![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
80 Cards in this Set
- Front
- Back
|
ANZCA April 2007 [60] |
ANSWER D
Concerns regarding MOAI 1. sympathetic hyperreactivity 2. ECT results in vagus stimulus followed by overwhelming sympathetic surge Therefore there is a significant risk of hypertensive crisis with MOAIs in ECT J ECT. 2004 Dec;20(4):258-61. Electroconvulsive therapy in patients taking monoamine oxidase inhibitors. -Reviewed the literature, presented 4 new cases and concluded there is no evidence of a dangerous interaction between ECT and MAOI use. In general, a cautious approach would be to discontinue MAOIs before ECT if the medication has not been helpful; however, there is no need for a washout interval before starting ECT. Furthermore, if there is otherwise a reason for continuing the MAOI, it can be continued during index ECT or initiated during maintenance ECT. |
|
|
AZ67 ANZCA version [2003-Apr] Q90, [Jul06] Q47, [Apr07]
The primary duty of an expert witness called by the defence is to the A. Court B. Defence Counsel C. defendent doctor D. medical profession E. patient taking legal action |
ANSWER A
* Be truthful * Be impartial * Must NOT have financial or other interest in the outcome of the case * Must NOT adopt a position of advocacy * Must NOT favour plaintiff or defendant o The ultimate test for accuracy and impartiality is a willingness to prepare testimony that could be presented unchanged for use either by the plaintiff or the defendant |
|
|
AZ02 [Jul07]
Fit and healthy young female for lap. gyne operation, which of the following doesn't require continuous monitoring (See PS 18): A. ECG B. Saturation probe C. Disconnect alarm D. Oxygen analyzer E. Capnography |
ANSWER A
Must be monitored continuously 1. Ventilation : continuously by direct and indirect means : capnography 2. Oxygenation : oximeter 3. Intermittent non-invasive blood pressure monitor 4. Oxygen analyiser with audible alarm to warm of low oxygen concentrations 5. Breathing system disconnection or ventilator failure alarm 6. Volatile anaesthetic agent concentration monitor if using volatile 7. Must be available 1. Electrocardiogram 2. Continuous intra-arterial blood pressure monitor 3. Temperature probe 4. NMB monitoring 5. BIS 6. CVP 7. spirometry 8. TOE |
|
|
AZ03 [Jul07]
The BEST indication of a difficult intubation in morbid obesity: A. Mallampatti Score B. Neck circumference C. Limited neck movement D. TMD E. Body weight |
ANSWER D, neck circumference
From Morbid Obesity and Tracheal Intubation (Anesth Analg 2002) * Factors looked at included: "height, weight, neck circumference, width of mouth opening, sternomental distance, thyromental distance and Mallampati score" * "Logistic regression identified neck circumference as the best single predictor of problematic intubation. Mallampati score inclusion did not further improve the model in our limited study with only 12 problematic intubations. In patients with a large neck, the view during direct laryngoscopy was poorer." |
|
|
04 ANZCA Version[Jul07]
Which of the following statements regarding infection control is FALSE? A. devices to be used in the upper airway that may cause bleeding must remain sterile until used B. provided there is an adequate filter between the patient and the breathing circuit, the circuit can be re-used for subsequent patients on an operating list C. when performing central neural blockade, the anaesthetist must adopt a full aseptic technique D. when performing central venous cannulation, the anaesthetist must adopt a full aseptic technique E. when performing vascular cannulation, the anaesthetist must wash hands and should wear gloves |
ANSWER A
|
|
|
AZ15
Increased alveolar-arterial oxygen gradient can be caused by: A. Endotracheal intubation B. Decreased cardiac output C. Second gas effect D. Atelectasis |
ANSWER D
The two main factors that affect A-a gradient are: * Shunt --> increased A-a gradient * PAO2 - higher PAO2 (due to higher FiO2) results in a high A-a gradient for any shunt The Cardiac output story: decreased CO - decreases mixed venous O2 so shunted blood has lower PaO2, BUT also reduces the shunt fraction, so that the NET effect is no change in A-a gradient |
|
|
AZ18 [Aug95]
Pupillary dilatation may be seen with: A. Metaraminol B. Trimetaphan C. Cardiac asystole D. Stellate ganglion block |
ANSWER D
* A. Metaraminol - maybe true: Metaraminol is a mixed-acting drug but "has relatively stronger direct α1-adrenergic–stimulating effects" (Miller Ch 12). Note that alpha 1 effects are to constrict, so any pupillary dilation will be due to indirect effects acting on beta receptors. * B. Trimethaphan - true: Trimethaphan is a ganglion-blocking drug. "The ganglion-blocking drugs cause a predictable cycloplegia with loss of accommodation because the ciliary muscle receives innervation primarily from the parasympathetic nervous system. The effect on the pupil is not so easily predicted, since the iris receives both sympathetic innervation (mediating pupillary dilation) and parasympathetic innervation (mediating pupillary constriction). Ganglionic blockade often causes moderate dilation of the pupil because parasympathetic tone usually dominates this tissue." (Katzung, Basic and Clinical Pharmacology, 11E, Chapter 8, Cholinoceptor-Blocking Drugs) * C. Cardiac asystole - maybe true: cardiac asystole per se should not cause dilated pupils. However, presumably a sympathetic response to the asystole will cause pupillary dilation, as will brain death secondary to asystole. * D. Stellate ganglion block - false: Horner's syndrome: meiosis, ptosis, enophthalmos, anhidrosis |
|
|
AZ19 [Aug92]
Pressure inside the GIT is increased by: A. Nitrous oxide B. Suxamethonium C. Neostigmine D. T6 epidural |
All true:
* A. diffusion, * B. increased intragastric pressure, * C. augment vagal tone, * D. antagonise SNS so increased vagal effects |
|
|
AZ21 ANZCA version [2002-Mar] Q120, [2002-Aug] Q146 (Similar question reported in [1987] [1988] [Aug92] [Apr96] [Aug96] [Apr97] [Jul97] [Jul98] [Apr99] [Aug99] [Jul00])
In an adult with advanced ankylosing spondylitis 1. surgery near the elbow could be done most safely under successful interscalene brachial plexus block 2. there is decreased lung compliance 3. maintenance of the airway during general anaesthesia using a face mask is frequently difficult 4. cardiovascular assessment should be thorough because of the known association with aortic insufficiency |
ANSWER 2 and 4
Ankylosing spondylitis is a type of seronegative arthropathy. Implicatications for anaesthesia: * Pulmonary fibrosis hence potential hypoxia * Aortic root pathology particularly AR 1 - incorrect. Interscalene blocks can cause loss of diaphragmatic tone, hence would be contraindicated in patients with respiratory complications. 2 - correct. Pulmonary fibrosis leads to decreased lung compliance 3 - incorrect. Ank. spond does not lead to difficulty with face mask application 4 - correct. Watch for AR. |
|
|
AZ22
Lignocaine spray to the cords reduces laryngospasm by: A. Blocking parasympathetic afferent receptors B. Paralysing the smooth muscle C. Blocks the sympathetic response D. ? |
ANSWER A
The glottic closure reflex is another protective airway reflex.5 It can be elicited by selective stimulation of the superior laryngeal nerve (CNX branch), but has been reported to be triggered by stimulation of any cranial nerve in experimental animals. The efferent arc encompasses the superior as well as the recurrent laryngeal nerve. Exaggeration of the glottic closure reflex, called laryngospasm, may be noted after prolonged or intense stimulation of the glottis and is initiated solely by stimulation of the superior laryngeal nerve. |
|
|
AZ27 [Mar94]
Lowest venous oxygen saturation during anaesthesia occurs in blood from: A. Liver B. Brain C. Heart D. Lung E. Kidney |
ANSWER C
Heart |
|
|
AZ23 ANZCA version [2001-Apr] Q120 (Similar question reported in [1986] [Mar90] [Aug95] [Apr96])
In the management of a 65 year old man who requires thoracotomy for a mediastinal tumour previously treated with large doses of bleomycin 1. a chest x-ray is essential to exclude pulmonary fibrosis 2. oxygen therapy should be given by face mask soon after narcotic premedication 3. impairment of renal function is common 4. surgery should be delayed for 48 hours after lymphangiography |
ANSWER
Bleomycin * used Testicular Ca,and squamous head and neck tumours, lymphomas * Can be used iv/sc/im, * little myelosuppression * Cleared renaly and you have increased complications if preexisting renal failure * Can be inactivated by bleomycin hydrolase [edit] Complications of bleomycin * allegic reactions common * raynauds, * mucocutaneous reactions eg alopecia, hyperpigmentation common * Toxicity dose usually more than a total of 300-400 units . [edit] pulmonary fibrosis * 5-10 % * usually lower lobes * Risks factors include o total bleomycin dose; o renal failure (it is renally excreted); o concurrent radiotherapy or other chemo; o age > 70. o possibly excessive crystalloid admin o possibly high FIO2 |
