![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
110 Cards in this Set
- Front
- Back
|
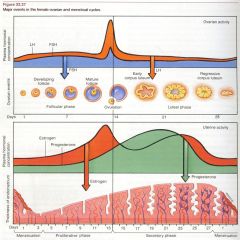
Give the length of each phase of the menstrual cycle.
|
follicular phase: days 1-13, but varies
ovulation: day 14 (or first day following follicular phase) luteal phase: days 15-28 (this is always 14 days, the length of time the corpus luteum can survive without further LH) |
|
|
Describe the hormonal trends (LH, FSH, estrogen, progesterone) of the normal menstrual cycle.
|
|
|
|
What is the definition of premature menopause?
|
ovarian failure and menstrual cessation before age 40
|
|
|
What are the predominant features of menopause?
|
"HAVOC"
Hot flashes (vasomotor instability) Atrophy of the Vagina Osteoporosis Coronary artery disease |
|
|
What laboratory changes are observed in menopause?
|
first: increased FSH
next: increased LH total cholesterol increased, HDL decreased |
|
|
What is the treatment for the vasomotor symptoms of menopause?
|
hormone replacement therapy with combination estrogen and progestin
|
|
|
What are the risks associated with hormone replacement therapy (HRT)?
|
increased cardiovascular morbidity and mortality
may increase risk of breast and endometrial cancers |
|
|
Why is progestin included in HRT?
|
unopposed estrogen in patients with a uterus predisposes to endometrial cancer
post-hysterectomy patients do not need progestin |
|
|
What are contraindications to HRT (6)?
|
vaginal bleeding
suspected or known BRCA endometrial CA history of thromboembolism chronic liver disease hypertriglyceridemia |
|
|
What non-HRT therapy can be offered to menopausal patients to reduce the frequency of hot flashes?
|
venlafaxine
clonidine (less common) |
|
|
What is the treatment for vaginal atrophy of menopause?
|
estrogen vaginal cream (short term)
estradiol vaginal ring (long-term) |
|
|
What percent of sexually active, premenopausal women will become pregnant within one year if no contraception is used?
|
85%
|
|
|
What are the absolute contraindications to estrogen-containing methods of contraception?
|
pregnancy
history of CAD or DVT BRCA undiagnosd abnormal vaginal bleeding estrogen-dependent CA benign or malignant liver neoplasm current tobacco use + age >35 |
|
|
What are the absolute contraindications to use of IUDs?
|
known or suspected pregnancy
unexplained vaginal bleeding current purulent cervicitis active or recurrent PID (within 3 mos) confirmed symptomatic actinomycosis bicornuate or septate uterus cervical or uterine CA Pap smear with SIL or two atypical Pap smears history of heart valve replacement or artificial joints |
|
|
Give the DDx of pediatric vaginal discharge (5).
|
infectious vulvovaginitis
STD resulting from sexual abuse foreign objects candidal infections sarcoma botryoides (rhabdomyosarcoma) |
|
|
Describe the two types of precocious puberty.
|
central: results from early activation of hypothalamic GnRH production; most commonly idiopathic; may be related to obesity; may be caused by CNS tumors
peripheral: also called pseudo-precocious; results from non-hypothalamic GnRH production |
|
|
Distinguish between signs of estrogen excess and signs of androgen excess in precocious puberty.
|
estrogen excess: breast development and possibly vaginal bleeding
androgen excess: pubic and/or axillary hair, enlarged clitoris, acne, increased body odor |
|
|
What do estrogen excess and androgen excess suggest, respectively?
|
estrogen excess: ovarian cysts or tumors
androgen excess: adrenal tumors or congenital adrenal hyperplasia |
|
|
What is the first step in the diagnosis of precocious puberty?
|
obtain wrist/hand x-ray to assess bone age
if bone age is within 1y of chronological age, puberty has not begun or has just begun if bone age is >2y from chronological age, puberty has been present for at least one year or is progressing rapidly |
|
|
What is the second step in diagnosis of precocious puberty, after determination of bone age?
|
conduct a GnRH (leuprolide) stimulation test
|
|
|
How can central precocious puberty be distinguished from peripheral precocious puberty using the GnRH (leuprolide) stimulation test?
