![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
536 Cards in this Set
- Front
- Back
|
What are the characteristics of neuron regeneration?
|
Neurons are permanent cells - do not divide in adulthood and have no progenitor stem cells
|
|
|
What are the structural components of a neuron?
|
- Dendrites: receive input
- Cell bodies - Axons: send output |
|
|
How can you stain neurons?
|
Stain the Nissl substance (stains RER which is found in cell bodies and dendrites, but not in axons)
|
|
|
What happens if an axon is injured?
|
Undergoes Wallerian Degeneration:
- Degeneration distal to injury and axonal retraction proximally - Allows for potential regeneration of axon (if in PNS) |
|
|
What are the functions of astrocytes?
|
- Physical support
- Repair - K+ metabolism - Removal of excess NT - Blood-brain barrier - Glycogen fuel reserve buffer - Reactive gliosis in response to neural injury |
|
|
What is the marker of astrocytes?
|
GFAP
|
|
|
What are astrocytes derived from?
|
Neuroectoderm
|
|
|
What are the phagocytes in the CNS? Origin?
|
Microglia - originate from mesoderm
|
|
|
What is the appearance of a microglia? Stain?
|
- Not readily discernible in Nissl stains
- Have small irregular nuclei and relatively little cytoplasm |
|
|
What are the functions of microglia?
|
- Phagocytosis in CNS
- Scavenger cells - Respond to tissue damage by differentiating into large phagocytic cells - Part of the mononuclear phagocyte system |
|
|
Which type of glial cell can be infected with HIV? Implications?
|
HIV infected microglia fuse to form multi-nucleated giant cells in the CNS
|
|
|
What kinds of cells increase the conduction velocity of signals transmitted down axons?
|
Myelin:
- Oligodendrocytes (CNS) - Schwann cells (PNS) |
|
|
What is the function of myelin?
|
- ↑ conduction velocity of signals transmitted down axons
- Results in saltatory conduction of AP between nodes of Ranvier |
|
|
What are the findings of the Nodes of Ranvier?
|
High concentrations of Na+ channels
|
|
|
What kind of cell myelinates the axons of neurons in the CNS? Characteristics?
|
Oligodendroglia
- Each one can myelinate many axons (~30) |
|
|
What are oligodendroglia derived from?
|
Neuroectoderm
|
|
|
What is the appearance of oligodendroglia histologically?
|
Fried egg appearance on H&E stain
|
|
|
What diseases are associated with injury to oligodendroglia?
|
- Multiple Sclerosis
- Progressive Multifocal Leukoencephalopathy (PML) - Leukodystrophies |
|
|
What kind of cell myelinates the axons of neurons in the PNS? Characteristics?
|
Schwann Cells
- Each one can myelinate only axon |
|
|
What is the function of Schwann cells?
|
- Myelinates 1 PNS axon
- Promotes axonal regeneration - ↑ Conduction velocity via saltatory conduction between nodes of Ranvier, where there are high concentrations of Na+ channels |
|
|
What are Schwann cells derived from?
|
Neural crest
|
|
|
What diseases are associated with injury to Schwann cells?
|
- Guillain-Barré syndrome
- Acoustic Neuroma (type of Schwannoma) |
|
|
What are the characteristics of an Acoustic Neuroma? What is it associated with?
|
- Type of Schwannoma
- Typically located in internal acoustic meatus (CN VIII) - If bilateral, strongly associated with neurofibromatosis type 2 |
|
|
What are the types of sensory corpuscles?
|
- Free nerve endings
- Meissner corpuscles - Pacinian corpuscles - Merkel discs |
|
|
What sensory corpuscles are responsible for sensing pain and temperature?
|
Free Nerve Endings
- C - slow, unmyelinated fibers - Aδ - fast, myelinated fibers |
|
|
What sensory corpuscles are responsible for sensing dynamic, fine/light touch and position sense?
|
Meissner Corpuscle
- Large, myelinated fibers, adapt quickly |
|
|
What sensory corpuscles are responsible for sensing vibration and pressure?
|
Pacinian Corpuscle
- Large, myelinated fibers, adapt quickly |
|
|
What sensory corpuscles are responsible for sensing pressure, deep static touch (eg, shapes, edges), and position sense?
|
Merkel Discs
- Large, myelinated fibers, adapt slowly |
|
|
What kind of fibers have free nerve endings? Characteristics?
|
- C: slow, unmyelinated fibers
- Aδ: fast, myelinated fibers |
|
|
What kind of fibers connect to Meissner Corpuscles? Characteristics?
|
Large, myelinated fibers that adapt quickly
(same as Pacinian Corpuscle) |
|
|
What kind of fibers connect to Pacinian Corpuscles? Characteristics?
|
Large, myelinated fibers that adapt quickly
(same as Meissner Corpuscle) |
|
|
What kind of fibers connect to Merkel Discs? Characteristics?
|
Large, myelinated fibers that adapt slowly
|
|
|
What do free nerve endings sense? Location?
|
- Sense: pain and temperature
- Location: all skin, epidermis, some viscera |
|
|
What do Meissner Corpuscles sense? Location?
|
- Sense: dynamic, fine/light touch and position sense
- Location: glabrous (hairless) skin |
|
|
What do Pacinian Corpuscles sense? Location?
|
- Sense: vibration and pressure
- Location: deep skin layers, ligaments, and joints |
|
|
What do Merkel Discs sense? Location?
|
- Sense: pressure, deep static touch (eg, shapes and edges), and position sense
- Location: basal epidermal layer and hair follicles |
|
|
What layer of tissue surrounds single nerve fibers?
|
Endoneurium
|
|
|
What layer of tissue surrounds a fascicle of nerve fibers?
|
Perineurium
|
|
|
What layer of tissue surrounds the entire nerve?
|
Epineurium (dense CT) - surrounds fascicles and blood vessels)
|
|
|
Where does inflammatory infiltrate get in Guillain-Barré Syndrome?
|
Gets into endoneurium (that surrounds single nerve fiber layers)
|
|
|
What layer of tissue surrounding nerve fibers must be rejoined in microsurgery for limb reattachemnt?
|
Perineurium (surrounds a fascicle of nerve fibers)
|
|
|
Does the endoneurium, perineurium, or epineurium form the permeability barrier?
|
Perineurium
|
|
|
What are the types of NTs?
|
- Norepinephrine
- Dopamine - 5-HT - ACh - GABA |
|
|
What diseases affect the level of norepinephrine? How is it changed? Location of synthesis?
|
Norepinephrine:
- ↑ in anxiety - ↓ in depression Synthesized in locus ceruleus (pons) |
|
|
What diseases affect the level of dopamine? How is it changed? Location of synthesis?
|
Dopamine:
- ↑ in Huntington disease - ↓ in Parkinson disease - ↓ in Depression Synthesized in ventral tegmentum and SNc (substantia nigra) in midbrain |
|
|
What diseases affect the level of 5-HT? How is it changed? Location of synthesis?
|
5-HT (serotonin)
- ↑ in Parkinson Disease - ↓ in anxiety - ↓ in depression Synthesized in raphe nucleus (pons, medulla, midbrain) |
|
|
What diseases affect the level of acetylcholine? How is it changed? Location of synthesis?
|
Acetylcholine:
- ↑ in Parkinson Disease - ↓ in Alzheimer Disease - ↓ in Huntington Disease Synthesized in basal nucleus of Meynert |
|
|
What diseases affect the level of GABA? How is it changed? Location of synthesis?
|
GABA:
- ↓ in anxiety - ↓ in Huntington disease Synthesized in nucleus accumbens |
|
|
What NTs are altered in anxiety? Location of synthesis?
|
- ↑ NE (locus ceruleus, pons)
- ↓ 5-HT (raphe nucleus - pons, medulla, midbrain) - ↓ GABA (nucleus accumbens) |
|
|
What NTs are altered in depression? Location of synthesis?
|
- ↓ NE (locus ceruleus, pons)
- ↓ Dopamine (ventral tegmentum and SNc - midbrain) - ↓ 5-HT (raphe nucleus - pons, medulla, midbrain) |
|
|
What NTs are altered in Huntington Disease? Location of synthesis?