|
|
AZ29 ANZCA version [2001-Aug] Q26, [2002-Mar] Q39 (Similar question reported in [Sep90] [Aug91] [Mar92] [Aug92] [Apr96] [Aug96] [Apr97])
When using low-flow circle absorber techniques, the uptake of nitrous oxide must be considered. In a healthy 70 kg adult the expected uptake of nitrous oxide, with a 70% inspired concentration, after 1.5 hours would be about A. 1000 ml.min-1 B. 500 ml.min-1 C. 250 ml.min-1 D. 100 ml.min-1 E. <50 ml.min-1 |
ANSWER D
uptake of N2O (in mls/min) is equal to 1000 divided by the square root of the time elapsed (in mins) * the time elapsed is 100 minutes. * the square root of this is 10 * 1000 divided by 10 is 100 so the N2O uptake at 100 mins into the case would be about 100mls/min. |
|
|
AZ30 [Mar91] [Aug91] [Apr97]
In a lightly anaesthetised patient who is apnoeic, the rise in pCO2 per minute is: A. 0.5 mmHg B. 1 mmHg C. 2 mmHg D. 3 mmHg E. 5 mmHg |
ANSWER D
D is best answer Rise in PaCO2 is 3-6mmHg/min (Nunn p238) Higher rate of rise early on then 3mmHg/min |
|
|
AZ35 [Mar92] [Apr97] [Jul97] [Aug99]
For a difficult intubation using a gum elastic bougie - to achieve the least resistance to entry of ETT: A. Leave laryngoscope as is & do a 1/4 turn clockwise with the ETT B. Leave laryngoscope as is & do a 1/4 turn anticlockwise C. Take laryngoscope out & do a 1/4 turn clockwise D. Take laryngoscope out & do a 1/4 turn anticlockwise |
ANSWER B
|
|
|
AZ38 [Mar93] [Aug93] [Apr98] [Jul98]
CPAP during spon resps: A. Increased insp. capacity B. IIncreased vital capacity C. Increased closing volume D. Increased (FRC-CV) difference |
ANSWER D
CPAP * ↑ FRC * ↓ extravascular lung water * ↓ CV ∴ if ↑ FRC and ↓ CV → ↑ FRC-CC |
|
|
AZ37 [Mar93] [Aug93]
Lightly anaesthetized patient in the lithotomy position (?spontaneously breathing): 1. Marked reduction in vital capacity 2. Increased FRC 3. Normal alveolar ventilation 4. Residual volume & closing volume equal 5. Decreased A-P diameter of thorax |
ANSWER 4
1. FALSE : no change to VC 2. FALSE : decrease in FRC 3. FALSE : decreased alveolar ventilation 4. TRUE : CV approaches FRC 5. FALSE : there is decreased crossectional area, but no change anterioly or caudad |
|
|
AZ39 [Aug93] [Mar94]
The major anabolic hormone in response to surgery is: A. Thyroxine B. Human growth hormone C. Cortisol D. Insulin E. Glucagon |
ANSWER B
Catecholamines, corticosteroids, GH, glucagon all increased. GH only anabolic hormone. TSH unchanged. Thyroxine may be increased by symathetic stimulation, but catabolic effects. |
|
|
AZ40 [Aug93]
A fit healthy 70kg adult has a laparotomy & a morphine infusion is ordered postoperatively. After a loading dose of ..(.?.)... mg/kg. what infusion rate would you order? A. 200 mcg/hr B. 500 mcg/hr C. 2000 mcg/hr D. 5000 mcg/hr |
ANSWER C
Acute pain management guidelines: 10-40mcg/kg/hr --> 2mg/h seems good. |
|
|
AZ41 [Aug93] [Mar94]
Scleroderma: A. Nasal intubation is contraindicated B. Sensitive to non-depolarising muscle relaxants C. Pulmonary involvement is only associated with severe systemic disease D. ? E. Gaseous induction is contra-indicated (Related Q MZ32) |
ANSWER ??D
Nasal intubation is RELATIVELY contraindicated because of the risk of bleeding from telangiectasia but may be required because of difficult upper airway/neck anatomy. Gas induction is similarly RELATIVELY contraindicated because of the risk of aspiration Introduction * Onset 20-40 years * Characteristics of autoimmune and collagen disease * Do NOT give corticosteroids * Can progress to CREST syndrome Signs and symptoms * Skin and musculoskeletal o Thickening o Increased CK from myopathy o Arthritis * Neuro o Perpipheral or Cranial neuropathy o Trigeminal neuralgia * CVS o Sclerosis coronary arteries o Replacement of cardiac muscle with fibrosis o Arrhythmias o CCF o pulmonary HT o Pericarditis o Oral or nasal telangectasias o Raynauds * Lungs o Diffuse interstitial fibrosis so decreased IC and increased RV o Decreased lung compliance due to fibrosis o Decreased diffusion capacity * Renal o Decreased RBF o Accelerated systemic HT and renal failure most common cause of death * GIT o Xerostomia (dry oral mucosa) o Dysphagia common o Decreased LOS tone so increased risk of reflux Anaesthesia * Decreased mouth opening due to tight skin * Telangectasias may bleed profusely * IV access difficult * Can be difficult getting a pulse oximeter reading from the fingers * Vasomotor instability - minimised by keeping patient warm * Increased risk of aspiration/reflux * Decreased pulmonary compliance so may need high airway pressures * Supplemental O2 needed because of poor diffusion capacity |
|
|
AZ42 ANZCA version [2001-Aug] Q1 (Similar question reported in [Aug93] [Apr96])
Carotid endarterectomy for symptomatic carotid disease A. has a peri-operative stroke rate of 8 to 10% B. should be performed under regional anaesthesia in patients with ischaemic heart disease to reduce the incidence of myocardial infarction C. may be performed under induced hypotension to reduce intraoperative blood loss D. when performed under deep cervical plexus block is often associated with a phrenic nerve palsy E. should be performed under regional anaesthesia in patients with a recent transient ischaemic attack to reduce the incidence of peri-operative stroke |
ANSWER
A. FALSE : 6.5% if symptomatic, 2.3% if assymptomatic B. FALSE : no evidence C. FALSE : BP should be normal to high to reduce cerebral ischemia D. TRUE E. FALSE : no evidence that regional reduces ischemic events (GALA trial no difference between primary outcomes for GA vs LA) |
|
|
AZ44b ANZCA version [2002-Mar] Q29, [2002-Aug] Q1 (A-type but only 4 options) (Similar question reported in [Jul00])
According to current legal recommendations in Australia regarding the obtaining of consent for anaesthesia A. it is reasonable to withhold risk information from the very anxious patient B. it is adequate to use the standard of risk disclosure set by a responsible body of medical opinion C. only risks which would be considered significant by a reasonable person need to be discussed D. significant risks with a likelihood of less than 1% may need to be discussed |
ANSWER D
A. FALSE B. FALSE : Bolam principle superceded by principles of Rogers v Whitaker. C. FALSE : Whitaker case D. TRUE : Whitaker case Even if an extremely unlikely risk is of concern to the patient it does need to be discussed. Roger's vs Whitaker : Duty of Disclosure -Whitaker was almost total blind in right eye since 9yo, but lives a normal life -Roger's, opthalmic surgeon, advised her that an operation on the injured eye would not only improve its appearance but would probably restore sight to it -Whitaker developed 'sympathetic ophthalmia' in her left eye with no improvement in her right and therefore was totally blind -Rogers defence was the "Bolan" principle, that a medical practitioner is not negligent if he acts in accordance with a practice accepted at the time as proper by his peers, even though other medical practitioners adopt a different practice. However, High Court Decision : -all medical treatment is preceded by the patient's choice to undergo it. -The choice is meaningless unless it is made on the basis of relevant information and advise. -description of risks should be tailored in the proposed risk, and the patient -a reasonable person in the patient's position, if warned of the risk, would be likely to attach significance to it |
|
|
AZ45 [Mar93] [Aug94] [Apr97] [Apr99]
In a patient who is to receive a renal transplant: A. Suxamethonium is contraindicated if the patient is anephric B. Hypotension should be treated with phenylephrine or methoxamine C. Regional anaesthesia is contraindicated D. CVP is an inappropriate guide to fluid replacement E. Hypotension should be treated with dopamine |
ANSWER E
Promote renal perfusion by (a combination of...) * decreasing anaesthesia depth * maintaining high normal SBP * giving crystalloids * dopamine IV (3ug/kg/min) |
|
|
AZ46 [Mar95] [Aug96] [Apr97] [Jul97]
Ambulatory surgery: (type K) A. ASA 3 patients have three times the risk of postop admission as compared to ASA 1 or 2 B. ASA 1 & 2 patients aged >60 have three times the risk of postop admission as compared to age <60 yrs C. Not suitable for the morbidly obese D. Not suitable for patients with a history of malignant hyperthermia |
All are false. – risk factors for admission are age > 85, comorbidity, hospitalisation within previous 6 months.