|
central: LH response to GnRH stim test is positive (obtain cranial MRI to look for CNS tumors)
peripheral: LH response to GnRH stim test is negative |
|
|
What steps should be taken if a GnRH (leuprolide) stimulation test for precocious puberty is negative?
|
workup for peripheral precocious puberty:
obtain U/S of ovaries and/or adrenal glands measure estradiol (increased in ovarian cysts/tumors) measure androgens measure 17-OH progesterone |
|
|
What is the treatment for central precocious puberty?
|
leuprolide
with treatment, physical changes regress or cease to progress |
|
|
What is the treatment for peripheral precocious puberty?
|
treat the cause
ovarian cysts: usually no Tx necessary CAH: treat with corticosteroids; surgery not required for Tx of ambiguous genitalia adrenal/ovarian tumors: surgical resection McCune-Albright syndrome: antiestrogen medications (e.g. tamoxifen) and estrogen synthesis blockers (ketoconazole, testolactone) |
|
|
Define primary amenorrhea.
|
absence of menses by age 16 with secondary sexual development present
or absence of secondary sexual characteristics by age 14 |
|
|
Give the possible etiologies of primary amenorrhea with absent secondary sexual characteristics (no estrogen production).
|
constitutional growth delay (MCC)
primary ovarian insufficiency (most commonly Turner's) central hypogonadism |
|
|
What factors may cause central hypogonadism?
|
undernourishment
stress prolactinemia exercise CNS tumors or cranial irradiation Kallmann's syndrome (isolated gonadotropin deficiency; associated with anosmia) |
|
|
Give the possible etiologies of primary amenorrhea WITH secondary sexual characteristics (evidence of estrogen production but other genetic or anatomic problems).
|
Mullerian agenesis
imperforate hymen complete androgen insensitivity (breast development, but no menses or pubic hair) |
|
|
What is the first step in the diagnosis of primary amenorrhea?
|
pregnancy test
|
|
|
What is the second step in the diagnosis of primary amenorrhea, after obtaining a pregnancy test?
|
radiograph to determine bone age
|
|
|
How should bone age results be interpreted in the workup of primary amenorrhea?
|
if bone age <12 years (short stature) with normal growth velocity, constitutional growth delay is probable cause
if bone age is >12 years but no sign of puberty, obtain LH, FSH and consider location of problem on HPA axis |
|
|
Interpret the following laboratory findings in a patient with primary amenorrhea:
1. low GnRH; low LH, FSH; low estrogen, progesterone (prepuberty levels) 2. low GnRH; low LH, FSH; low estrogen, progesterone 3. high GnRH; high LH, FSH; low estrogen, progesterone 4. high GnRH; high LH, FSH; high estrogen, progesterone 5. normal pubertal hormone levels |
1. constitutional growth delay
2. hypogonadotropic hypogonadism (hypothalamic or pituitary problem) 3. hypERgonadotropic hypogonadism (points to ovarian failure to produce estrogen) 4. PCOS or problem with estrogen receptors 5. anatomic problem (menstrual blood can't get out) |
|
|
Give the DDx of primary amenorrhea presenting with hypogonadotropic hypogonadism.
|
Kallmann's syndrome
hypothyroidism hyperprolactinemia tumor infection trauma chronic disease anorexia excess exercise weight loss stress |
|
|
Give the DDx of primary amenorrhea presenting with hypERgonadotropic hypogonadism.
|
Turner's syndrome
premature ovarian failure (chemo, radiation, idiopathic) pure gonadal dysgenesis Savage's syndrome (gonadotropin-resistant ovary) |
|
|
Give the DDx of secondary amenorrhea presenting with hypogonadotropic hypogonadism.
|
Sheehan's syndrome
neoplasms panhypopituitarism hyperprolactinemia hypothyroidism anorexia excess exercise weight loss stress |
|
|
Give the DDx of secondary amenorrhea presenting with hypERgonadotropic hypogonadism.
|
premature ovarian failure (primary hypogonadism before age 40)
menopause chemotherapy with alkylating agents |
|
|
Give causes of primary and secondary amenorrhea due to anatomic problems (normal hormone levels).