|
- ↑ Dopamine (ventral tegmentum and SNc - midbrain)
- ↓ ACh (basal nucleus of Meynert) - ↓ GABA (nucleus accumbens) |
|
|
What NTs are altered in Parkinson Disease? Location of synthesis?
|
- ↓ Dopamine (ventral tegmentum and SNc - midbrain)
- ↑ 5-HT (raphe nucleus - pons, medulla, midbrain) - ↑ ACh (basal nucleus of Meynert) |
|
|
What NTs are altered in Alzheimer Disease? Location of synthesis?
|
↓ ACh (basal nucleus of Meynert)
|
|
|
What functions does the locus ceruleus mediate? What NT does it synthesize?
|
Stress and panic - mediated via NE
|
|
|
What functions does the nucleus accumbens and septal nucleus mediate? What NT does it synthesize?
|
- Reward enter, pleasure, addiction, fear
- Mediated via GABA |
|
|
What structures mediate the blood brain barrier?
|
- Tight junctions between non-fenestrated capillary endothelial cells
- Basement membrane - Astrocyte foot processes |
|
|
What is the function of the blood brain barrier?
|
- Prevents circulating blood substances from reaching the CSF / CNS
- Helps prevent bacterial infection from spreading into the CNS - Also restricts drug delivery to brain |
|
|
What crosses the blood brain barrier slowly?
|
Glucose and amino acids cross slowly via carrier-mediated transport mechanism
|
|
|
What crosses the blood brain barrier quickly?
|
Non-polar / lipid-soluble substances cross rapidly via diffusion
|
|
|
What specialized brain regions have fenestrated capillaries and no blood-brain barrier? Effect?
|
Allows molecules in the blood to affect brain function:
- Area postrema → vomiting after chemo - OVLT → osmotic sensing Allows neurosecretory products to enter the circulation: - Neurohypophysis → ADH release |
|
|
Besides the blood brain barrier, what are the other notable barriers?
|
- Blood-testis barrier
- Maternal-fetal blood barrier of placenta |
|
|
What can cause vasogenic edema in the brain?
|
Infarction and/or neoplasm that destroys the endothelial cell tight junctions
|
|
|
What inputs and outputs permeate the blood brain barrier?
|
Hypothalamic inputs and outputs
|
|
|
What does the hypothalamus control?
|
TAN HATS:
- Thirst and water balance - Adenohypophysis control (regulates anterior pituitary) - Neurohypophysis releases hormones produced by hypothalamus - Hunger - Autonomic regulation - Temperature regulation - Sexual urges |
|
|
What inputs to the hypothalamus are not protected by the blood brain barrier?
|
- OVLT (organum vasculosum of the lamina terminalis) - senses changes in osmolarity
- Area Postrema - responds to emetics |
|
|
Where is ADH made?
|
Supraoptic nucleus of the hypothalamus
|
|
|
Where is oxytocin made?
|
Paraventricular nucleus of the hypothalamus
|
|
|
Where are ADH and oxytocin stored and released from?
|
Posterior pituitary
|
|
|
What are the areas of the hypothalamus with specific functions?
|
- Lateral area
- Ventromedial area - Anterior hypothalamus - Posterior hypothalamus - Suprachiasmatic nucleus |
|
|
Which part of the brain is responsible for telling you you're hungry?
|
Lateral area of hypothalamus
|
|
|
Which part of the brain is responsible for telling you you're full (satiated)?
|
Ventromedial area of hypothalamus
|
|
|
Which part of the brain is responsible for cooling you down?
|
Anterior hypothalamus
|
|
|
Which part of the brain is responsible for warming you up?
|
Posterior hypothalamus
|
|
|
Which part of the brain is responsible for the Circadian rhythm?
|
Suprachiasmatic nucleus of hypothalamus
|
|
|
What happens if you destroy the lateral area of the hypothalamus?
|
Anorexia, failure to thrive (infants)
"If you zap your lateral nucleus, you shrink laterally" |
|
|
What happens if you destroy the ventromedial area of the hypothalamus?
|
Hyperphagia (can be destroyed by craniopharyngioma)
"If you zap your ventromedial nucleus, you grow ventrally and medially" |
|
|
What are the actions of leptin?
|
- Leptin inhibits the lateral nucleus of the hypothalamus (prevents you from feeling hungry)
- Leptin stimulates the ventromedial nucleus of the hypothalamus (makes you feel satiated) |
|
|
A craniopharyngioma can destroy what part of the hypothalamus? Implications?
|
Can destroy the ventromedial nucleus of the hypothalamus → hyperphagia (gain weight)
|
|
|
What controls the anterior hypothalamus and posterior hypothalamus?
|
- Anterior: parasympathetic (cools you down)
- Posterior: sympathetic (heats you up) |
|
|
What happens if you damage your posterior hypothalamus?
|
Become a "Poikilotherm" = cold-blooded, like a snake
|
|
|
What hormones are controlled by the Circadian rhythm?
|
Nocturnal release of:
- ACTH - Prolactin - Melatonin - Norepinephrine Suprachiasmatic Nucleus → NE release → pineal gland → melatonin |
|
|
What regulates the Suprachiasmatic Nucleus (SCN)?
|
Environment (eg, light)
|
|
|
What are the stages of sleep?
|
- Rapid Eye Movement (REM)
- Non-REM |
|
|
What controls the movement of eyes during REM sleep?
|
Extraocular movements due to activity of PPRF (paramedian pontine reticular formation / conjugate gaze center)
|
|
|
How often does REM sleep occur? How long is it relatively during the night?
|
- REM occurs every 90 minutes
- Duration ↑ throughout night |
|
|
What drugs decrease REM sleep and delta wave sleep?
|
- Alcohol
- Benzodiazepines - Barbiturates - Norepinephrine |
|
|
What drugs can be used to treat bed-wetting?
|
- Oral desmopressin acetate (DDAVP) - mimics ADH
- Imipramine (less optimal due to adverse effects) |
|
|
What drugs can be used to treat night terrors and sleepwalking?
|
Benzodiazepines
|
|
|
What EEG waveform is characteristic of being awake with eyes open?
|
Beta (highest frequency, lowest amplitude)
|
|
|
What EEG waveform is characteristic of being awake with eyes closed?
|
Alpha waves
|
|
|
What EEG waveform is characteristic of stage N1 (light sleep)?
|
Theta waves
|
|
|
What EEG waveform is characteristic of stage N2 (deeper sleep)?
|
Sleep spindles and K complexes
|
|
|
What EEG waveform is characteristic of the stage N3 (deepest non-REM sleep)?
|
Delta (lowest frequency, highest amplitude)
|
|
|
What EEG waveform is characteristic of REM sleep?
|
Beta waves (like in awake with eyes open stage)
|
|
|
How much of your sleep is spent in each stage of sleep?
|
- Stage 1: 5%
- Stage 2: 45% - Stage 3: 25% - REM sleep: 25% |
|
|
During which stage of sleep does bruxism (teeth grinding) occur?
|
Stage N2
|
|
|
During which stage of sleep does sleepwalking occur?
|
Stage N3
|
|
|
During which stage of sleep do night terrors occur?
|
Stage N3
|
|
|
During which stage of sleep does bedwetting occur?
|
Stage N3
|
|
|
During which stage of sleep does dreaming occur?
|
REM sleep
|
|
|
During which stage of sleep does penile and clitoral tumescence occur?
|
REM sleep
|
|
|
What happens to your brain and body during REM sleep?
|
- Loss of motor tone
- ↑ brain O2 use - ↑ and variable HR and BP - May serve a memory processing function |
|
|
What does the posterior pituitary (neurohypophysis) receive inputs from?
|
Receives hypothalamic axonal projections from supraoptic (ADH) and paraventricular (oxytocin) nuclei
|
|
|
What is the function of the thalamus?
|
Major relay for all ascending sensory information (except olfaction)
|
|
|
What are the nuclei of the thalamus?