Miller (pg2592-3) answers this question nicely: A - False (not difference with ASA status) B - False (not age difference) C - Best answer ("morbid obesity complicated by symptomatic cardiovascular or respiratory problems is contraindication to outpatient surgery") D - False (trigger-free anaesthesia & observe for 4 hrs) - |
|
|
AZ49 ANZCA version [2002-Aug] Q66, [2003-Apr] Q71 (Similar question reported in [Aug96] [Apr98] [Jul98])
A patient taking cyclosporine after renal transplantation is UNLIKLELY to have A. Macrocytic anaemia B. Interstitial renal fibrosis C. Hypertension D. Peripheral neuropathy E. Suppresion of humoral immunity |
ANSWER A
Cyclosporin -DMARDS (disease modifying anti-rheumatic drugs) -immunosuppressive -used to treat RA, SLE, polymyositis, rejection of transplant Genitourinary -renal dysfunction (common 30%) -glomerular capilliary thrombosis Cardiovascular -hypertension (50%) -IHD Skin -Acne -Hirsutism CNS -tremor (common 20%) -convulsion -headache -somnolence GIT -gum hyperplasia (common 15%) -diarrhoea -nausea vomiting (common 10%) -hepatotoxity (common 50% of patients have elevated bilirubin, tramaminases, alk phos) -gynecomastia CNS -distal plaresthesia -Flushing Blood -leukopenia -lymphoma (infectious complications include : sepsis, abscess, systemic fungal infection CMV) Resp -sinusitis |
|
|
AZ50 [Aug96] [Apr97] [Jul97] [Apr99]
ANZCA guidelines for care of patients recovering from anaesthesia in the recovery area: A. Recovery bed must be tiltable from one end but not both (OR: Tilt head down but not head up) B. Ratio of registered nurses to patients must provide no less than one nurse to two patients, and one to any patient who remains unconscious C. Each bed space must be provided with a means of inflating the lungs with oxygen in a ratio of one per bed D. Recording of postop observations including SaO2 & temperature |
ANSWER D
* Observations should be recorded at appropriate intervals and should include state of consciousness, oxygen saturation, respiratory rate, pulse rate, blood pressure and temperature. * Bed must tilt from one or both ends both head up and head down at least 15 degrees * The ratio of registered nurses to patients needs to be flexible so as to provide no less than one nurse to three patients, and one nurse to each patient who has not recovered protective reflexes or consciousness. * Must be means for manual ventilation with oxygen in a ratio of one unit per two bed spaces, but with a minimum of two such devices |
|
|
AZ51 ANZCA version [2001-Apr] Q33, [2003-Apr] Q21, [2003-Aug] Q46 (A-type with only 4 options) [2006-Mar] Q110-similar question but with 5 options
During anaesthesia for Magnetic Resonance Imaging, A. any ferromagnetic items outside the 30 Gauss line will not be strongly attracted to the magnetic core B. any battery-powered monitor of non-ferromagnetic construction can be safely placed close to the magnetic core without risk of attraction to the magnet C. the most commonly used MRI contrast medium, gadopentetate dimeglumide (Magnevist) induces a similar incidence of side effects as does the iodinated contrast media used in radiology D. it is essential to limit the use of halogenated agents as halogen atoms exhibit the property of nuclear magnetic resonance and may interfere with image quality E. permanent pacemakers can only be permitted if they have been completely disabled prior to the MRI (2006 March paper) |
ANSWER A
A. TRUE : Ferromagnetic items must be kept outside the 30-50 Gauss lines5 or, ideally, excluded from the MRI suite. B. FALSE : most batteries are ferromagnetic in construct, even though the monitor maybe non ferromagnetic C. FALSE : The most common agent, dimeglumine gadopentetate (Magnevist, Schering Pty Ltd), has a high therapeutic index compared to iodinated agents. D. FALSE E. FALSE : The risks of scanning patients with permanent pacemakers or ICDs are related to possible movement of the device, programming changes, asynchronous pacing, activation of tachyarrhythmia therapies, inhibition of pacing output, and induced currents in lead wires leading to heating and/or cardiac stimulation. Despite reports that some patients with pacemakers or ICDs have been scanned safely, the presence of a pacemaker or ICD is still considered a strong relative contraindication to routine MR examination. |
|
|
AZ52 [Aug96] [Apr98] [Jul98] [Jul00] (type A)
In MRI scan, which will NOT cause patient burns: A. Thermistor temperature probe B. Non-metallic face makeup C. Coiled monitor leads on patient chest in magnetic core D. Non-ferromagnetic equipment touching patient E. Pulsating magnetic field |
ANSWER B
|
|
|
MRI notes
|
Overview
The 3 particular aspects of MRI affecting anaesthesia are: * need for the subject to lie still during the scan * the effects of the magnetic field (eg need for special monitoring modifications) * location outside OT The 2 indications for anaesthetic involvement are: * to provide immobility (eg children, uncooperative adults) * very sick patients requiring intensive monitoring About 3% of adults cannot tolerate MRI without anesthesia Duration A typical scan sequence lasts 15 to 25 minutes, although complex procedures may up to two hours. Generic list of hazards * from magnetic field * from precautions for field * hard to see or get to patient in tunnel * from remote location * from associated conditions * hypothermia in small children Issues with magnetic field Basic physics * most are 0.5-1.5 Tesla (T). POWH, Randwick, has a 3T MRI Scanner o 1 gauss= Earth's Magnetic Field o 1T = 10,000 gauss o gauss = 0.1milliT ie 5 gauss = 0.5mT * magnetic field decreases with distance problems to do with magnetic field * Hazards from magnetic field * Precautions to avoid hazards * Interference with magnetic field/signals from other equipment Hazards from magnetic field movement of ferromagnetic objects * projectiles (eg needles, laryngoscope, scissors) * movement of implants (eg aneurysm clips leading to intracranial haemorrhage; implanted heart valves -usually OK; cardiac stents areoften ferrous - wait 8/52 for them to be stuck down; endoluminal AAA - some kits have ferrous material in iliac sleeves/"legs"; foreign body in eye can lead to vitreoretinal haemorrhage) hearing * rapidly changing magnetic field leads to VERY loud 65-95dB knocking noises burns * magnetic field leads to eddy currents in electrical devices eg ecg electrodes - need carbon fibre ones * burns have been reported with: o standard ECG o standard SpO2 - (In one case, so so severe that patient lost a finger) o temperature monitoring * large metallic prosthesis will get localised heating but clinical impression is that thermal fx are mild and tolerable * electrical equipment tends to malfunction near magnetic field ECG * distorted so much it is usually useless * magnetic storage media will be erased (eg Credit cards, floppy discs) All staff, patients or relatives have to fill out questionaire to detect potential problems issues due to precautions due to magnetic field * see also positioning * long tubing o outside scan room set at 0.5mT boundary o gas analysis response time inc by 5-10sec * can't use invasive pressure monitoring * unfamiliar equipment * can’t resuscitate patient while in the scanner interference with the test * magnetic field + quality of images can be messed with by radiofrequency waves from: o large nearby ferromagnetic objects o even small amounts of ferrous materials within 3D space to be scanned * so decreasing quality of images may be non-diagnostic * scan room shielded from outside electrical equipment * electrical equipment inside scan room needs to similarly shielded associated conditions -syndromic kids - watch for airways & CVS changes remote location * generic probs o of consideration to anesth needs in design (eg pipeline gases, suction, waste gas exhaust capabilities) o lack of trained personnel to assist in emergency IV contrast media for MRI * Paramagnetic * May not contain iodine * Gadolinium is the common ingredient * High therapeutic ratio * Side effects: o Headache o Nausea & vomiting o Local burning o Weals 2.5% * Anaphylaxis 1/100 000 Common agents * Gadopentate o Magnevist o 0.2-0.4ml/kg * Gadodiamine o Omniscan o 0.2ml/kg * gadoversetamide o Optimark Positioning issues and monitoring * equipment positioning * ear protection Two approaches to anaes equipment and magnetic field * Use specialised MRI compatible equipment within scan room * Use conventional equipment located outside field in control room Standardising on one option keeps anaesthetist and equipment together ie you either do one or the other Factors in decision * funds * space * expected frequency of GAs * individual preference Conventional outside approach advantages: * allows faulty monitors to be changed * cheaper * less crowding in scan room * can apply simply rule: Nothing enters scan room except patient and trolley typical set up * induction area adjacent to but outside scan room 0.5mT boundary * compact conventional anaes machine/monitoring