|
primary:
imperforate hymen transverse vaginal septum vaginal and/or cervical agenesis Mullerian agenesis secondary: Asherman's syndrome due to emdometritis, scarring after delivery, or D&C cervical stenosis |
|
|
Give the treatment for the following causes of primary amenorrhea:
1. constitutional growth delay 2. hypogonadism 3. anatomic |
1. no treatment needed
2. begin HRT with estrogen alone at lowest dose; after 12-18 mos, begin cyclic estrogen/progesterone therapy 3. generally requires surgical intervention |
|
|
Define secondary amenorrhea.
|
absence of menses for six consecutive months in women who have passed menarche
|
|
|
What is the first step in the diagnosis of secondary amenorrhea?
|
pregnancy test
|
|
|
What is the second step in the diagnosis of secondary amenorrhea, following a pregnancy test?
|
negative beta-hCG: measure TSH and prolactin to assess for hypothyroidism or hyperprolactinemia
normal beta-hCG: initiate a progestin challenge (10 days of progestin) |
|
|
Describe both positive and negative responses to a progestin challenge.
|
positive progestin challenge (withdrawal bleed): indicates anovulation likely due to non-cyclic gonadotropin secretion, pointing to PCOS or idiopathic anovulation
negative progestin challenge (no bleed): indicates uterine abnormality or estrogen deficiency; check FSH levels |
|
|
What do high and low levels of FSH following a negative progestin challenge indicate, respectively?
|
high FSH: indicates hypERgonadotropic hypogonadism/ovarian failure
low FSH: obtain a cyclic estrogen/progesterone test; a withdrawal bleed from this test indicates hypogonadotropic hypogonadism; no bleeding suggests endometrial or anatomic problem |
|
|
What is the next best step in a woman with secondary amenorrhea and signs of hyperglycemia (polyuria, -dipsia) or hypotension?
|
1mg overnight dexamethasone suppression test to distinguish CAH, Cushing's, Addison's
|
|
|
What is the next best step in a woman with secondary amenorrhea and clinical signs of virilization?
|
measure testosterone, DHEAS, and 17-OH progesterone
mild virilization suggests PCOS, CAH, or Cushing's moderate-severe virilization suggests ovarian or adrenal tumor |
|
|
Give the treatment for secondary amenorrhea of the following etiologies:
1. hypothalamic 2. tumors 3. premature ovarian failure |
1. reverse underlying cause; induce ovulation with gonadotropins
2. excision; medical therapy for prolactinomas (e.g. bromocriptine, cabergoline) 3. if uterus is present, treat with estrogen plus progestin replacement therapy |
|
|
Define primary dysmenorrhea.
What is the usual mechanism of primary dysmenorrhea? |
menstrual pain associated with ovulatory cycles in the absence of pathologic findings
uterine vasoconstriction leads to anoxia and sustained contractions mediated by an excess of prostaglandin (PGF2-alpha) |
|
|
What is the treatment for primary dysmenorrhea?
|
NSAIDs
topical heat therapy combined OCPs Mirena IUD |
|
|
What is the definition of secondary dysmenorrhea?
Name some common causes of secondary dysmenorrhea (6) |
menstrual pain for which an organic cause exists
endometriosis, adenomyosis tumors fibroids adhesions polyps PID |
|
|
What is the first step in the diagnosis of secondary dysmenorrhea?
|
obtain beta-hCG to exclude ectopic pregnancy
|
|
|
What is the second step in the diagnosis of secondary dysmenorrhea, following a negative pregnancy test?
|
CBC w/ diff
UA (r/o UTI) GC/CT swab (r/o STDs, PID) stool guaiac (r/o GI pathology) |
|
|
What is the third step in diagnosis of secondary dysmenorrhea after pregnancy test and labs have been negative/normal?
