Pollen - Mold spores - Specific animals - Cleaning of the house |
|
|
What are potential irritant triggers that can worsen symptoms of allergic rhinitis? |
- Smoke - Pollution - Strong smells |
|
|
Response to what class of medications supports the diagnosis of allergic rhinitis? |
Anti-histamines |
|
|
What is a common finding near the eyes in patients with allergies? |

"Allergic shiners" - dark circles around the eyes related to vasodilation or nasal congestion
Dennie-Morgan lines (prominent creases below the inferior eyelid) are also associated with allergic rhinitis |
|
|
What is a common finding near the nose in patients with allergies? |
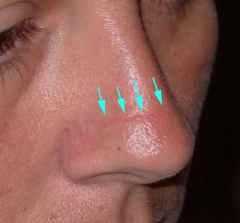
"Nasal crease" - horizontal crease across the lower half of the bridge of the nose caused by repeated upward rubbing of the tip of the nose by the palm of the hand ("allergic salute") |
|
|
What is the classic appearance of nasal mucosa in a patient with allergic rhinitis? |
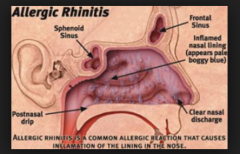
- Swollen (boggy) - Pale bluish-gray color - Thin and watery secretions (vs. thick/purulent is usually associated with sinusitis), however thick, purulent, colored mucus may be in allergic rhinitis |
|
|
After evaluating the nasal mucosa for swelling, color, and secretions, what should you check for? |
Inspect for growths such as polyps or tumors - Polyps are firm, gray masses that are often attached by a stalk, which may not be visible
Inspect the nasal septum for deviation of perforation that may be caused by chronic rhinitis, granulomatous disease, cocaine abuse, prior surgery, topical decongestant abuse, or rarely topical steroid overuse |
|
|
How can you determine if someone has a nasal polyp if you can't visualize a stalk? |
Spray topical decongestant, polyp will not shrink (whereas the surrounding nasal mucosa will shrink) |
|
|
What can cause a nasal septal perforation? |
- Chronic rhinitis - Granulomatous disease - Cocaine abuse - Prior surgery - Topical decongestant abuse - Rarely topical steroid overuse |
|
|
Why should you look in the ears of a patient with allergic rhinitis? |
Look for tympanic membrane retraction, air-fluid levels, or bubbles
These findings can be associated with allergic rhinitis, particularly if eustachian tube dysfunction or secondary otitis media is present |
|
|
What should you look for on ocular exam in a patient with allergic rhinitis? |
Look for findings of "injection" and swelling of the palpebral conjunctivae, with excess tear production |
|
|
What finding on the pharynx may be present in patients with allergic rhinitis? |
"Cobblestoning" of the posterior pharynx is often observed. This is caused by the presence of streaks of lymphoid tissue on the posterior pharynx. Tonsillar hypertrophy can also be seen. |
|
|
What should you look for on a neck exam in a patient with allergic rhinitis? |
Check for lymphadenopathy |
|
|
What should you look for on a respiratory exam in a patient with allergic rhinitis? |
Check for findings consistent with asthma - wheezing, tachypnea, and a prolonged expiratory phase of respiration |
|
|
What are the common causes of allergic rhinitis? |
- Pollens (tree, grass, weed) - House dust mites - Animals |
|
|
When is tree pollen the worst? |
During the spring (although some species are in the fall) |
|
|
When is grass pollen the worst? |
Usually late spring through fall (but can be present year round in warmer climates) |
|
|
Do many people have allergies to just one type of grass? Why or why not? |
No, many grasses are cross-reactive, meaning they have similar antigenic structures (ie, proteins recognized by specific IgE in allergic sensitization)
Consequently, a person who is allergic to one species is also likely to be sensitive to a number of other species |
|
|
When are weed allergens most prominent? |
Most prominent in late summer and fall (eg, ragweed), but some are prominent all year in warmer climates |
|
|
What typically causes perennial allergic rhinitis? |
Allergens within the home
Also by outdoor allergens present year-round (eg, grass pollens in warmer climates)
Also by trees/grass in warmer months and molds/weeds in winter |
|
|
Name the pollens and when they are most prominent. |
- Tree: spring, fall - Grass: late spring through fall - Weeds: late summer and fall |
|
|
Where are house dust mites found? |
- Carpets - Upholstered furniture - Pillows - Mattresses - Comforters - Stuffed toys |
|
|
What allows dust mites to live in houses? |
They feed on the death skin cells that are shed from humans and pets |
|
|