in induction room * non magnetic tipping trolley * compact eg wall mounted conventional anaes machine in ctl room with 10m coaxial/bain syestem * MRI-compatible saturation probe fibreoptic pt probe shielded cable * extended gas sampling line (slows response time by 5-10 sec) * MRI compatible ECG – carbon fibre leads and electrodes * NIBP machine with extended hose, non-metallic connectors, range of cuffs * ECG: carbon fibre leads and electrodes Airway 3 issues/points: * decreased access * options available * practical issues Access limited so low threshold for intubation relative categories/options:3 -<2/12 will often sleep through short scan if fed wrapped up placed on side in scanner -ETT indications *suspect increased ICP *suspect Space occupying lesion head * kids <15kg *aspiration risk * LMA /sv ok if older kids or adults without above risks sedation * adults where anxiety main issue * back pain where ++ analgesia required to tolerate lying still * some centres have protocol for kids - questionable risk:benefit equipment/practical issues * RAE good cos keeps connectors/filters out of head ring * tape pilot balloon to something eg filter * cuffed tube handy – see below Ventilation issues with long tubing * if long tubing, use circuit that decreased dead space eg **bain **T piece *these systems tend to have expir resistance that leads to some PEEP, especially at higher FGF * PPV tidal volumes [=Vt] tend to be lower due to **expans'n of tubing **"compression losses " within tubing * cos Vt's tend to be lower to start with, leak around an uncuffed ETT not as well tolerated - consider going a size up or using cuffed ETT * simple Pressure generating ventilators may not cut the mustard * P's measured at anaesthetic machine end don't accurately reflect P's at pt end of tubing If patient arrests in scan room * Don't do ACLS in scan room * Don't allow arrest team into scan room * BLS in scan room: o external cardiac compression o non metallic bag/mask ventilation * transfer out using non metallic trolley Contraindications Absolute * Cardiac pacmakers * ICD * Metal in the orbit * Metal in the CNS (some modern aneurysm clips are not ferromagnetic) * ferromagnetic stapedial implants Relative * Other electronic implants o spinal stimulators o insulin pumps o lead wires * prosthetic heart valves * cochlear implants * Metal in other parts of body (joint replacements and secure plates are OK) * Tattoos |
|
|
AZ53 [Apr97] [Apr98] (type A)
According to ANZCA policy documents which of the following emergency drugs does NOT need to be available where minor sedation is carried out: A. Lignocaine B. Atropine C. Adrenaline D. 50% dextrose E. Calcium chloride |
ANSWER E
Emergency drugs should include at least the following: 1. adrenaline 2. atropine 3. dextrose 50% 4. lignocaine 5. naloxone 6. flumazenil 7. portable emergency O2 supply |
|
|
AZ55 [Apr98] (type A)
Cricoid pressure applied at 40 Newtons would: A. Halve the lower oesophageal sphincter (LOS) pressure B. Double the LOS pressure C. No effect on LOS pressure/tone D. Resist a gastric pressure of 40 mmHg. E. Resist a gastric pressure of 80 mmHg. |
ANSWER ?A ?D
40N resists 38mmHg and 40mmHg OESOPHAGEAL pressure depending on study. Halves LOS tone from 24 to 12. |
|
|
AZ55b ANZCA version [2005-Apr] Q79
Application of cricoid pressure with a force of 40 newtons will resist reflux with an intra-oesophageal pressure of A. 30 mmHg B. 40 mmHg C. 50 mmHg D. 60 mmHg E. 70 mmHg |
ANSWER B
40N resists 38mmHg and 40mmHg OESOPHAGEAL pressure depending on study. Halves LOS tone from 24 to 12. |
|
|
AZ56 ANZCA version [2001-Apr] Q53, [2001-Aug] Q40, [2002-Aug] Q32, [2003-Aug] Q67, [2005-Apr] Q72, [2005-Sep] Q82, [Apr07] Q67(Similar question reported in [Jul98])
A patient with severe liver disease is scheduled to have a portacaval shunt for portal hypertension. Recommended features of the anaesthetic management include A. use of vecuronium as the relaxant of choice B. care with the dose of suxamethonium because it may have a prolonged effect C. avoidance of fentanyl as an analgesic D. avoidance of all volatile anaesthetic agents including isoflurane E. reduction of the induction dose of thiopentone |
ANSWER E
A. FALSE : cis-atracurium is the drugs of choice B. FALSE The metabolism of succinylcholine may be slowed because of reduced pseudocholinesterase concentrations, but in practice this gives few problems C. FALSE D. FALSE E. TRUE : The dose of thiopental should be reduced because a reduction in plasma proteins results in an increased unbound fraction of drug; the distribution half-life and consequently the duration of action are also prolonged |
|
|
AZ59 ANZCA version [2001-Apr] Q111 (Similar question reported in [Mar00])
The lower oesophageal sphincter 1. has both longitudinal and circumferential fibres 2. is supplied by both sympathetic and parasympathetic nerves 3. exerts a pressure in excess of 30 cmH2O 4. does not usually extend above the diaphragm in normal individuals |
1, 2, 3 true, 4 false,
|
|
|
AZ60 [Mar00] [Jul00]
Young male with a ruptured right main bronchus and fractured 1st & 2nd ribs with blood from external auditory meatus. (?Past history of narcotic addiction.) Components of induction include: (OR: Appropriate anaesthetic: ) A. Awake nasal intubation after topicalisation B. Awake fibreoptic orally using topical lignocaine (? & DLT) C. ? D. Left double lumen tube & use scope to check position (Similar to AT19) (see also IC15b) |
ANSWER ?B
OPTIONS - Awake surgical trache if no laryngeal damage - AFOI if tolerated, with DLT - still is risk of obstruction - Inhalational induction, keep spont breathing, DLT (risk of obst esp with relaxant) In all cases have ENT scrubbed in theatre ready to do emergency cricothyroidotomy/trache Also obviously do all this in OR NOT in ED Locate cricothyoid membrane before induction/AFOI so can do emergency cricothyoidotomy |
|
|
AZ61 ANZCA version [2001-Apr] Q116 (Similar question reported in [Jul00])
Methods to potentiate electroconvulsive therapeutic seizures include 1. hyperoxygenation 2. administration of adenosine antagonists 3. ensuring good electrode scalp coupling 4. unilateral electrode placement |
1, 2, 3 true, 4 false
Increase seizure duration: *Hyperoxia *hypocapnia *ketamine *alfentanil/remi (by reducing anaes agent dose) *caffeine *ensure good coupling Decrease seizure duration: Opposite of above + *methohexital/thio/diazepam/propofol/esmolol |
|
|
AZ62 ANZCA version [2001-Aug] Q63, [2002-Mar] Q58
A 91 year old farmer presents for anaesthesia for a total hip replacement. He gives a history of failed endotracheal intubation with his last two anaesthetics, probably due to arthritis of the cervical spine. The rest of the history and examination is unremarkable. His American Society of Anesthesiologists Physical Status Score (ASA Status) is A. ASA 1 B. ASA 2 C. ASA 3 D. ASA 4 E. ASA 5 |
ANSWER B
ASA I: * patient's health: excellent with no systemic disease * limitations on activity: none * danger of death: none * excluded: persons at extremes of age (very young very old) ASA II: * patient's health: disease of one body system * status of underlying disease: well-controlled * limitations on activity: none * danger of death: none ASA III: * patient's health: disease of more than one body system or one major system * status of underlying disease: controlled * limitations on activity: present but not incapacitated * danger of death: no immediate danger ASA IV: * patient's health: poor with at least one severe disease * status of underlying disease: poorly controlled or end-stage * limitations on activity: incapacitated * danger of death: possible ASA V: * patient's health: very poor moribund * limitations on activity: incapacitated * danger of death: imminent ASA VI: * brain-dead patient undergoing organ harvest |
|
|
AZ63 ANZCA version [2002-Aug] Q123, [Mar06] Q59 [Apr07] Q10
Regarding extracorporeal shockwave lithotripsy (ESWL) for renal calculi in patients with a permanent pacemaker in situ, A. ESWL is contraindicated B. ESWL pulses should be timed to coincide with the ST interval C. rate modulation of the pacemaker should be deactivated during the ESWL procedure D. there is a risk that the ESWL pulse will reprogramme the pacemaker E. regional anaesthesia is relatively contraindicated |
ANSWER C
Lithotripsy may be used in patients with a pacemaker insitu, but the lithotriptor must be kept at least 6 inches away from the pacemaker. The lithotripsy pulses should be timed with the ECG and rate-modulation should be de-activated |
|
|
AZ64 ANZCA version [2002-Aug] Q90, [2003-Aug] Q50, [2005-Apr] Q23, [2005-Sep] Q13
The Mallampati classification of the airway using the view of the faucial pillars, the soft palate and the uvula obtained with the tongue protruding, is A. validated in both children and adults B. associated with a high false positive rate for difficult laryngoscopy C. not applicable to edentulous patients D. useful for choosing the size of endotracheal tube E. associated with a positive predictive value of approximately 90% |