|
look for pelvic pathology causing pain
|
|
|
Discuss endometriosis v. adenomyosis with respect to the following characteristic:
location |
endometriosis: endometrial glands and stroma outside the uterus
adenomyosis: endometrial tissue within the myometrium of uterus |
|
|
Discuss endometriosis v. adenomyosis with respect to the following characteristic:
history, physical exam |
endometriosis: classically, cyclic pelvic and/or rectal pain with dyspareunia
adenomyosis: noncyclical pain, menorrhagia, enlarged uterus |
|
|
Discuss endometriosis v. adenomyosis with respect to the following characteristic:
diagnosis |
endometriosis: direct visualization by laparoscopy (blue-black "raspberry" or dark brown "powder burned" appearance; "chocolate cysts" on ovaries)
adenomyosis: ultrasound or MRI |
|
|
Discuss endometriosis v. adenomyosis with respect to the following characteristic:
treatment |
endometriosis: pharmacologic with combination OCPs or GnRH analogs + danazol; conservative surgical management w/ excision of abnormal tissue; TAH/BSO +/- LoA
adenomyosis: NSAIDs for symptom relief, plus OCPs or progestins; endometrial ablation or resection w/ hysteroscopy; hysterectomy (definitive Tx) |
|
|
Discuss endometriosis v. adenomyosis with respect to the following characteristic:
complications |
endometriosis: infertility (MCC among menstruating women >30 years)
adenomyosis: endometrial carcinoma (rare) |
|
|
What is the provisional diagnosis for a woman with vaginal bleeding for six or more months following cessation of menstrual function?
|
cancer, until proven otherwise
|
|
|
Define the following terms:
1. menorrhagia 2. oligomenorrhea 3. polymenorrhea 4. metrorrhagia 5. menometrorrhagia |
1. incr. amount of flow (>80 mL blood loss per cycle) or prolonged bleeding (flow lasting >8 days); may lead to anemia
2. incr. length of time between menses (35-90 days) 3. frequent menstruation (<21-day cycle); anovular 4. bleeding between periods 5. excessive and irregular bleeding |
|
|
What are indications for endometrial biopsy?
|
>4mm endometrium in a postmenopausal woman
patient >35 years obese patient (BMI >35) diabetic patient |
|
|
What is the management of uterine hemorrhage?
|
high-dose IV estrogen (stabilizes endometrial lining and stops bleeding within 1h)
if bleeding not controlled within 12-24 hours, D&C is indicated |
|
|
What is the management of ovulatory bleeding?
|
NSAIDs to decrease blood loss
if patient is hemodynamically stable, treat with OCPs or a Mirena IUD to thicken endometrium and control bleeding if not effective within 24h, look for alternative diagnosis |
|
|
What is the general strategy for treating anovulatory bleeding?
|
convert proliferative endometrium to secretory endometrium
|
|
|
What is the management of anovulatory bleeding?
|
progestins x10 days to stimulate withdrawal bleeding
if young patient with suspected bleeding disorder, desmopressin followed by rapid incr. in vWF and factor VIII (lasts ~6h) |
|
|
What treatment options are available to stop uterine bleeding if medical management fails?
|
D&C
hysteroscopy (ID polyps, aid in performance of directed uterine biopsies) hysterectomy or endometrial ablation |
|
|
Define congenital adrenal hyperplasia (CAH).
|
21-hydroxylase deficiency that can present in its most severe, classic form as newborn female infant with ambiguous genitalia and life-threatening salt wasting; milder forms present later in life
11-beta-hydroxylase deficiency is a less common cause of adrenal hyperplasia |
|
|
What is the usual presentation of CAH (5)?
|
excessive hirsutism
acne amenorrhea and/or abnormal uterine bleeding infertility palpable pelvic mass (rare) |
|
|
How is CAH diagnosed?
|
incr. androgens = testosterone >2ng; DHEAS >7mcg/mL (r/o adrenal or ovarian neoplasm
incr. serum testosterone alone, suspect ovarian tumor incr. DHEAS alone, suspect adrenal source e.g. tumor, Cushing's, CAH incr. 17-OH progesterone (either basally or in response to ACTH) |
|
|
What is the prevalence and alternative name for PCOS?
|
6-10% among US women of childbearing age
Stein-Leventhal syndrome |
|
|
What criteria must be met for diagnosis of PCOS?
|
Must have two of the following three:
1. polycystic ovaries 2. oligo-/anovulation 3. clinical or biochemical evidence of hyperandrogenism |
|
|
What are the typical findings on history and physical in a patient with PCOS (3)?