How can you reduce exposure to dust mites? |
Carpet removal
No benefit to using mite-proof mattresses or pillow covers |
|
|
What animals can cause allergic rhinitis? |
- Dogs and cats - Birds - Cockroaches - Rodents |
|
|
What are the treatment modalities for allergic rhinitis? |
- Patient education - Allergen avoidance - Pharmacologic management - Immunotherapy |
|
|
What are the pharmacotherapy options for allergic rhinitis? |
- Antihistamines - Decongestants - Intranasal corticosteroids - Systemic corticosteroids (severe cases) |
|
|
What is the mechanism of antihistamines? |
Competitively antagonize histamine receptors (histamine is released from mast cells) |
|
|
What are the first generation antihistamines? |
- Diphenhydramine (Benadryl) - Chlorpheniramine - Hydroxyzine |
|
|
What are the side effects of the first generation antihistamines? |
- Sedation - Anticholinergic effects: dry mouth, dry eyes, blurred vision, urinary retention (need to monitor especially in elderly!) |
|
|
What are the second generation antihistamines? |
- Loratadine (Claritin) - Desloratadine (Clarinex) - Fexofenadine (Allegra) - Cetirizine (Zyrtec) |
|
|
What are the benefits of the second generation antihistamines? |
- Lower penetration into CNS, resulting in lower incidence of sedation as a side effect (except for cetirizine) - Fewer anticholinergic effects |
|
|
What are the downsides of the second generation antihistamines? |
More expensive |
|
|
How quickly do the oral antihistamines take to work? |
Within 15-30 minutes |
|
|
Oral antihistamines are best suited for what situation? |
Patients with mild and intermittent symptoms |
|
|
How can decongestants be delivered? |
Orally or Intranasally |
|
|
What is the mechanism of action of decongestants? |
Alpha-adrenoreceptor agonist --> constricts blood vessels in the nasal mucosa and reduce overall volume of mucosa |
|
|
What is the most commonly used decongestant? |
Pseudophedrine |
|
|
What are the side effects of decongestants (pseudophedrine)? |
- Tachycardia - Tremors - Insomnia - Rebound hyperemia and worsening of symptoms with chronic use or upon discontinuation of nasal decongestants |
|
|
What is the most effective treatment and first-line therapy for the long-term management of mild to moderate persistent symptoms of allergic rhinitis? |
Corticosteroid nasal sprays |
|
|
What is the mechanism of action of corticosteroid nasal sprays? |
Reduce production of inflammatory mediators and the recruitment of inflammatory cells |
|
|
Why is it ok to use corticosteroid nasal sprays long-term? |
Systemic absorption of the steroid is relatively low, reducing the risk of complications associated with chronic use of systemic corticosteroids |
|
|
What are the potential side effects of corticosteroid nasal sprays? |
- Nosebleeds - Pharyngitis - Upper respiratory tract infections - Max effectiveness is achieved after 2-4 weeks of use |
|
|
What meds are indicated both for allergic rhinitis and for maintenance therapy for persistent asthma? Mechanism? |
Leukotriene inhibitors: Zafirlukast, Montelukast, and Zileuton |
|
|
What are the indications for Zafirlukast, Montelukast, and Zileuton? |
- Allergic rhinitis - Maintenance therapy for persistent asthma - Particularly useful in patients with both asthma and allergies or in those whose asthma is triggered by allergens |
|
|
How does the efficacy of corticosteroid nasal spray compare to leukotriene inhibitors? |
Corticosteroid nasal sprays are more effective |
|
|
When are oral corticosteroids indicated for allergic rhinitis? |
Only for severe allergies and are used in the lowest possible dose for the shortest possible time |
|
|
What can long-term oral corticosteroid therapy cause? |
- Suppression of the HPA axis - Hyperglycemia - Peptic ulcer formation - Increased susceptibility to infection - Poor wound healing - Reduction of bone density |
|
|
What therapy can be attempted in patients who remain symptomatic despite maximal medical therapy? |
Desensitization therapy |
|
|
What are the steps of desensitization therapy? |
(1) Test for specific antigens to which the patient is allergic (2) Inject the patient with highly diluted concentrations of this antigen (3) The concentration of the antigen is gradually increased, in an effort to reduce the patient's inflammatory response to the antigen(s) (4) Injections are typically given weekly or biweekly |
|
|
What is the downside of desensitization therapy? |
- Injections are typically given weekly or biweekly, therefore it is a time-consuming process - It is expensive - Must be prepared to address severe, even anaphylactic, reactions that may occur during the process |