ANSWER C
For predicting difficult tracheal intubation, the original Mallampati test had very poor accuracy. Four of the five studies had sensitivities <50%. Small increases in sensitivity led to large sacrifices in specificity. From Cattano's figures rounded out: true -ve (MP<3, easy tube) 1700. false +ve ( MP>=3, easy tube) 180 false -ve (MP<3, hard tube) 30. true +ve (MP>=3, hard tube) 15 Sensitivity (good sens has low false neg) = TP/(TP+FN) = 15/(15+30) = 30% Specificity (good spec has low false pos) = TN/(TN+FP) = 1700/(1700+180) = 90% PPV = TP/(TP+FP) = 15/(15+180) = <10% NPV = TN/(TN+FN) = 1700/(1700+30) =>98% |
|
|
AZ65a ANZCA version [2001-Apr] Q54, [2001-Aug] Q48, [2002-Aug] Q87, [2003-Apr] Q50
For personnel working in an operating room environment A. levels of volatile anaesthetic agents of less than 5 parts per million are considered safe B. chronic exposure to trace levels of anaesthetic agents causes significant cognitive impairment C. the risk of abnormal pregnancy is higher than that of smokers D. the risk of cancer is increased in males E. none of the above |
ANSWER E
A. FALSE : Recommended maximum concentrations in operating theatre (National Occupational Health and Safety Comission, Australia) • 25 ppm for nitrous oxide • 0.5 ppm for volatile agents when nitrous oxide is used, 2 ppm when it is not B. FALSE: The NIOSH recommendations arose from a study by Bruce and Bach in which healthy volunteers in the laboratory suffered a decrease in psychomotor performance when exposed to concentrations of nitrous oxide as low as 50 ppm, alone or in combination with 1 ppm of halothane. The same study showed that 25 ppm of nitrous oxide combined with 0.5 ppm of halothane had no effect. C. FALSE : This preliminary report showed the incidence of infertility, spontaneous abortion and children with congenital abnormalities in female anesthesiologists to be the same as that in other physicians D. FALSE : the prevalence of abortion was substantially higher in female anesthesiologists than in female physicians working outside the operating room. Studies in this era also concluded that the incidence of congenital anomalies in children of male and female anesthesiologists was higher than in the control groups of physicians. In addition to these reproductive effects, meta-analysis of six of these early studies linked the exposure to anesthetic gases to hepatic disease in males[10] and cervical cancer, liver disease, and kidney disease in females. E. TRUE |
|
|
AZ66 ANZCA version [2003-Apr] Q124
The bibliographic database of LEAST relevance to anaesthetists is A. CINAHL B. Cochrane Library C. Embase D. Medline E. PsycINFO |
ANSWER E
* Psycinfo is specific for psychology. * Embase is an alternative to medline-it is relevant in that to FULLY search the literature you should search medline and embase- any decent meta-analysis will do this as some journals will not be referenced in both - contains many european & foreign language journals(although Medline is more than enough for our MCQ answering it includes BJA,CJA, A and A etc.) * Cochrane is a database of sytematic reviews and there are many others EBM etc. * CINAHL is a database of journals relevant to nursing; it has major anaesthesia journals such as Anesthesiology so should be useful. |
|
|
AZ70 ANZCA version [2003-Apr] Q102, [2004-Apr] Q57, [2004-Aug] Q64
Acute cannabis use just prior to surgery is most likely to A. cause intra-operative bradycardia B. decrease anaesthetic requirements C. increase the incidence of peri-operative nausea D. increase the risk of infra-operative awareness E. reduce the reliability of a BIS (bispectral index) monitor |
ANSWER B
acute cannabis use have decreased anaesthetic requirement(doesn't stimulate the sym system) Amphetamines & Cocaine (stimulate the SYM system) - increase req on acute use only |
|
|
AZ71 ANZCA version [2003-Apr] Q99
The most common reason for patients complaining about their medical treatment is A. charging of excessive fees B. patient's predisposition to com plain C. poor communication with medical staff D. poor outcome of medical treatment E. poor physical environment |
ANSWER C
|
|
|
AZ72 ANZCA version [2003-Apr] Q121 [Mar10]
The American Society of Anaesthetists (ASA) Physical Status Classification rating system was designed for categorising A. intra-operative adverse anaesthetic event risk based on physical status B. intra-operative adverse surgical event risk based on physical status C. physical status in a standardised manner D. peri-operative adverse anaesthetic event risk based on physical status E. peri-operative adverse surgical event risk based on physical status |
ANSWER C
ASA classification was always meant to globally assess the degree of "sickness" or "physical state" prior to selecting the anesthetic or prior to performing surgery. It is not an measure of risk. |
|
|
AZ73 ANZCA version [2004-Apr] Q127, [2005-Apr] Q52, [2005-Sep] Q7 [2009-Aug]q76
A fourteen-year-old girl is scheduled to have a termination of pregnancy. With regard to consent for this procedure, which of the following statements most truly reflects the law in Australasia? A. A fourteen-year-old girl is able to give consent independently of her parents/guardians if she is considered, by her treating doctors, to be of sufficient maturity to understand the issues. B. A fourteen-year-old girl is able to give consent independently of her parents/guardians only if a court deems her sufficiently mature. C. Minors are not able to give consent, independently of parents/guardians, until sixteen years of age. D. Minors are not able to give consent, independently of parents/guardians, until eighteen years of age. E. Only life-saving treatment may be administered to a fourteen-year-old without parental/ guardian consent. |
ANSWER A
This is a test of Gillick competence. The relevant common law discussion is outlined here[1] (http://www.lawlink.nsw.gov.au/lrc.nsf/pages/ip24chp02) at the NSW Law reform commission site. (All following quotes from this site.) Note that the initial Gillick decision was made in regard to contraception: "In Gillick, it was held that a young girl was competent to consent to contraceptive advice and treatment if she had a sufficient understanding and intelligence to enable her to understand fully what was proposed" Privacy: If you are 12 years or over you can see your doctor/health carer without your parents being present and your doctor is not allowed to give out information about you without your permission. Your health carer must keep what you say to them confidential unless: • You told them you were going to seriously harm or kill yourself • You were thinking about injuring/harming someone else • Someone else is physically harming you or sexually abusing you. Contraception and abortion: • If you are 16 years or more you can give your own consent to the doctor for contraception. • If you are 14 years, and the doctor believes you can give informed consent, then they are able to prescribe contraception or perform an abortion without the permission of the parent or guardian. • If you are under 14 years, the health carer must establish that you are able to give informed consent and some health workers may want to ask your parent/s’ permission. If this is a problem for you contact a youth health service or try another health worker. If you are capable of making an informed decision, then your doctor must listen to you if you have not given your consent. Medicare: • At fifteen you can obtain your own Medicare card, and your parents will not be told. The Gillick-competence test A young person under 18 years of age is legally competent to consent to medical treatment if he or she is capable of understanding the nature and consequences of that treatment. The High Court of Australia settled this common law test for determining a young person’s competence in a case commonly known as Marion’s case. The majority of the Court held that: A minor is capable of giving informed consent when he or she achieves a sufficient understanding and intelligence to enable him or her to understand fully what is proposed. The majority in Marion’s case followed a decision of the English House of Lords in Gillick v West Norfolk and Wisbech Area Health Authority.11 In Gillick, it was held that a young girl was competent to consent to contraceptive advice and treatment if she had a sufficient understanding and intelligence to enable her to understand fully what was proposed. The test focuses on an assessment of the individual young person’s level of maturity and understanding in relation to the treatment proposed. This means that, before the age of 18 (when a young person legally becomes an adult), there is no fixed age at which it is possible to say, in advance of such an assessment, that a young person is automatically capable of consenting to medical treatment generally, or to specific types of medical treatment. Thus, while a young person of, say, 10 years of age may have the necessary intelligence and understanding of what is proposed to consent to the administration of a course of antibiotics to treat a sore throat, he or she may not, at the same time, possess sufficient understanding to consent to the removal of his or her tonsils in the case of acute tonsillitis. In short, before the age of majority, competence to consent operates on a continuum which ranges from the point at which a young person is clearly able to consent to the medical treatment proposed to that at which he or she is clearly unable to do so. The test may prove difficult for medical practitioners, with whom the assessment of Gillick-competence initially rests, to apply in practice. The imprecision of the test places a significant onus on that assessment. Medical practitioners sued for providing medical treatment to a young person without consent bear the onus of proving that they believed that the young person was of sufficient maturity and understanding to consent to the treatment in question. |
