![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
53 Cards in this Set
- Front
- Back
|
The zona pellucida is a viscous gel surrounding the oocyte, what is the name for the cells that surround it?
|
Cumulus cells (need to be broken through by the spermatozoon)
|
|
|
What is 'cleavage'? Where does it go on?
|
Partitioning of the single large zygote into a ball of smaller cells. Goes on along the uterine tube, towards the uterine cavity
|
|
|
Each of the cells that results from cleavage is known as a __________
|
Blastomere
|
|
|
What is a 'morula'? When is it present?
|
Cleaving division converts the single large egg into a solid mass of smaller cells known as a morula.
~12-16 cells, day 3 |
|
|
During the 8-16 cell stage, outer cells of the morula flatten against each other in a change called _____________
|
compactation (increases cell-to-cell contact)
|
|
|
During compactation, , outer cells make watertight 'tight junctions' to form an epithelium. They pump fluid into the interior of the morula, creating a cavity known as the...
|
Blastocoele
|
|
|
When the blastocoele is formed, the morula changes name to become known as a:
|
Blastocyst
|
|
|
What is the name for the cells on the outer epithelium of the blastocyst?
|
Trophoblast cells
|
|
|
What is the name for the cell clump inside the blastocyst?
|
Inner cell mass (embryoblast)
|
|
|
What is 'ectopic implantation'?
|
Implantation in an abnormal place
|
|
|
How many days after fertilisation does implantation take place?
|
6-7 days
|
|
|
What is the 'syncytiotrophoblast'? What cells does it consist of?
|
A specialsed tissue, formed by the fusing of trophoblast cells and uterine epithelial cells (it is a very early stage of implantation)
It consists of giant cells which make 'proteolytic' enzymes which break down surrounding maternal tissue - ensuring proper implantation within 2-4 days of attachment |
|
|
Once the blastocyst attaches to the uterine wall, how long does it take to become full yimplanted?
|
2-4
|
|
|
When the blastocyst burrows into the uterine wall, maternal tissue is damaged. What does it then do?
|
Forms a fibrin plug, sealing it in place in the uterine wall
|
|
|
Where does implantation normally take place?
|
Middle or upper part of the uterine cavity - hight on the dorsal wall between openings of the uterine (fallopian) tubes
|
|
|
What is 'placenta praevia'?
|
A condition where, due to ectopic implantation, the placenta grows over the cervix - leading to haemorrhaging in late pregnancy
|
|
|
What is the effect of the antiprogesterone drug 'RU-486' (mifepristone)?
|
It dislodges an already implanted embryo by triging menstruation artificially (it s a safe abortifacient up to the sixth week of development)
|
|
|
What is 'luteinisation'?
|
When the ovarian follicle becomes filled with secretory cells forming a yellowish swelling called the luteal body (corpus luteum)
|
|
|
Which hormone does the corpus luteum secrete? What effect does it have?
|
Progesterone. It prepares the endometrium for implantation.
If, after 10-14 days, it does not occur - levels fall and trigger menstruation |
|
|
After 10-14 days, ordinarily the corpus luteum will normally stop secreting progesterone - causing mensturation. If there is an implantation - what is done to stop it?
|
The trophoblast cells secrete 'human chronic gonadotrophin' (hCG)
This causes the CL to keep secreting progesterone until the placenta itself can make it |
|
|
What are common causes of infertility?
|
Fairly of oocyte maturation
Failure to make enough motile sperm Ejaculation of semen into the bladder Female production of antibodies against sperm! Maternal ageing - chromosomal abnormalities |
|
|
What are the two types of trophoblast cells present during implantation ~day 8
|
Syncytiotrophoblast - Giant, invasive cells
Cytotrophoblast |
|
|
What is 'gastrulation'?
|
When the morphology of the embryo is reorganized to form the three germ layers: ectoderm, mesoderm, and endoderm
|
|

|
|
|
|
What forms the amniotic cavity?
|
The fluid pumping action of the epithelial cells of the epiblast
|
|
|
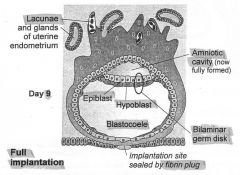
Day 9: What is the name for epiblast cells that lie in close contact with the cytotrophoblast? What is the name for the membrane formed later on?