|
- VPL
- VPM - LGN - MGN - VL |
|
|
What information is relayed through the VPL nucleus of the thalamus?
|
- Pain and temperature
- Pressure, touch, vibration, and proprioception |
|
|
What information is relayed through the VPM nucleus of the thalamus?
|
Face sensation and taste
|
|
|
What information is relayed through the LGN nucleus of the thalamus?
|
Vision
|
|
|
What information is relayed through the MGN nucleus of the thalamus?
|
Hearing
|
|
|
What information is relayed through the VL nucleus of the thalamus?
|
Motor
|
|
|
Pain and temperature information travels on what tracts? Through what nucleus of the thalamus? Destination?
|
- Spinothalamic tract →
- VPL nucleus → - 1° Somatosensory Cortex |
|
|
Pressure, touch, vibration, and proprioception information travels on what tracts? Through what nucleus of the thalamus? Destination?
|
- Dorsal columns / Medial lemniscus →
- VPL nucleus → - 1° Somatosensory Cortex |
|
|
Face sensation information travels on what tracts? Through what nucleus of the thalamus? Destination?
|
- Trigeminal nerve →
- VPM nucleus → - 1° Somatosensory Cortex |
|
|
Taste information travels on what tracts? Through what nucleus of the thalamus? Destination?
|
- Gustatory pathway →
- VPM nucleus → - 1° Somatosensory Cortex |
|
|
Visual information travels on what tracts? Through what nucleus of the thalamus? Destination?
|
- CN II →
- LGN nucleus - Calcarine sulcus |
|
|
Auditory information travels on what tracts? Through what nucleus of the thalamus? Destination?
|
- Superior olive and inferior colliculus of tectum →
- MGN nucleus → - Auditory cortex of temporal lobe |
|
|
Motor information travels on what tracts? Through what nucleus of the thalamus? Destination?
|
- Basal ganglia and cerebellum →
- VL nucleus → - Motor cortex |
|
|
What does the limbic system control?
|
- Emotion
- Long-term memory - Olfaction - Behavior modulation - Autonomic nervous system function |
|
|
What structures are apart of the limbic system?
|
- Hippocampus
- Amygdala - Fornix - Mammillary bodies - Cingulate gyrus |
|
|
What are the functions of the limbic system?
|
5 F's:
- Feeding - Fleeing - Fighting - Feeling - Fornication (sex) |
|
|
What does the cerebellum control?
|
- Modulates movement
- Aids in coordination and balance |
|
|
What are the inputs to the cerebellum?
|
- Contralateral cortex via middle cerebellar peduncle
- Ipsilateral proprioceptive information via inferior cerebellar peduncle from the spinal cord (input nerves = climbing and mossy fibers) |
|
|
What are the outputs from the cerebellum?
|
- Sends information to contralateral cortex to modulate movement
- Output nerves = Purkinje cells → deep nuclei of cerebellum → contralateral cortex via superior cerebellar peduncle - Deep nuclei (lateral → medial): Dentate, Emboliform, Globose, Fastigial |
|
|
What is the path along which information from the cerebellum is sent to the contralateral cortex to modulate movement?
|
Purkinje cells → deep nuclei of cerebellum → contralateral cortex via the superior cerebellar peduncle
|
|
|
What are the deep nuclei of the cerebellum (from lateral to medial)?
|
From lateral → medial:
"Don't Eat Greasty Foods" - Dentate - Emboliform - Globose - Fastigial |
|
|
What are the implications of lateral lesions to the cerebellum?
|
Propensity to fall toward injured (ipsilateral side) - problem with voluntary movement of extremities
|
|
|
What are the implications of medial lesions to the cerebellum?
|
Generally bilateral motor deficits affecting axial and proximal limb musculature:
- Truncal ataxia - Nystagmus - Head tilting - Wide-based gait - Deficits in truncal coordination |
|
|
Lesions to what structures can lead towards a propensity to fall to one side?
|
Injury to lateral structures in cerebellum on same side as they are falling towards
|
|
|
Lesions to what structures can lead to truncal ataxia, nystagmus, and head tilting?
|
Lesions to midline structures of the cerebellum (vermal cortex, fastigial nuclei) and/or the flocconodular lobe
|
|
|
The basal ganglia is important for what functions?
|
Voluntary movements and making postural adjustments
|
|
|
What does the basal ganglia receive input from? How does it respond?
|
Receives cortical input and provides negative feedback to cortex to modulate movement
|
|
|
What are the components of the striatum in the basal ganglia?
|
Putamen (motor) + Caudate (cognitive)
|
|
|
What are the components of the lentiform nucleus in the basal ganglia?
|
Putamen + Globus Pallidus
|
|
|
What are the areas of the Basal Ganglia?
|
- SNc: Substantia Nigra pars Compacta
- GPe: Globus Pallidus externus - GPi: Globus Pallidus internus - STN: Subthalamic Nucleus - Putamen - Caudate |
|
|
What pathways pass through the substantia nigra? Functions?
|
Dopamine can bind to:
- Direct pathway: D1 receptor → stimulates excitatory pathway - Indirect pathway: D2 receptor → inhibits inhibitory pathway Both lead to ↑ motion |
|
|
What happens on the excitatory pathway through the basal ganglia? Effect?
|
- Cortical inputs stimulate the striatum
- Stimulates release of GABA - Disinhibits thalamus vis the GPi/SNr - ↑ Motion |
|
|
What happens on the inhibitory pathway through the basal ganglia? Effect?
|
- Cortical inputs stimulate the striatum
- Disinhibits STN via GPe - STN stimulates GPi/SNr - Inhibits thalamus - ↓ Motion |
|
|
What kind of disorder is Parkinson Disease? What accumulates to mediate the pathology?
|
- Degenerative disorder of CNS
- Accumulation of Lewy bodies and loss of dopaminergic neurons in SNc |
|
|
What are Lewy bodies?
|
Composed of α-synuclein - intracellular eosinophilic inclusions
Associated with Parkinson disease |
|
|
What happens to the substantia nigra pars compacta (SNc) in Parkinson disease?
|
Loss of dopaminergic neurons in this area → depigmentation
|
|
|
What are the signs/symptoms of Parkinson disease?
|
Parkinson TRAPS your body:
- Tremor (at rest - eg, pill-rolling tremor) - Rigidity (cogwheel) - Akinesia (or bradykinesia) - Postural instability - Shuffling gait |
|
|
What is the cause of Huntington disease?
|
- Autosomal dominant
- Trinucleotide repeat disorder on chromosome 4: CAG repeats - Caudate loses ACh and GABA (CAG) |
|
|
When and how does Huntington disease present?
|
- Between ages 20-50 (appears earlier in successive generations)
- Symptoms: choreiform movements, aggression, depression, dementia |
|
|
What can Huntington disease sometimes be mistaken for initially?
|
Substance abuse (aggression, depression, dementia)
|
|
|
What NT changes occur in Huntington disease?
|
↓ levels of GABA and ACh in the Caudate
|
|
|
What happens to neurons in Huntington disease? Mechanism?
|
- Neuronal death via NMDA-R binding and glutamate toxicity
- Atrophy of caudate nuclei can be seen on imaging |
|
|
What are the types of movement disorders?
|
- Hemiballismus
- Chorea - Athetosis - Myoclonus - Dystonia - Essential tremor (postural tremor) - Resting tremor - Intention tremor |
|
|
What would you call sudden, wild flailing of one arm +/- the ipsilateral leg? Characteristic lesion?
|
Hemiballismus
- Lesion to contralateral subthalamic nucleus (eg, lacunar stroke) |
|
|
What would you call sudden, jerky, purposeless movements? Characteristic lesion?
|
Chorea
- Lesion to basal ganglia (eg, Huntington disease) |
|
|
What would you call slow, writhing movements, especially seen in fingers? Characteristic lesion?
|
Athetosis
- lesion to basal ganglia (eg, Huntington disease) |
|
|
What would you call sudden, brief, uncontrolled muscle contraction? Specific examples? Characteristic cause?