|
|
AZ74 ANZCA version [2004-Apr] Q123, [2004-Aug] Q63, [Mar06] Q51, [Jul07]
Intubation of patients with acute C5 spinal cord injury A. can only be safely performed using awake fibreoptic intubation B. is necessary in most patients for secretion clearance C. is necessary in most patients to avoid atelectasis D. is associated with a low risk of aspiration E. may be safely facilitated by the use of suxamethonium |
ANSWER E
A. FALSE : Options include (i) direct laryngoscopy and intubation in the presence of manual in-line immobilisation; (ii) blind nasal intubation if there is no compromise to the cribiform plate; (iii) blind oral intubation using the intubating laryngeal mask airway (ILMA); (iv) awake fibre-optic intubation; and (iv) surgical airway if intubation is not possible Direct laryngoscopy with in-line immobilisation is a safe and acceptable method B and C FALSE : A C5/C6 fracture will result in a VC 31% of predicted Note C5-C8-> complete intercostal muscle paralysis, and ineffective or no cough. Intubation indications with Cervical Spine injury * Prophylactic o VC < 15ml/kg (or <20% predicted) o Head or Chest Injuries * Therapeutic o Inability to clear secretions o Respiratory complications D. FALSE see above E. TRUE : Succinylcholine is the muscle relaxant of choice. The release of potassium associated with the use of succinylcholine in spinal cord injury has not been shown to be a problem until 3 days post-injury at the earliest. |
|
|
AZ75 ANZCA version [2005-Apr] Q127, [2005-Sep] Q3
The usual cardiovascular response to ECT (electro-convulsive therapy) is A. not predictable as it is very variable B. transient bradycardia followed by tachycardia and hypertension C. transient bradycardia with hypotension D. transient tachycardia and hypertension E. transient tachycardia followed by bradycardia and hypotension |
ANSWER B
Initial parasympathetic induced bradycardia lasting 10-15 seconds followed immediately by a more prominent sympathetic response that results in tachycardia and hypertension lasting 5 minutes or longer. |
|
|
AZ76b ANZCA Version [2006-Mar] Q123, [Jul06] Q50
A 70-yr-old man is to undergo removal of cataract and intraocular lens implantation. He has long-standing atrial fibrillation and is on warfarin. He has no other health problems. He has never had a stroke. A sub-tenon’s block is planned for the procedure. His INR is 2.5. What should be the perioperative management of his warfarin therapy and anticoagulant status? A. Interrupting warfarin therapy is optional for this procedure. If warfarin is interrupted for 5 days to allow normalisation of INR (< 1.5) no other perioperative anticoagulant prophylaxis is necessary B. Warfarin therapy should be ceased 5 days preoperatively and no other perioperative anticoagulant prophylaxis is necessary. Surgery should proceed if INR is < 1.5 C. Warfarin therapy should be ceased 5 days preoperatively. He should commence daily low molecular weight heparin, omitting the dose on the day of surgery. Surgery should proceed if INR is < 1.5 D. Warfarin therapy should be ceased 5 days preoperatively. He should take daily clopidogrel till surgery. Surgery should proceed if INR is < 1.5 E. Warfarin therapy should be ceased 5 days preoperatively. He should take daily low dose aspirin till surgery. Surgery should proceed if INR is < 1.5 |
None.
# Retrobulbar haemorrhage is rare with Subtenon's block # Retrobulbar haemorrhage is increased in people treated with warfarin even if it is stopped ? tissue fragility ? comorbidity # Retrobulbar haemorrhage is uncommonly sight threatening if a surgeon manages it immediately # The risks of thromboembolism are life threatening Continue warfarin. Test on the day of surgery. Don't stop aspirin or NSIADs Only for planned uncomplicated phaco INR<1.5 -peribulbar block INR <3.0 proceed with surgery -subtenon -topical LA INR >3.0 -postpone |
|
|
AZ77 ANZCA Version [Jul06] Q149
With regard to peri-operative cardiac risk reduction there is evidence that all of the following reduce perioperative cardiac morbidity EXCEPT A. intra-operative use of nitrous oxide B. peri-operative use of alpha-two agonists C. perioperative use of diltiazem D. peri-operative use of statins E. tight peri-operative glycaemic control (blood sugar between 3.5 and 6mmol.l-1) |
ANSWER A
|
|
|
AZ78 ANZCA Version [2006-Mar] Q124 [Jul07]
A 25-year-old 80 kg male with no other health problems is undergoing ECT (electroconvulsive shock therapy) for severe depression. Anaesthesia for his first 2 treatments consisted of thiopentone 350 mg and suxamethonium 50 mg. The treating psychiatrist is concerned at the limited duration of seizure activity with treatment despite maximal seizure stimulus. An acceptable seizure duration would be best be achieved by: A. adjunctive use of remifentanil to reduce the dose of induction agent B. clonidine premedication C. hypoventilating the patient to reduce seizure threshold D. pretreatment with lignocaine to reduce seizure threshold E. using propofol instead of thiopentone for induction of anaesthesia |
ANSWER A
A. TRUE : Anaesthesia Secrets' p513: Remifentanil 1 mcg/kg (makes it) possible to reduce the doses of methohexitone and propofol required to induce unconsciousness by 33% thus resulting in prolongation of ECT induced seizure duration. Adjunctive use of potent rapid and short acting opioid analgesics has become an effective way of extending siezure times in patients with short seizure duration. |
|
|
AZ79 ANZCA version [2003-Apr] Q100
The first step in developing a clinical audit should be to: A. define the question to be asked B. develop the relevant clinical protocol C. draw up the audit form D. find the relevant standards E. obtain ethics committee approval |
ANSWER A
Clinical audit - the process The clinical audit process seeks to identify areas for service improvement, develop & carry out action plans to rectify or improve service provision and then to re-audit to ensure that these changes have an effect.-->Clinical audit can be described as a cycle or a spiral, see figure. Within the cycle there are stages that follow the systematic process of: establishing best practice; measuring against criteria; taking action to improve care; and monitoring to sustain improvement. As the process continues, each cycle aspires to a higher level of quality. * Stage 1: Identify the problem or issue * Stage 2: Define criteria & standards * Stage 3: Data collection * Stage 4: Compare performance with criteria and standards * Stage 5: Implementing change |
|
|
AZ80 ANZCA version [2005-Sep] Q107, [Jul07] Mar10 Aug10
Which of the following is NOT an absolute contraindication to magnetic resonance imaging? A. cardiac pacemaker B. cerebral aneurysm clips C. cochlear implant D. implanted defibrillator E. prosthetic heart valve |
ANSWER E
Absolute Contraindications * electronically, magnetically, and mechanically activated implants: * cardiac pacemakers * ferromagnetic or electronically operated stapedial implants * hemostatic clips (CNS) * metallic splinters in the orbit Relative Contraindications * electronically, magnetically, and mechanically activated implants: * other pacemakers, e.g., - for the carotid sinus; - insulin pumps and nerve stimulators; - lead wires or similar wires * non-ferromagnetic stapedial implants * cochlear implants * prosthetic heart valves (in high fields, if dehiscence is suspected) * hemostatic clips (body) * makeup and tattoos * congestive heart failure * pregnancy (claustrophobia) |
|
|
AZ81 ANZCA version [2005-Sep] Q129
The adverse outcomes resulting in the most frequent medicolegal claims against anaesthetists are A. dental damages from airway instrumentation B. eye injuries C. non-obstetric epidural complications D. obstetric epidural complications E. peripheral nerve injuries |
ANSWER A
1. Cass NM. Medicolegal claims against anaesthetists: a 20 year study. Anaesth Intensive Care. 2004 Feb;32(1):47-58. PMID 15058121 2. Aders A, Aders H. Anaesthetic adverse incident reports: an Australian study of 1,231 outcomes. Anaesth Intensive Care. 2005 Jun;33(3):336-44. PMID 15973916 |