|
1. high BP
2. BMI >30 3. stigmata of hyperandrogenism or insulin resistance: menstrual cycle disturbances hirsutism acne androgenic alopecia acanthosis nigricans |
|
|
What is the most severe form of PCOS?
|
HAIR-AN syndrome:
HyperAndrogenism Insulin Resistance Acanthosis Nigricans |
|
|
How is the diagnosis of PCOS made?
|
laboratory findings of incr. testosterone, DHEAS, DHEA
exclude other causes of hyperandrogenism (check TSH, prolactin, 17-OH progesterone) evaluate for metabolic abnormalities with 2h glucose tolerance test, fasting lipid panel |
|
|
What is the "pearl necklace" sign?
How common is it? |
>8 small, subcapsular ovarian follicles seen on ultrasound
found in 2/3rds of women with PCOS |
|
|
What is the ratio of LH:FSH in PCOS?
|
LH:FSH will be >2:1
|
|
|
Give the treatment of PCOS for the following:
1. women who are not attempting to conceive 2. women who ARE attempting to conceive |
1. combination of OCPs, progestin, metformin (or other insulin-sensitizing agents)
2. clomiphene +/- metformin (first-line treatment for ovulatory stimulation) |
|
|
Give the treatment for the following symptoms of PCOS:
1. hirsutism 2. CV risk factors/lipid levels |
1. combination OCPs (first-line); antiandrogens (spironolactone, finasteride) and metformin (second-line)
2. diet, weight loss, exercise +/- statin |
|
|
What are the complications of PCOS?
|
incr. risk of early-onset type 2 DM
incr. risk of miscarriages incr. long-term risk of breast, endometrial cancers due to unopposed estrogen secretion |
|
|
What is the definition of infertility?
|
inability to conceive after 12 months of normal, regular, unprotected sexual activity
|
|
|
What %of infertile couples are due to male causes; what % due to female causes?
|
male causes: 25%
female causes: 58% unexplained: 17% |
|
|
What are the four major causes of male infertility?
|
In order of descending frequency:
unknown primary hypogonadism (high FSH) disordered sperm transport secondary hypogonadism (low LH and FSH) |
|
|
What are the four major causes of female infertility?
|
In order of descending frequency:
hypothalamic/pituitary causes PCOS premature ovarian failure uterine or outflow tract disorders |
|
|
What is the presentation of vaginitis?
|
change in discharge
malodor pruritus irritation burning swelling dyspareunia dysuria |
|
|
Name two normal vaginal secretions.
|
midcycle estrogen surge: clear, elastic, mucoid secretions
luteal phase/pregnancy: thick and white secretions; adherent to vaginal wall |
|
|
What are common causes of acute pelvic pain?
|
"A ROPE"
Appendicitis Rupture ovarian cyst Ovarian torsion/abscess PID Ectopic prenancy |
|
|
What are the available outpatient regimens for treatment of PID?
|
1. ofloxacin/levofloxacin x14d +/- metronidazole x14d
2. ceftriaxone IM x1 dose 3. cefoxitin + probenecid + doxycycline x14d +/- metronidazole x14d |
|
|
What are the available inpatient regimens for treatment of PID?
|
1. cefoxitin/cefotetan + doxycycline x14d
2. clindamycin + gentamicin x14d |
|
|
What is the risk of infertility following successive eipsodes of PID?
|
1st episode: 10%
2nd episode: 25% 3rd episode: 50% |
|
|
What is the causative agent of toxic shock syndrome?
What are the presenting symptoms? |
pre-formed S. aureus toxin (TSST-1)
abrupt onset of fever, vomiting, watery diarrhea diffuse macular erythematous rash nonpurulent conjunctivitis desquamation, especially of palms and soles |
|
|
What is the treatment of toxic shock syndrome?
|
rapid rehydration
antistaphylococcal drugs (nafcillin, oxacillin; vancomycin if penicillin allergy) corticosteroids to decrease symptoms, fever manage renal or cardiac failure |
|
|
What is the mortality rate associated with toxic shock syndrome?