|
Myoclonus
- Jerks or hiccups - Common in metabolic abnormalities such as renal and liver failure |
|
|
What would you call sustained, involuntary muscle contractions? Specific examples?
|
Dystonia
- Writer's cramp - Blepharospasm (sustained eyelid twitch) |
|
|
What would you call a tremor that is exacerbated by holding a posture or limb position? Cause?
|
Essential Tremor (Postural Tremor)
- Occurs while moving - Genetic predisposition - Patients often self-medicated with EtOH, which ↓ tremor amplitude |
|
|
How can you treat/prevent tremors that are exacerbated by holding a posture of limb position?
|
Essential Tremor (Postural Tremor)
- Treatment: β-blockers and Primidone - Patients often self-medicated with EtOH, which ↓ tremor amplitude |
|
|
What would you call an uncontrolled movement of distal appendages (most noticeable in hands) that is relieved by intentional movement? Specific example? Cause?
|
Resting Tremor
- Occurs at rest, "pill-rolling tremor" - Seen in Parkinson Disease |
|
|
What would you call a slow, zigzag motion when pointing / extending toward a target? Characteristic lesion?
|
Intention Tremor
- Cerebellar dysfunction |
|
|
What are the three types of tremors? How do they differ?
|
Essential Tremor (Postural Tremor)
- Action tremor, exacerbated by holding a posture / limb position Resting Tremor - Uncontrolled movement when at rest, eg, pill-rolling tremor Intention Tremor - Slow, zigzag motion when pointing/extending toward a target |
|
|
What important areas are in the frontal component of the cerebral cortex?
|
- Principal motor area
- Premotor area (part of extrapyramidal circuit) - Frontal eye fields - Motor speech: Broca's area - Frontal association areas |
|
|
What important areas are in the parietal component of the cerebral cortex?
|
- Principal sensory area
- Arcuate fasciculus |
|
|
What important areas are in the temporal component of the cerebral cortex?
|
- Primary auditory cortex
- Associative auditory cortex: Wernicke area |
|
|
What important areas are in the occipital component of the cerebral cortex?
|
Principal visual cortex
|
|
|
Describe the layout of the homunculus?
|
- Leg is most medial along longitudinal fissure
- Arm is most superior - Face is most lateral Distorted appearance is due to certain body regions that are more richly innervated and thus have ↑ cortical representation |
|
|
What syndrome is associated with hyperorality, hypersexuality, and disinhibited behavior? What lesion is it associated with?
|
Klüver-Bucy Syndrome
- Lesion in amygdala (bilateral) - associated with HSV-1 |
|
|
What lesion is associated with disinhibition and deficits in concentration, orientation, and judgment?
|
Lesion to frontal lobe
|
|
|
What lesion is associated with reemergence of primitive reflexes?
|
Lesion to frontal lobe
|
|
|
What lesion is associated with spatial neglect syndrome (ignoring the contralateral side of the world)?
|
Lesion to right parietal-temporal cortex
|
|
|
What lesion is associated with agraphia, acalculia, finger agnosia, and left-right disorientation?
|
Gerstmann Syndrome
- Lesion to left parietal-temporal cortex |
|
|
What lesion is associated with reduced levels of arousal and wakefulness (eg, coma)?
|
Lesion to reticular activating system in midbrain
|
|
|
What syndrome and lesion is associated with confusion, opthalmoplegia, ataxia, memory loss (anterograde and retrograde amnseia), confabulation, and personality changes?
|
Wernicke-Korsakoff syndrome
- Lesion to mammillary bodies (bilateral) due to thiamine (B1) deficiency and excessive EtOH use - Can be precipitated by giving glucose without B1 to a B1-deficient patient |
|
|
What lesion is associated with tremor at rest, chorea, or athetosis?
|
Lesions to basal ganglia
- Eg, Parkinson disease |
|
|
What lesion is associated with intention tremor, limb ataxia, and loss of balance?
|
Lesion to ipsilateral cerebellar hemisphere (lateral)
- Fall towards side of lesion |
|
|
What lesion is associated with truncal ataxia and dysarthria (difficult or unclear articulation of speech)?
|
Lesion to cerebellar vermis (centrally located)
|
|
|
What lesion is associated with hemiballismus (flailing limb(s) on one side of body)?
|
Lesion to contralateral subthalamic nucleus
|
|
|
What lesion is associated with anterograde amnesia (inability to make new memories)?
|
Lesion to hippocampus (bilateral)
|
|
|
What lesion is associated with eyes that look away from the side of the lesion?
|
Lesion of paramedian pontine reticular formation (looking away from the side injured)
|
|
|
What lesion is associated with eyes that look towards the side of the lesion?
|
Lesion of frontal eye fields (looking at side injured)
|
|
|
What injury is associated with "locked in syndrome" that causes acute paralysis, dysarthria, dysphagia, diplopia, and loss of consciousness?
|
Central Pontine Myelinolysis
- Due to massive axonal demyelination in pontine white matter tracts - Can be due to osmotic forces and edema - Commonly iatrogenic due to overly rapid correction of hyponatremia |
|
|
What can happen if you correct a low serum Na+ too quickly?
|
From low to high, your pons will die (central pontine myelinolyis = locked in syndrome)
|
|
|
What can happen if you correct a high serum Na+ too quickly?
|
From high to low, your brain will blow (cerebral edema / herniation)
|
|
|
What are the symptoms of Central Pontine Myelinolysis?
|
- Acute paralysis
- Dysarthria - Dysphagia - Diplopia - Loss of consciousness Can caused locked in syndrome |
|
|
What is the term for a higher order inability to speak (language defecit)?
|
Aphasia
|
|
|
What is term for a motor inability to speak (movement deficit)?
|
Dysathria
|
|
|
What are the types of aphasia (language deficit)?
|
- Broca
- Wernicke - Global - Conduction - Transcortical motor - Transcortical sensory - Mixed transcortical |
|
|
What is the name for the deficit that causes non-fluent aphasia with intact comprehension?
|
Broca Aphasia
- Deficit in inferior frontal gyrus of frontal lobe |
|
|
What is the name for the deficit that causes fluent aphasia with impaired comprehension and repetition?
|
Wernicke Aphasia (Wernicke is wordy but makes no sense)
- Deficit in superior temporal gyrus of temporal lobe |
|
|
What is the name for the deficit that causes non-fluent aphasia with impaired comprehension?
|
Global Aphasia
- Both Broca and Wernicke areas are affected |
|
|
What is the name for the deficit that causes poor repetition but fluent speech with intact comprehension?
|
Conduction Aphasia
- Can be due to damage to left superior temporal lobe and/or left supramarginal gyrus (Can't repeat phrases such as "no ifs, ands, or buts") |
|
|
What is the name for the deficit that causes non-fluent aphasia with good comprehension and repetition?
|
Transcortical Motor Aphasia
|
|
|
What is the name for the deficit that causes poor comprehension with fluent speech and repetition?
|
Transcortical Sensory Aphasia
|
|
|
What is the name for the deficit that causes non-fluent speech, poor comprehension, but good repetition?
|
Mixed Transcortical Aphasia
|
|
|
What deficit occurs with Broca Aphasia? What language capabilities are intact?
|
- Non-fluent speech
- Intact comprehension |
|
|
What deficit occurs with Wernicke Aphasia? What language capabilities are intact?
|
- Impaired comprehension
- Impaired repetition - Fluent speech |
|
|
What deficit occurs with Global Aphasia? What language capabilities are intact?
|
- Non-fluent speech
- Impaired comprehension |
|
|
What deficit occurs with Conduction Aphasia? What language capabilities are intact?
|
- Poor repetition
- Fluent speech - Intact comprehension |
|
|
What deficit occurs with Transcortical Motor Aphasia? What language capabilities are intact?
|
- Non-fluent speech
- Intact comprehension - Intact repetition |
|
|
What deficit occurs with Transcortical Sensory Aphasia? What language capabilities are intact?