|
|
What is urticaria? |

Large, irregularly shaped, pruritic, erythematous wheals |
|
|
What is angioedema? |

Painless, deep, subcutaneous swelling that often involves the periorbital, circumoral, and facial regions |
|
|
What is anaphylaxis? |
Systemic reaction with cutaneous symptoms that is associated with dyspnea, visceral edema, and hypotension |
|
|
What causes anaphylaxis? |
- Widespread vasodilation --> hypotension / shock - Bronchospasm or laryngeal edema --> respiratory distress - GI and uterine muscle contraction - Urticaria - Angioedema |
|
|
What should be done at the first suspicion of anaphylaxis? |
Aqueous epinephrine 1:1000, in a dose of 0.2-0.5 mL (0.2-0.5 mg) is injected subcutaneously or intramuscularly
Repeat every 15-30 minutes as necessary |
|
|
Besides giving epinephrine, what other treatment modalities are important for treating anaphylaxis? |
- Rapid IV infusion of large volumes of fluids (saline, LR, plasma or plasma expanders) - Endotracheal intubation may be necessary or the bronchospasm may respond to subcutaneous epinephrine or terbutaline - Antihistamines may be useful adjuvant therapies for alleviating cutaneous manifestations of urticaria or angioedema and pruritus - Need to monitor all patients with anaphylaxis for a period of time (eg, 24 hours) |
|
|
What is the most common eye disease seen in community medicine? |
Conjunctivitis |
|
|
What is conjunctivitis? |
Infection of the palpebral and/or bulbar conjunctiva |
|
|
What causes conjunctivitis? |
- Usually bacterial or viral infection - Other causes are allergy and chemical irritants |
|
|
How is conjunctivitis typically spread? |
From direct contact to the opposite eye or to other persons via fingers, towels, or hankerchiefs |
|
|
What are the most common bacterial causes of conjunctivitis? |
- Staphylococcus - Streptococcus - Haemophilus - Moraxella - Pseudomonas |
|
|
In severe cases how should conjunctivitis be worked up? |
May need exam of stained conjunctival scrapings and cultures |
|
|
What is the time course of conjunctivitis? With treatment? |
- Untreated it will last only 10-14 days - A sulfonamide instilled locally TID will usually clear the infection in 2-3 days |
|
|
What is "pink eye"? |
Epidemic keratoconjunctivitis - highly contagious and spread by person-to-person contact of fomites |
|
|
What is the most common cause of "pink eye"? |
Adenovirus |
|
|
What is "pink eye" associated with? |
- Pharyngitis - Fever - Malaise - Pre-auricular lymphadenopathy |
|
|
What is the presentation of "pink eye"? |
Palpebral conjunctiva is red with a copious watery discharge and scanty exudates |
|
|
How should you treat "pink eye"? |
- Local sulfonamide therapy might prevent secondary bacterial infection - Hot compresses reduce discomfort of associated lid edema - Weak topical steroids may be necessary to treat the corneal infiltrates |
|
|
How long does a course of "pink eye" typically last? |
At least 2 weeks |
|
|
What are the symptoms of allergic conjunctivitis? |
- Itching - Tearing - Redness - Stringy discharge - Sometimes photophobia |
|
|
How do you treat allergic conjunctivitis? |
Oral antihistamines or topical antihistamines or anti-inflammatory eye drops |
|
|
A 30-year old man has both mild persistent asthma and chronic environmental allergies. What medication is indicated for management of both of these conditions? |
Oral montelukast (leukotriene modifier)
|
|
|
A 12-year old adolescent male presents with eye itching and redness. He has clear drainage from his eyes but no crusting. Exam today is normal except for mildly injected conjunctiva bilaterally. What is the most appropriate treatment? |
Anti-inflammatory eye drops
This patient has allergic conjunctivitis. Topical anti-inflammatory drops are appropriate. Other options are topical or oral antihistamines. |
|
|
A 56-year old man preseents to his physician with symptoms consistent with allergic rhinitis. His PMH is positive for benign prostatic hyperplasia. He continues to work in a warehous as a forklift operator. Which of the follow meds should be used to treat this patient? a) Diphenhydramine b) Hydroxyzine c) Chlorpheniramine d) Fexoenadine |
d) Fexofenadine (2nd gen antihistamines are less sedating and have fewer anticholinergic side effects than first gen. They would be a better choice for someone who operates heavy machinery and has benign prostatic hyperplasia. However, they are no more effective at symptom relief than the first-gen antihistamines) |