|
|
AZ82 ANZCA version [2005-Sep] Q105,
In the elderly patient A. renal dysfunction can be excluded if the serum urea and creatinine concentration are within normal limits B. sedation does not negate the benefits of regional anaesthesia with respect to postoperative cognitive dysfunction C. shivering may be less effective in restoring body temperature, than in younger adults D. the effect of ephedrine in treating hypotension is similar to younger adults E. the uptake of sevoflurane is similar to younger adults, because of its low blood gas solubility |
ANSWER C
A. False B. False "The advantages of regional anaesthesia with respect to postoperative cognitive dysfunction are only maintained if sedation is avoided" C. True "elderly or debilitated patients shiver less effectively than younger patients" Perioperative hypothermia in the high-risk surgical patient. Best Practice & Research Clinical Anaesthesiology, Volume 17, Issue 4, Pages 485-498 K. Leslie, D. Sessler D. False "The elderly have a poor response to exogenous b-agonists therefore a-agonists should be used". E. False, newer insoluble volatiles(eg Sevo) are ass with a slower uptake in the elderly dt increased V/Q Mismatch and shunting. |
|
|
[ANZCA version Apr08 q123]
All the following are predictors of difficult intubation EXCEPT: A. Inter-incisor distance <3cm B. Prominent C1 spinous process C. Prominent maxillary canines D. Samsoon classification - Class IV E. TMD <6cm |
ANSWER B
|
|
|
PZ106 ANZCA Version [Jul06] Q136, [Apr07]
A 25-year-old male presents for ECT (electroconvulsive shock therapy) at a free-standing facility. He has a life-threatening depressive illness that has not responded adequately to medication, however he is still taking tranylcypramine (Parnate). You should A. cancel the procedure, cease tranylcypramine and perform the ECT in 2 weeks B. proceed with the ECT, but induce with midazolam and remifentanil C. proceed with the ECT, but pre-treat with esmolol D. proceed with the ECT with caution, but with your usual drugs E. transfer the patient to a tertiary centre for their ECT |
ANSWER D
The problem with ECT is the vagal stimulus followed by an overwheling sympathetic surge. -significant risk of a hypertensive crisis with MAOI -avoid sympathomimetic drugs and stimulating sympathetic NS -discontinuing MAO inhibitors at least 2 weeks prior to elective surgery is no longer recommended -with the expection of trachlcypromine (irreversible enzyme inhibition, 2 weeks to regernate new enzymes) However, this is an emergency and should go ahead with precautions -avoid pethidine : hyperthermia, seziures and coma -exaggerated response to vasopressors and sympatheometics -consider use of esmolol to blunt sympathetic surge but this may worsen brady -avoid ketamine and pancuronium as they enhance the sympathetic response |
|
|
IC85 [Apr07] Q115
A young woman has an MVA when driving home from a nightclub. She was known to have moderate MDMA (ecstasy) consumption. Which of the following complications is least likely to be due to MDMA? A. Hyponatraemia B. Hypotension C. Pneumothorax D. Sweating E. Tachycardia |
ANSWER B
A. FALSE : multifactorial due to dehydration, excessive sweating, increase water intake, surge in ASH -can result in seziures and coma B. TRUE : MDMA causes tachycardia and hypertension. Any hypotension in a trauma situation is hypovolaemia until proven otherwise. C. FALSE : there are case reports of pneumonthorax attributed to estasy as the result of excessive physical activity against a closed glottis (valsalva) => alveolar rupture D. FALSE E. FALSE 2 Minor clinical symptoms and signs seen with MDMA Tachycardia Elevated mood Hypertension Confusion Mydriasis Ataxia Dry mouth Nystagmus Sweating Bruxism (jaw clenching) |
|
|
ANZCA Version [Apr 07]
A 60y.o. man with a 45 pack year history of smoking and heavy drinking presents with stridor. He has had a hoarse voice for about 4 months. He has been waking at night for a week with difficulty breathing relieved by sitting up. He is sitting upright in bed with moderate inspiratory stridor. His SaO2 on air is 95%. The next step in his management should be A. awake fibreoptic intubation B. CT scan of the neck C. examination under anaesthesia following gaseous induction D. nasenoscopy under topical anaesthesia E. tracheostomy under LA |
ANSWER D
This patient has upper airway obstruction -currently stable -but likely to progress to complete obstruction Options to secure airway include 1. ETT (Inhalational, AFOI) 2. Tracheostomy (LA or GA) This will depend on evaluation, diagnosis, and level of skill and speed. Fibre-optic nasendoscopy must be performed by the ENT surgeon in the out-patient clinic or on the ward. It may require no local anaesthesia or simple preparation of the nose with lidocaine and epinephrine. A CT scan may help to locate the tumor and aid tracheostomy placement. |
|
|
RH26b ANZCA version [2004-Apr] Q126, [Jul07]
To achieve maximum anaesthesia with minimal risk of trauma to veins, the tip of a needle used for a medial peribulbar injection should be advanced no further past the equator of the globe than A. 5 mm B. 10 mm C. 15 mm D. 20 mm E. 25 mm |
ANSWER B
|
|
|
RH31 [Apr07] Q70
In performing a retrobulbar block, the complication of brainstem anaesthesia: A. Is not associated with contralateral amaurosis B. Has an incidence of approximately 1 in 2000 blocks C. Becomes clinically apparent within 2 to 15 minutes D. Usually takes 4 to 6 hours to resolve E. Is associated with increased auditory acuity |
ANSWER C
Complication from Brain stem anaesthesia -LA spread along optic nerve sheath -mostly likely with retobulbar -prevalence of 0.1%-0.3% -rare if needle is less than 31mm Symptoms and signs -drowsiness -lightheadness -confusion -loss of verbal contact -incranial nerve palsies -convulsions -respiratory depression -respiratory arrest -cardiac arrest *onset within 10minutes *lasy up to 2-3 hours Prevention -minimised using short, fine needles -eye looking straight ahead |
|
|
TMP-126 ANZCA version [Apr08] Q119
With regard to surgical antibiotic prophylaxis, which of the following statements is LEAST correct? A. cephalosporins can usually be safely administered to penicillin allergic patients B. clindamycin can be indicated in penicillin allergic patients C. they should be administered at the time of surgical incision D. the ideal timing of administration is less than 30 minutes prior to surgical incision E. vancomycin should be given routinely in MRSA (methicillin resistant staphylococcus aureus) prevalent areas |
ANSWER E
|
|
|
AZ In performing an awake fibreoptic intubation it is MOST important that care is taken to avoid:
a. Causing any bleeding that will obstruct view b. Oversedation as leads to posterior pharyngeal wall collapse c. Trauma to nasal turbinates d. Touching vocal cords as will induce coughing e. Oral route as may bite the fibreoptic scope |
ANSWER B
Oversedation results in posterior wall collapse and reduction in cough (which maybe a problem if bleeding) |
|
|
27. (NEW) As per ANZCA Acute Pain Guidelines (2nd ed update), after a prophylactic subcutaneous dose of heparin, minimum time before you can remove epidural catheter is
a. 2 hours b. 4 hours c. 6 hours d. 8 hours e. 10 hours |
ANSWER B
1) Anticoagulation is the most important risk factor for epidural haematoma -followed by insertion of epidural needle/catheter -coagulopathy ASRA guidelines 2003 (updated version 2010) 1. Antiplatelet medications : -NSAIDS alone do not significantly increase risk of spinal haematoma -tirofiban : wait 4-8 hours -abciximab : wait 24-48 hours -clopidogrel : wiat 7 days -ticlopidine : wait 14 days 2) Unfractionated SC heparin -not a contraindication -rule out HITs if heparin has been administered > 4days -wait 6 hours to insert/remove -wait 2 hours to give heparin 3) Unfractionated IV heparin -wait till normalization of coagulation before inserting or removing -wait hour after removal before giving IV hep 4) LMWH -wait 12 hours to insert/remove -wait 2 hours for next LMWH dose 5) Warfarin -stop warfarin 4-5 days prior and measure INR -INR checked prior to removal -INR <1.5 is safe to insert/remove 6) Fibrinolysis and thrombolysis -absolute contraindication -no data on the safe time interval -no recommendations 7) Herbal -garlic, ginkgo and ginseng have effects on haemostasis, there are currently no specific concerns about their use with neuraxial blockade. |
|
|
TMP-101 [Mar10] [Aug10]
Aneurysm sugery. Propofol/remifentanil/NMDR. DOA monitoring (Entropy). MAP 70 , HR 70/min, State entropy 50, Response entropy 70. What do you do? A. ? B. Metaraminol C. Check TOF D. Nothing E. Increase TCI |
ANSWER C
Response entropy is a product of EMG & EEG. This implies that there is muscle activity & I would check TOF to see if more relaxant is required |
|
|
Can05-8 A pediatric patient is having a laparotomy for resection of a neuroblastoma. What is the best way to avoid hypothermia?