|
- Poor comprehension
- Fluent speech - Intact repetition |
|
|
What deficit occurs with Mixed Transcortical Aphasia? What language capabilities are intact?
|
- Non-fluent speech
- Poor comprehension - Intact repetition |
|
|
What are the components of the Circle of Willis?
|
- Internal Carotid Arteries
- Anterior Cerebral Arteries (connected by Anterior Communicating Artery) - Posterior Cerebral Arteries (connected to ICA by Posterior Communicating Arteries) |
|
|
What are the branches of the Vertebral Arteries?
|
Inferior to Superior:
- Posterior Inferior Cerebellar Arteries (PICA) - Anterior Spinal Artery (ASA) - Anterior Inferior Cerebellar Arteries (AICA) Combine to form Basilar Artery |
|
|
What are the branches of the Basilar Artery?
|
Inferior to Superior:
- Pontine Arteries - Superior Cerebellar Arteries (SCA) - Posterior Cerebral Arteries (PCA) |
|
|
What is the system of anastomoses between the anterior and posterior blood supplies to the brain?
|
Circle of Willis
|
|
|
What part of the brain is supplied by the Anterior Cerebral Arteries?
|
Anteromedial surface of brain
|
|
|
What part of the brain is supplied by the Middle Cerebral Arteries?
|
Lateral surfaces of brain
|
|
|
What part of the brain is supplied by the Posterior Cerebral Arteries?
|
Posterior and Inferior surfaces of brain
|
|
|
What are the Watershed Zones? What are they susceptible to?
|
- Between anterior cerebral / middle cerebral and middle cerebral / posterior cerebral arteries
- Damage caused by severe hypotension → upper leg/upper arm weakness, defects in higher order visual processing |
|
|
What regulates brain perfusion?
|
Tight auto-regulation
- Primarily driven by PCO2 - PO2 also modulates perfusion in severe hypoxia |
|
|
What can cause increased intracranial pressure? How can you decrease this by using the principles of cerebral perfusion regulation?
|
Caused by acute cerebral edema (stroke, trauma)
Therapeutic Hyperventilation → ↓ PCO2 → vasoconstriction → ↓ cerebral perfusion |
|
|
How does PO2 affect cerebral perfusion?
|
Hypoxemia only increases cerebral perfusion when PO2 <50 mmHg
(Normal: ~100 mmHg) |
|
|
How does PCO2 affect cerebral perfusion?
|
Hypercapnia stimulates cerebral perfusion when PCO2 > 90 mmHg
(Normal: ~40 mmHg) |
|
|
What are the effects of a stroke in the MCA?
|
- Contralateral paralysis - upper limb and face (motor cortex deficit)
- Contralateral loss of sensation - upper and lower limbs and face (sensory cortex deficit) - Aphasia if in dominant (usually left) hemisphere - Hemineglect if in non-dominant (usually right) hemisphere |
|
|
What are the effects of a stroke in the ACA?
|
- Contralateral paralysis - lower limb (motor cortex deficit)
- Contralateral loss of sensation - lower limb (sensory cortex deficit) |
|
|
What are the effects of a stroke in the Lenticulostriate Artery?
|
- Contralateral hemiparesis / hemiplegia (deficit in striatum or internal capsule)
- Common location of lacunar infarcts, 2° to unmanaged hypertension |
|
|
What are the effects of a stroke in the ASA?
|
- Contralateral hemiparesis - upper and lower limbs (deficit in lateral corticospinal tract)
- ↓ Contralateral proprioception (deficit in medial lemniscus) - Ipsilateral hypoglossal dysfunction - tongue deviates ipsilaterally (deficit in caudal medulla / hypoglossal nerve) |
|
|
What are the effects of a stroke in the PICA?
|
Deficit in lateral medulla:
- Vomiting, vertigo, nystagmus - ↓ Pain and temperature sensation from ipsilateral face and contralateral body - Dysphagia, hoarseness, ↓ gag reflex - Ipsilateral Horner syndrome - Ataxia and dysmetria (lack of coordination) |
|
|
What are the effects of a stroke in the AICA?
|
Deficit in Lateral Pons:
- Vomiting, vertigo, nystagmus - Paralysis of face - ↓ Lacrimation, salivation - ↓ Taste from anterior 2/3 of tongue - ↓ Corneal reflex - Face: ↓ pain and temperature sensation - Ipsilateral ↓ hearing - Ipsilateral Horner syndrome Deficit in Middle and Inferior Cerebellar Peduncles - Ataxia and dysmetria (lack of coordination) |
|
|
What are the effects of a stroke in the PCA?
|
Deficit in occipital cortex and visual cortex
- Contralateral hemianopia with macular sparing |
|
|
What are the effects of a stroke in the Basilar Artery?
|
Deficits to Pons, Medulla, Lower Midbrain, Corticospinal and Corticobulbar Tracts, Ocular CN nuclei, Paramedian Pontine Reticular Formation:
- Preserved consciousness and blinking - Quadriplegia - Loss of voluntary facial, mouth, and tongue movements |
|
|
What are the effects of a stroke in the Anterior Communicating Artery?
|
- Visual field defects
- Commonly due to aneurysm |
|
|
What are the effects of a stroke in the Posterior Communicating Artery?
|
- CN III palsy - eye is "down and out" with ptosis and pupil dilation
- Lesion is commonly due to saccular aneurysm |
|
|
What areas are lesioned in an MCA stroke?
|
- Motor cortex: upper limb and face
- Sensory cortex: upper limb and face - Temporal lobe (Wernicke area possibly) - Frontal lobe (Broca area possibly) |
|
|
What areas are lesioned in an ACA stroke?
|
- Motor cortex: lower limb
- Sensory cortex: lower limb |
|
|
What areas are lesioned in a Lenticulostriate artery stroke? Common cause?
|
- Striatum
- Internal Capsule Common location of lacunar infarct, 2° to unmanaged hypertension |
|
|
What areas are lesioned in an ASA stroke?
|
- Lateral corticospinal tract
- Medial lemniscus - Caudal medulla / hypoglossal nerve |
|
|
What areas are lesioned in a PICA stroke?
|
Lateral Medulla:
- Vestibular nuclei - Lateral spinothalamic tract - Spinal trigeminal nucleus - Nucleus ambiguus - Sympathetic fibers - Inferior cerebellar peduncle |
|
|
What areas are lesioned in an AICA stroke?
|
Lateral Pons:
- Cranial nerve nuclei - Vestibular nuclei - Facial nucleus - Spinal trigeminal nucleus - Cochlear nuclei - Sympathetic fibers Middle and inferior cerebellar peduncles |
|
|
What areas are lesioned in a PCA stroke?
|
- Occipital cortex
- Visual cortex |
|
|
What areas are lesioned in a Basilar Artery stroke?
|
- Pons, medulla, lower midbrain
- Corticospinal and corticobulbar tracts - Ocular cranial nerve nuclei - Paramedian pontine reticular formation |
|
|
What is a common location of a lacunar infarct? Effect?
|
Lenticulostriate artery
- Lesions striatum and internal capsule - Causes contralateral hemiparesis and hemiplegia |
|
|
What causes Medial Medullary Syndrome? Effects?
|
- Caused by infarct of paramedian branches of ASA and vertebral arteries (commonly bilaterally)
- Lesions lateral corticospinal tract → contralateral hemiparesis (upper and lower limbs) - Lesions medial lemniscus → ↓ contralateral proprioception - Lesions caudal medulla and hypoglossal nerve → ipsilateral hypoglossal dysfunction (tongue deviates ipsilaterally) |
|
|
What causes Lateral Medullary (Wallenberg) Syndrome? Effects?
|
Stroke in PICA
* Nucleus ambiguus effects are specific for PICA lesion * Dysphagia and hoarseness - Vomiting, vertigo, nystagmus - ↓ Pain and temperature sensation from ipsilateral face and contralateral body - ↓ Gag reflex - Ipsilateral Horner syndrome - Ataxia and dysmetria "Don't pick a (PICA) horse (hoaraseness) that can't eat (dysphagia)" |
|
|
What causes Lateral Pontine Syndrome? Effects?