|
Amnioblasts
Amnion layer |
|
|
What is the name for the disk formed between epiblast cells in close contact with the hypoblasts?
|
Bilaminar germ disk
|
|
|
Day 9: What is the name for the epiblast cells that are very near to the cytotrophoblast? What membrane do the form?
|
Amnioblast cells. They form the 'amnion' membrane.
|
|
|
Day 9: Hypoblast cells spread out and line the blastocoele - this lined cavity is now known as the...
|
...primary yolk sac.
|
|
|
What is the name for the tissue that divides the cytotrophoblast from the primary yolk sac?
|
The extraembryonic reticulum
|
|
|
Day 12-13: The extraembryonic reticulum grows and develops microcavities that fuse to form a single, continuous cavity. What is the name for this?
This cavity is also connected at a certain point - what is this point called? |
The extraembryonic coelom.
The connecting stalk. (This later forms the umbilical chord) |
|
|
How, and when, is the secondary yolk sac formed?
|
~Day 13. Hypoblast cells migrated around the wall of the primary yolk sac to form the secondary one.
The old sac is pinched off and degenerates |
|
|
What is the 'chorin'?
|
A tough membrane formed by the fused outer layer of the extraembryonic reticulum (containing mesoderm) and the cytotrophoblast.
|
|
|
What is the origin of mesoderm cells? (I.e. when and where)
|
They are found in the extraembryonic reticulum around day 14
|
|
|
Once the chorion has formed, the extraembryonic coelom is now called the...
|
Chorionic cavity
|
|
|
What is 'gastrulation'? When does it start.
|
Starts: day 14. It is the conversion of the bilaminar germ disk into a three layered disk - the trilaminar germ disk (from which all the tissues of the embryo are derived).
|
|
|
Day 14: What is the 'embryonic mesoderm' layer?
|
A middle layer between formed when cells migrate between the epiblast and hypoblast layer
|
|
|
Day 15: How is endoderm formed?
|
Cells from the epiblast layer migrates into the hypoblast layer (not well understood)
|
|
|
Day 15: After gastrulation, what is the name given to the remaining epiblast cells?
|
Ectoderm
|
|
|
What is the first visible sign of the head-to-tail axis of the embryo?
|
The primitive streak
|
|
|
What is the lump at the end of the primitive streak known as?
|
The primitive node
|
|
|
The primitive streak marks a V-shaped crease that cells burrow into, breaking away from the epiblast layer at its base
|
.
|
|
|
The head of the embryonic acis is called the _________ _____. This plate later becomes the _______________ ________ and has a role in the formation of the _____
|
Prochordal plate, buccopharyngeal membrane, mouth
|
|
|
Where is the heart formed from?
|
The cardiogenic region - at the head of the body axis
|
|
|
What is the 'cloacal membrane'?
|
At the tail end of the embryonic axis - forms anal (teehee) canal and urogenital system
|
|
|
What is the notochord?
|
The part that establishes the main body axis.
It is important in sending signals to the ectoderm to set up the NS (this process is called neural induction') |
|
|
What does node-derived mesoderm/prechordal mesoderm develop into (near notochord)?
|
Head formation.
|
|
|
What is the name for the specialised region of ectoderm that results from neural induction? What does it ultimately form?
|
The neural plate (ultimately forms brain and spinal chord)
|
|
|
Why is the vascular system developed so early on? When does it begin to appear?
|
Diffusion is ineffective over large distances and would limit growth. Middle of the third week
|
|
|
What is the 'cardiogenic region'
|
Clusters of angiogenic cells around the cranial edge of the embryonic disk involved in forming vascular tubes. Including 'primitive heart tubes' that fuse to form the basis of the heart.
|
|
|
Fusion of the sperm to the egg membrane triggers a release of calcium. What are the two effects of this?
|
Zona reaction - ZP2 cleaved to harden - this excludes sperm
Meiosis II is completed with extrusion of the second polar body |
|
|
Cleavage is/isn't synchronised in humans.
|
Is not (i.e. cells do not neatly got 1-2, 2-4, 4-8, some will divide at other times)
|
|
|
What are the four roles of the ZP?
|
Preventing polyspermy
Stabilising the zygote Preventing ectopic pregnancy Protection from immune system |