What are the three major causes of death? |
3-6%
ARDS intractable hypotension hemorrhage secondary to DIC |
|
|
What is the most common benign neoplasm of the female genital tract?
What is the rate of malignant transformation of these neoplasms? |
uterine leiomyoma (fibroids)
0.1-0.5% |
|
|
What is the pharmacologic treatment of uterine fibroids?
|
NSAIDs
combined OCPs medroxyprogesterone/danazol (slow or stop bleeding) GnRH analogs (decr. size of myomas, suppress further growth, decr. surrounding vascularity) |
|
|
What is the surgical treatment of uterine fibroids?
When is emergent surgery indicated? |
myomectomy or hysteroscopy with leiomyoma resection
hysterectomy for women who have completed childbearing uterine artery embolization (~25% will need further invasive Tx) for torsion of pendunculated myoma |
|
|
What health risks are associated with exposure to diethylstilbestrol (DES)?
|
for woman who took DES:
incr. risk of BRCA (~30% over general population) female offspring of women treated with DES: incr. risk of clear cell adenocarcinoma of vagina and cervix incr. risk of genital tract structural anomalies incr. risk of fertility problems |
|
|
What is the five-year overall survival for women with carcinoma of the cervix?
|
68% in Caucasians
55% in African-Americans |
|
|
Where does vaginal cancer typically present?
|
upper 1/3rd of vagina (75% of patients)
|
|
|
Give the tumor marker for the following types of ovarian tumors:
1. epithelial 2. endodermal sinus 3. embryonal carcinoma 4. choriocarcinoma 5. dysgerminoma 6. granulosa cell |
1. CA-125
2. AFP 3. AFP, hCG 4. hCG 5. LDH 6. inhibin |
|
|
What are causes of female urinary incontinence without specific urogenital pathology?
|
"DIAPPERS"
Delirium/confusional state Infection Atrophic urethritis/vaginitis Pharmaceutical Psychiatric causes (esp. depression) Excessive urinary output (hyperglycemia, hypercalcemia, CHF) Restricted mobility Stool impaction |
|
|
Describe the following types of female urinary incontinence:
1. total 2. stress 3. urge 4. overflow |
1. uncontrolled loss at all times, in all positions
2. after incr. intra-abdominal pressure e.g. sneezing, lifting 3. strong, unexpected urge to void that is unrelated to position or activity 4. chronic urinary retention |
|
|
Give the treatment for the following types of female urinary incontinence:
1. total 2. stress 3. urge 4. overflow |
1. surgery
2. Kegel exercises and pessary; vaginal vault suspension surgery 3. anticholinergic medications or TCAs; biofeedback training 4. placement of urethral catheter in acute settings; timed voiding; treat underlying disease |
|
|
What is the role of fine-needle aspiration in the evaluation of breast masses?
|
if cyst: alleviates pain and confirms cystic nature
diagnosis of fibroadenoma |
|
|
Fibrocystic change v. fibroadenoma: which changes in size during menstrual cycle?
|
fibrocystic change
as name implies, this is a condition that involves exaggerated stromal tissue response (change) to hormones and growth factors |
|
|
What % of breast cancers occur in the upper outer margin of the breast, including the axillary "tail?"
|
60%
|
|
|
What is the first step in evaluation of a suspicious breast mass?
|
depends on woman's age:
mammography in postmenopausal women or those older than 30 ultrasound in women younger than 30 |
|
|
What are tumor markers for recurrent BRCA?
|
CEA
CA15-3 CA27-29 |
|
|
What laboratory values suggest metastatic breast cancer?
|
incr. ESR
incr. alk phos (indicates liver/bone mets) incr. Ca2+ |
|
|
What is the pharmacologic treatment of breast cancer?
|
all hormone receptor positive patients should receive tamoxifen
ER negative patients should receive chemotherapy trastuzumab for HER2/neu-expressing cancers |
|
|
What are contraindications to breast-conserving surgical treatment?
|
large tumor size
subareolar location multifocal tumors fixation to chest wall involvement of nipple or overlying skin |
|
|
Give the staging criteria for breast cancer.
|
Stage I: tumor size <2cm
Stage II: tumor size 2-5 cm Stage III: axillary node involvement Stage IV: distant metastasis |