|
Stroke in AICA
* Facial nucleus effects are specific to AICA lesions * Paralysis of face "Facial droops means AICA's pooped" |
|
|
A stroke in what artery will caused "locked in syndrome"?
|
Basilar Artery
|
|
|
Where does a Berry Aneurysm occur?
|
Bifurcations in the Circle of Willis
- Most common site: Anterior Communicating Artery and Anterior Cerebral Artery |
|
|
What are the most common complications of a Berry Aneurysm?
|
- Rupture → subarachnoid hemorrhage → worse headache of life
- Hemorrhagic stroke - Bitemporal hemianopia via compression of optic chiasm |
|
|
What is a Berry aneurysm associated with?
|
- ADPKD
- Ehlers Danlos Syndrome - Marfan Syndrome - Advanced age - Hypertension - Smoking - Race (↑ in blacks) |
|
|
What is a Charcot-Bouchard Microaneurysm associated with? What does it affect?
|
- Chronic hypertension
- Affects small vessels (eg, in basal ganglia and thalamus) |
|
|
What sensations can occur post-stroke?
|
Central Post-Stroke Pain Syndrome
- Neuropathic pain due to thalamic lesions - Initial sensation of numbness and tingling following in weeks to months by allodynia (ordinarily painless stimuli cause pain) - Dysaesthesia |
|
|
What is the syndrome that causes neuropathic pain after a stroke? How common?
|
Central Post-Stroke Pain Syndrome - occurs in 10%o f stroke patients
|
|
|
What are the types of intracranial hemorrhages?
|
- Epidural hematoma
- Subdural hematoma - Subarachnoic hemorrhage - Intraparenchymal (hypertensive) hemorrhage |
|
|
What kind of injury can occur if the temporal bone is fractured?
|
Rupture of middle meningeal artery (branch of maxillary artery) → Epidural Hematoma
|
|
|
What are the characteristics of a middle meningeal artery bleed?
|
Epidural Hematoma
- Lucid interval - Rapid expansion under systemic arterial pressure - Can cause transtentorial herniation, CN III palsy - CT shows biconvex (lentiform), hyperdense blood collection - Can NOT cross suture lines - Can cross falx and tentorium |
|
|
What kind of injury can occur if the bridging veins are ruptured? Characteristics of bleed?
|
- Slow venous bleeding (less pressure → hematoma develops over time)
- Crescent-shaped hemorrhage - Can cause midline shift - Can cross suture lines - Can NOT cross falk or tentorium |
|
|
What is more likely to get a subdural hematoma? Predisposing factors?
|
- Elderly
- Alcoholics - Blunt trauma - Shaken baby Predisposing factors: - Brain atrophy - Shaking - Whiplash |
|
|
Which type of hematoma can cross suture lines?
|
Subdural Hematoma
|
|
|
Which type of hematoma can cross the falx and tentorium?
|
Epidural Hematoma
|
|
|
Which type of brain bleed can be caused by the rupture of an aneurysm? What is this associated with?
|
Subarachnoid Hemorrhage
- Berry aneurysm associated with Marfan, Ehlers-Danlos, and ADPKD |
|
|
What can cause a Subarachnoid Hemorrhage?
|
- Berry aneurysm: associated with Marfan, Ehlers-Danlos, and ADPKD
- Atrioventricular malformation (AVM) |
|
|
What are the symptoms of a Subarachnoid Hemorrhage?
|
- Rapid time course
- "Worst headache of my life" |
|
|
On what type of brain bleed would you expect to see a bloody or yellow (xanthochromic) spinal tap?
|
Subarachnoid Hemorrhage
|
|
|
What are the potential complications of Subarachnoid Hemorrhage? Appearance on CT? Treatment?
|
- 2-3 days afterword risk of vasospasm due to blood breakdown (not visible on CT, treat with nimodipine)
- Rebleed possible (visible on CT) |
|
|
What type of brain bleed is commonly caused by systemic hypertension?
|
Intraparenchymal Hemorrhage
|
|
|
What can cause an Intraparenchymal Hemorrhage?
|
- Systemic hypertension
- Amyloid angiopathy - Vasculitis - Neoplasm |
|
|
Where do Intraparenchymal Hemorrhages usually occur?
|
- Typically occurs in basal ganglia and internal capsule (Charcot-Bouchard aneurysm of lenticulostriate vessels)
- Can be lobar |
|
|
How long does hypoxia have to occur to cause irreversible damage? Implications?
|
>5 minutes → irreversible neuronal injury
|
|
|
What areas of the brain are most vulnerable to hypoxia?
|
- Hippocampus
- Neocortex - Cerebellum - Watershed areas |
|
|
What is the appearance of an ischemic brain stroke on imaging?
|
- Diffusion weighted MRI: bright
- Non-contrast CT: dark (hemorrhage appears bright) |
|
|
How can you detect an ischemic stroke early on?
|
Bright on diffusion-weighted MRI from 3-30 minutes after stroke (highest sensitivity for early ischemia)
|
|
|
How can you detect an ischemic stroke later on?
|
Dark abnormality on non-contrast CT from 12-24 hours after stroke
|
|
|
Why do you need to do a CT for a patient you suspect of having a stroke if it doesn't show ischemia for 12-24 hours?
|
Non-contrast CT will show bright area if there is a hemorrhage; if there is a hemorrhage you can't give tPA for ischemia
|
|
|
What are the histologic signs of an ischemic stroke 12-48 hours after it occurs?
|
Red neurons
|
|
|
What are the histologic signs of an ischemic stroke 24-72 hours after it occurs?
|
Necrosis and neutrophils
|
|
|
What are the histologic signs of an ischemic stroke 3-5 days after it occurs?
|
Macrophages
|
|
|
What are the histologic signs of an ischemic stroke 1-2 weeks after it occurs?
|
Reactive gliosis + Vascular proliferation
|
|
|
What are the histologic signs of an ischemic stroke >2 weeks after it occurs?
|
Glial scar
|
|
|
What are the types of strokes?
|
- Hemorrhagic stroke
- Ischemic stroke: thrombotic, embolic, and hypoxic - Transient ischemic attack |
|
|
What can cause a hemorrhagic stroke?
|
- Hypertension
- Anticoagulation - Cancer (abnormal vessels can bleed) - 2° to ischemic stroke followed by reperfusion (↑ vessel fragility) |
|
|
What is the most common site of hemorrhagic strokes (intracerebral hemorrhages)?
|
Basal ganglia
|
|
|
What is the consequence of an ischemic stroke?
|
Liquefactive necrosis
|
|
|
What are the types of ischemic strokes?
|
- Thrombotic
- Embolic - Hypoxic |
|
|
What causes a thrombotic ischemic stroke?
|
Clot forms directly at the site of infarction (commonly the MCA), usually over an atherosclerotic plaque
|
|
|
What causes an embolic ischemic stroke?
|
Embolus from another part of the body obstructs a vessel, can affect multiple vascular territories; often cardioembolic
|
|
|
What causes a hypoxic ischemic stroke?
|
Due to hyperperfusion or hypoxemia
- Common during cardiovascular surgeries, tends to affect watershed areas |
|
|
How do you treat an ischemic stroke?
|
tPA (if within 3-4.5 hours of onset and no hemorrhage/risk of hemorrhage)
|
|
|
How do you reduce the risk of an ischemic stroke?
|
- Medical therapy: aspirin, clopidogrel
- Optimum control of BP, blood sugars, and lipids - Treat conditions that increase the risk (eg, atrial fibrillation) |
|
|
What is a transient ischemic attack (TIA)?
|
- Brief, reversible episode of focal neurologic dysfunction lasting <24 hours without acute infarction (- MRI)
- Majority of resolve in <15 minutes - Deficits are due to focal ischemia |
|
|
What are the large venous channels that run through the dura? Purpose?
|
Dural venous sinuses - drains blood from cerebral veins and receives CSF from arachnoic granulations
|
|
|
What do the dural venous sinuses drain into?