A. Set the room temperature at 29 degrees Celsius B. Warm IV fluids C. Forced air warmer D. Humidified inhaled air |
ANSWER C
|
|
|
AC153 ANZCA version [2004-Aug] Q137
When considering perioperative hypothermia A. the brain and major abdominal organs generate more metabolic heat than resting muscle B. the pattern of intra-operative hypothermia has 2 phases C. induction of general anaesthesia leads to a core temperature drop of < 0.5oC within the first hour D. the extent of redistribution hypothermia is primarily related to patient initial body heat content E. conduction contributes most to heat loss during the linear phase of hypothermia |
ANSWER A
A. TRUE : The brain and major organs in the trunk are the most metabolically active tissues and generate more metabolic heat than does muscle at rest B. FALSE : 3 phases C. FALSE : A quantitative study of systemic heat balance and regional body heat distribution in volunteers indicated that after 1 h of anesthesia, core temperature decreased 1.6°C, with redistribution contributing 81% to the decrease. D. FALSE : the degree of effect of redistribution is related to the initial difference between core and peripheral temperatures E. FALSE : radiation is 60% heat loss linear phase |
|
|
Black Bank March 2010
27. Best way to prevent hypothermia in patient undergoing a general anaesthetic (Repeat question) A. Prewarming of patient B. C. D. Warm IV fluids |
ANSWER A
|
|
|
Black Bank March 2010
ET03 Jehovah's witness patient refusing blood products. The ethical principle you are honouring if you continue with elective hip operation A. Autonomy B. Nonmaleficience C. Justice D. Paternalism |
ANSWER A
|
|
|
Black Bank March 2010
ET01 An 86yo with severe dementia and multiple medical problems.. Surgeons want to operate for faecal peritonitis/bowel perforation, and believe he will die without the surgery. Your decision NOT proceed with surgery is supported by which ethical principle? A. Dignity B. Competence C. Non-maleficience D. Paternalism E. Futility |
ANSWER E
|
|
|
Black Bank March 2010
64.Most distant anatomy seen on grade III laryngoscopy A. soft palate B. hard palate C. Epiglottis D. arytenoid cartillage E. opening to ? |
ANSWER D
|
|
|
Black Bank March 2010
64.Most distant anatomy seen on grade III laryngoscopy A. soft palate B. hard palate C. Epiglottis D. arytenoid cartillage E. opening to ? |
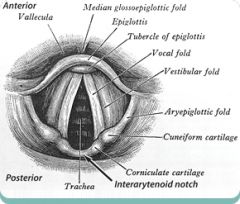
ANSWER D
|
|
|
Black Bank March 2010
SZ80 Which of the following is not an absolute contra-indication for MRI? A. cochlear implant B. heart valve prosthesis C. ICD D. pacemaker E. intracranial clips |
ANSWER A
Absolute Contraindications * electronically, magnetically, and mechanically activated implants: * cardiac pacemakers * ferromagnetic or electronically operated stapedial implants * hemostatic clips (CNS) * metallic splinters in the orbit Relative Contraindications * electronically, magnetically, and mechanically activated implants: * other pacemakers, e.g., - for the carotid sinus; - insulin pumps and nerve stimulators; - lead wires or similar wires * non-ferromagnetic stapedial implants * cochlear implants * prosthetic heart valves (in high fields, if dehiscence is suspected) * hemostatic clips (body) * makeup and tattoos * congestive heart failure * pregnancy (claustrophobia) |
|
|
Black bank August 2010
TMP-Jul10-005 (This is a very old repeat) Relative humidity – air fully saturated at 20 %. What is the relative humidity at 37 degrees ? A. 20 B. 30 C. 40 D. 50 E. 60% |
ANSWER C
1m3 of air at 20˚C, 100% saturated, contains about 17g of water. If it is warmed to 37˚C, the mass of water vapour or absolute humidity is still the same but the relative humidity is only 39%, as at 37˚C, 1m3 of air contains 44g of water vapour when fully saturated and the ratio of 17 to 44 gives a value of 39% |
|
|
Black Bank August 2010
MC161 Drug eluting stent 6 months old. On aspirin and prasugrel 10mg. Elective lap cholecystectomy for biliary colic. A. Do case while taking both. B. Do case while stopping both. C. Stop Prasugrel for 7 days, keep taking aspirin. D. Stop Prasugrel for some other different time E. Post-pone for 6 months |
ANSWER E
As per AHA/ACC Guidelines -recommended to continue dual anti-platelet therapy for 365 days, -Given that this is an elective procedure, and the potential for blood loss (while usually minimal) is significant (especially given dual anti-platelet therapy), the procedure should be delayed for another 6 months (i.e. 12 months from time of stent placement). The risk of an in-stent thrombosis is high if both anti-platelet drugs are not continued for the full 12 months. |
|
|
Black bank August 2010
117. A 12 year old child with hip dislocation at 4pm. Ate something 1 hour after injury. Now 11 pm. Best anaesthetic: A. RSI with ETT B. delay until next day then treat elective C. inhalational induction and continue with face mask D. Reduce immediately with iv sedation E. inhalational induction and continue with face mask |
ANSWER A
|
|
|
Black bank August 2010
TMP-Jul10-041 New onset atrial fibrillation in a 10 week pregnant lady. BP 150/90, HR 160, SaO2 92%. Moderate mitral stenosis on TTE, no thrombus seen. Emergency doctor gave her anticoagulant (not specified what). Most appropriate management: A. Verapamil B. Labetalol 20mg iv to 300mg C. Amiodarone 300mg IV D. Synchronised biphasic cardioversion with 70-100 Joule E. Oral digoxin -1000mcg then 500mcg 6 hrs later |
ANSWER D
In a pregnant woman who develops AF -diagnosis and treatment of the underlying condition causing the arrhythmia -ventricular rate should be controlled with digoxin, a beta blocker, or a nondihydropyridine calcium channel antagonist -All currently available antiarrhythmic drugs have the potential to cross the placenta and enter breast milk and should therefore be avoided if possible. -Quinidine, sotalol, flecainide, and amiodarone have all been used successfully during pregnancy, however, in relatively small numbers of cases. -Quinidine has the longest record of safety in pregnant women and remains the agent of choice for pharmacological cardioversion of AF in this situation. **In the event of hemodynamic embarrassment, direct-current cardioversion can be performed without fetal damage This patients Sats 92%, ?progressing failure and should be cardioverted |
|
|
Black bank August 2010
TMP-106 A 75yo male with moderate aortic stenosis (valve area 1.1cm2).. Gets mild dyspnoea on exertion but otherwise asymptomatic. Needs hip replacement. A. Continue with surgery B. Beta block then continue C. Get myocardial perfusion scan D. Postpone surgery awaiting AVR E. Postpone surgery awaiting balloon valvotomy |
ANSWER D
if the aortic stenosis is symptomatic, elective noncardiac surgery should generally be postponed or cancelled. Such patients require aortic valve replacement before elective but necessary noncardiac surgery Indications for AVR -mean P gradient > 40mmHg -valve area < 1.0 cm2 -symptomatic |
|
|
Black bank August 2010
SZ11 Lowering intra-ocular pressure by applying pressure to the globe (e.g. Honan balloon) is typically contraindicated in a patient having A. a revision corneal graft B. a revision trabeculectomy C. an extra-capsular lens extraction D. a redo vitrectomy E. repeat retinal cryotherapy |
ANSWER B
|
|
|
Black bank March 2011
ET02 An 85y.o for open AAA repair. Refuses blood because of risk of vCJD. You tell him you won't anaesthetise him as the risk is too high. This is an example of: A: Autonomy B: Beneficence C: Malevolence D: Coercion E: Paternalism |
ANSWER C
A. Autonomy would be to respect the patients decision to refuse blood and continue with the case after discussing the risks, optimising and considering alternatives B. FALSE C. TRUE : Maleflicence : first do no harm D. FALSE : Coercion would be to pursuade him to accept blood E. FALSE : Paternalism would be to anaesthetise him and given him blood regardless of his views. |
|
|
Black Bank March 2011
24. NEW. When compared to a non-obese patient, in an obese patient (BMI >35) when fasted for an elective procedure the gastric secretion will have: A: more volume, higher pH B: more volume, lower pH C: same volume, same pH D: less volume, lower pH E: less volume, higher pH |
ANSWER C
the study of Vaughan, in a study with 256 patients undergoing elective surgical interventions, did not observe statistically significant differences in gastric volume and pH between obese and non-obese patients. |