|
Internal Jugular Vein
|
|
|
What are the ventricles of the brain?
|
- Lateral ventricle
- 3rd ventricle - 4th ventricle |
|
|
What is the path through the ventricular system of the brain?
|
- Lateral ventricle → R & L interventricular foramina of Monro → 3rd ventricle
- 3rd ventricle → Cerebral Aqueduct (of Sylvius) → 4th ventricle - 4th ventricle → Foramina of Luschka and Foramen of Magendie → Subarachnoid Space |
|
|
What connects the lateral ventricles and 3rd ventricle?
|
R and L Interventricular Foramina of Monro
|
|
|
What connects the 3rd and 4th ventricles?
|
Cerebral Aqueduct of Sylvius
|
|
|
What connects the 4th ventricle to the subarachnoid space?
|
- Foramina of Luschka (lateral)
- Foramen of Magendie (medial) |
|
|
What is the origin of CSF?
|
Ependymal cells of choroid plexus
|
|
|
How is CSF reabsorbed?
|
Arachnoid granulations absorb CSF and drain it into the dural venous sinuses
|
|
|
What are the types of hydrocephalus?
|
Communicating (non-obstructive)
- Communicating hydrocephalus - Normal pressure hydrocephalus - Hydrocephalus ex vacuo Non-Communicating (obstructive) - Non-communicating hydrocephalus |
|
|
What is the cause of communicating hydrocephalus? What does it lead to?
|
- ↓ CSF absorption by arachnoid granulations (eg, arachnoid scarring post-meningitis)
- Causes ↑ intracranial pressure, papilledema, and herniation |
|
|
What is the cause of normal pressure hydrocephalus? What does it lead to?
|
- Does not result in increased subarachnoid space volume
- Expansion of ventricles distorts the fibers of the corona radiata and leads to the clinical triad of urinary incontinence, ataxia, and cognitive dysfunction (sometimes reversible) - "Wet, wobbly, and wacky" |
|
|
What is the cause of hydrocephalus ex vacuo? What does it lead to?
|
- Appearance of ↑ CSF in atrophy (eg, Alzheimer disease, advanced HIV, Pick disease)
- Intracranial pressure is normal - triad is not seen - Apparent increase in CSF observed on imaging is actually the result of ↓ neural tissue due to neuronal atrophy |
|
|
What is the cause of non-communicating hydrocephalus? What does it lead to?
|
Caused by a structural blockage of CSF circulation within the ventricular system (eg, stenosis of the aqueduct of Sylvius)
|
|
|
How many spinal nerves are there? Types?
|
31 total spinal nerves:
- 8 cervical - 12 thoracic - 5 lumbar - 5 sacral - 1 coccygeal |
|
|
How do the spinal nerves exit relative to the vertebrae?
|
- Nerves C1-C7 exit ABOVE the corresponding vertebra
- All other nerves exit BELOW the corresponding vertebra |
|
|
What happens in a vertebral disc herniation? What direction?
|
- Nucleus pulposus (soft central disc) herniates through annulus fibrosis (outer ring)
- Usually occurs in posterolateral direction |
|
|
What is the most common location for a vertebral disc herniation?
|
- L4-L5
- L5-S1 |
|
|
How far down does the spinal cord extend?
|
Extends to lower border of L1-L2 vertebrae
|
|
|
How low does the subarachnoid space (which contains CSF) extend?
|
Extends to lower border of S2 vertebra
|
|
|
Where do you do a lumbar puncture? Why?
|
Between L3-L4 or L4-L5 (level of cauda equina)
- Goal is to obtain sample of CSF without damaging the spinal cord - To keep the cord alive, keep the spinal needle between L3 and L5 |
|
|
What are the tracts in the dorsal column? Function?
|
Ascending tracts of dorsal column:
- Fasciculus gracilis: pressure, vibration, touch proprioception sensation from lower body and legs - Fasciculus cuneatus: same sensation from upper body and arms |
|
|
What is the orientation of spinal nerves in the dorsal column?
|
From medial to lateral:
Fasciculus gracilis: - Sacral - Lumbar Fasciculus cuneatus: - Thoracic - Cervical |
|
|
What tracts carry sensory information about pressure, vibration, touch, and proprioception? Location?
|
Fasciculus gracilis and cuneatus
- Found in dorsal column |
|
|
What tracts carry sensory information about pain and temperature? Orientation?
|
Lateral Spinothalamic Tract
- Lateral: sacral - Medial: cervical |
|
|
What tracts carry sensory information about crude touch and pressure?
|
Anterior Spinothalamic Tract
|
|
|
What tracts carry voluntary motor information? Orientation?
|
Lateral Corticospinal Tract
- Lateral: sacral - Medial: cervical Anterior Corticospinal Tract |
|
|
What is the function of the dorsal column in the spinal cord?
|
Ascending sensory information: pressure, vibration, fine touch, and proprioception
|
|
|
What is the path of the first order neuron of the dorsal column?
|
- Sensory nerve ending → cell body in dorsal root ganglion → enters spinal cord, ascends ipsilaterally in the dorsal column
- Synapses on the ipsilateral nucleus cutaneous or gracilis (in medulla) |
|
|
What is the path of the second order neuron of the dorsal column?
|
- Originates from the ipsilateral nucleus cutaneous or gracilis (in medulla)
- Decussates in medulla → ascends contralaterally in medial lemniscus - Synapses on VPL (thalamus) |
|
|
What is the path of the third order neuron of the dorsal column?
|
- Originates in VPL (in thalamus)
- Travels to sensory cortex |
|
|
What is the function of the spinothalamic tract in the spinal cord?
|
Ascending sensory information:
- Lateral: pain and temperature - Anterior: crude touch and pressure |
|
|
What is the path of the first order neuron of the spinothalamic tract?
|
- Sensory nerve ending (Aδ and C fibers) (cell body in dorsal root ganglion) → enters spinal cord
- Synapses on ipsilateral gray matter (spinal cord) |
|
|
What is the path of the second order neuron of the dorsal column?
|
- Originates at ipsilateral gray matter (in spinal cord)
- Decussates at anterior white commissure and ascends contralaterally - Synapses on VPL (thalamus) |
|
|
What is the path of the third order neuron of the dorsal column?
|
- Originates on VPL (thalamus)
- Travels to sensory cortex |
|
|
What is the function of the lateral corticospinal tract in the spinal cord?
|
Descending:
- Voluntary movement of contralateral limbs |
|
|
What is the path of the first order neuron of the lateral corticospinal tract?
|
- UMN: cell body in 1° motor cortex → descends ipsilaterally (through internal capsule), most fibers decussate at caudal medulla (pyramidal decussation) → descends contralaterally
- Synapses on cell body of anterior horn (in spinal cord) |
|
|
What is the path of the second order neuron of the spinothalamic tract?
|
- LMN originates in cell body of anterior horn of spinal cord
- LMN leaves spinal cord and synapses at neuromuscular junction |
|
|
What are the signs of an upper motor neuron lesion?
|
Everything UP (tone, reflexes, toes):
- Weakness - ↑ Reflexes - ↑ Tone - Babinski sign - Spastic paralysis - Clasp knife spasticity |
|
|
What are the signs of a lower motor neuron lesion?
|
Everything LOWERED (less muscle mass, ↓ muscle tone, ↓ reflexes, downgoing toes):
- Weakness - Atrophy - Fasciculations - ↓ Reflexes - ↓ Tone - Flaccid paralysis |
|
|
What are fasciculations?
|
Muscle twitching
|
|
|
What is a positive Babinski sign indicative of?
|
- Normal in infants
- Positive in UMN lesions |
|

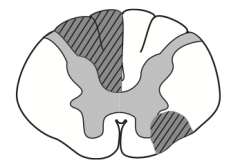
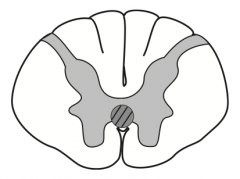
What kind of disease causes this area to be injured? Characteristics of lesion?
|

- Caused by poliomyelitis and spinal muscular atrophy (Werdnig-Hoffman disease)
- LMN lesions only, due to destruction of anterior horns - Causes flaccid paralysis |
|
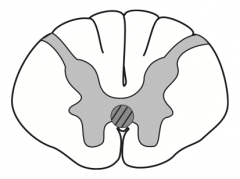
What kind of disease causes this area to be injured? Characteristics of lesion?
|
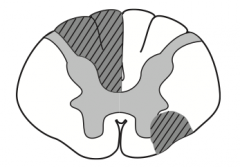
Multiple Sclerosis
- Due to demyelination of random regions (often asymettric) - Mostly white matter of cervical region - Scanning speech, intention tremor, and nystagmus |
|

What kind of disease causes this area to be injured? Characteristics of lesion?
|

Amyotrophic Lateral Scerlosis / Lou Gehrig disease:
- Can be caused by defect in superoxide dismutase 1 - Combined UMN and LMN deficits with no sensory, cognitive, or oculomotor deficits (both UMN and LMN signs) - Commonly presents as fasciculations with eventual atrophy and weakness of hands - No cognitive defect - Fatal |
|

What drug can be used to treat this condition?
|

Amyotrophic Lateral Scerlosis / Lou Gehrig disease:
- Riluzole treatment modestly ↑ survival by ↓ presynaptic glutamate release |
|
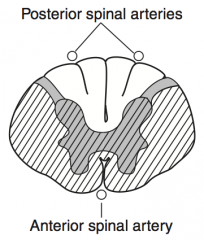
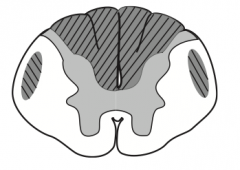
What kind of disease causes this area to be injured? Characteristics of lesion?
|
Complete Occlusion of Anterior Spinal Artery
- Spares dorsal columns and Lissauer tract - Upper thoracic ASA territory is a watershed area, as artery of Adamkiewicz supplies ASA below T8 |
|
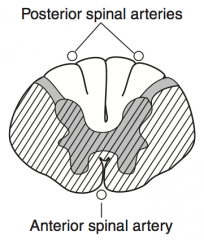
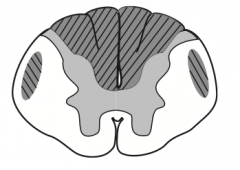
What kind of disease causes this area to be injured? Characteristics of lesion?
|
Tabes Dorsalis (caused by 3° syphilis)
- Results from degeneration / demyelination of dorsal columns and roots → impaired sensation and proprioception and progressive sensory ataxia (inability to sense or feel legs → poor coordination) - Absence of reflexes and positive Romberg |
|
|
What is Tabes Dorsalis associated with?
|
- Charcot joints
- Shooting pain - Argyll Robertson pupils (small bilateral pupils that further constrict to accommodation and convergence, but not to light) - Exam will demonstrate absence of reflexes and positive Romberg |
|
|
What is the term for pupils that are small bilaterally that constrict to accommodation and convergence, but not to light?
|
Tabes Dorsalis
|
|
What kind of disease causes this area to be injured? Characteristics of lesion?
|
Syringomyelia
- Syrinx expands and damages anterior white commissure of spinothalamic tract (2nd order neurons) - Bilateral loss of pain and temperature sensation (usually C8-T1) - Seen with Chiari I malformation - Can expand and affect other tracts |
|
What kind of disease causes this area to be injured? Characteristics of lesion?
|
Vitamin B12 or Vitamin E deficiency:
- Subacute combined degeneration - Demyelination of dorsal columns, lateral corticospinal tracts, and spinocerebellar tracts - Ataxic gait, paresthesia, impaired position and vibration sense |
|
|
What causes Poliomyelitis?
|
Poliovirus (fecal-oral transmission)
|
|
|
How does poliovirus infect someone?
|

- Replicates in the oropharynx and small intestine
- Spreads to the CNS via the bloodstream - Infection causes destruction of cells in the anterior horn of the spinal cord (LMN death) |
|
|
What are the symptoms of Poliomyelitis?
|
LMN lesions signs:
- Weakness - Hypotonia - Flaccid paralysis - Fasciculations - Hyporeflexia - Muscle atrophy |
|
|
What are the signs of a poliovirus infection?
|
- Malaise
- Headache - Fever - Nausea |
|
|
What are the lab findings associated with poliomyelitis?
|
- CSF: ↑ WBCs and slight ↑ of protein (no change in CSF glucose)
- Virus recovered from stool or throat |
|
|
What causes "floppy baby" syndrome?
|
Spinal Muscular Atrophy (Werdnig-Hoffmann Disease)
- Congenital degeneration of anterior horns of spinal cord → LMN lesion - Autosomal recessive inheritance |
|
|
What are the symptoms of the congenital degeneration of the anterior horns of the spinal cord?
|
Floppy Baby: Spinal Muscular Atrophy (Werdnig-Hoffmann Disease)
- Marked hypotonia and tongue fasciculations - Median age of death is 7 months |
|
|
What causes degeneration of multiple spinal cord tracts leading to muscle weakness and loss of deep reflexes, vibratory sense, and proprioception?
|
Friedreich Ataxia
- Autosomal recessive trinucleotide repeat disorder (GAA) on chromosome 9 (encodes Frataxin - iron binding protein) - Impairs mitochondrial functioning - Leads to degeneration of multiple spinal cord tracts |
|
|
What is the cause of Friedreich Ataxia?
|
- Autosomal recessive trinucleotide repeat disorder (GAA) on chromosome 9 (encodes Frataxin - iron binding protein)
- Impairs mitochondrial functioning - Leads to degeneration of multiple spinal cord tracts |
|
|
What are the problems caused by Friedreich Ataxia?
|
- Muscle weakness
- Loss of deep reflexes - Loss of vibratory sense - Loss of proprioception |
|
|
What are the symptoms caused by Friedreich Ataxia?
|
- Staggering gait
- Frequent falling - Nystagmus - Dysarthria - Pes cavus - Hammer toes - Hypertrophic cardiomyopathy (cause of death) - Presents in childhood with kyphoscoliosis |
|
|
What disease presents in childhood with kyphoscoliosis? Cause of death?
|
Friedreich Ataxia
- Cause of death is hypertrophic cardiomyopathy |
|
|
What is the mnemonic to remember the characteristics of Friedreich Ataxia?
|
"Friedreich is FRATAstic (Frataxin gene): He's your favorite FRAT brother, always stumbling, staggering, and falling, but he has a big heart (hypertrophic cardiomyopathy)"
|
|
|
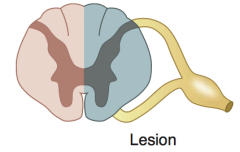
What is the cause of Brown-Séquard Syndrome?
|
Hemisection of Spinal Cord
|
|
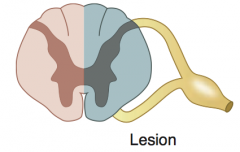
What is the name for the syndrome caused by a hemisection of the spinal cord? What are the neurologic findings?
|
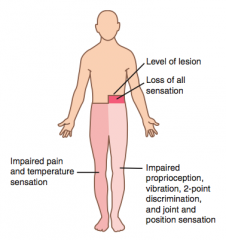
Brown-Séquard Syndrome
- Ipsilateral UMN signs BELOW the lesion (corticospinal tract damage) - Ipsilateral loss of tactile, vibration, proprioceptio sense 1-2 levels BELOW the lesion (dorsal column damage) - Contralateral pain and temperature loss BELOW level of lesion (spinothalamic tract damage) - Ipsilateral loss of all sensation AT level of lesion - Ipsilateral LMN signs (eg, flaccid paralysis) AT level of lesion |
|
|
What are the additional problems that can be associated with a patient with Brown-Séquard Syndrome if the lesion occurs above T1?
|
Patient may present with Horner Syndrome due to damage of the oculosympathetic pathway
|
|
|
What are the ipsilateral findings associated with a hemisection of the spinal cord?
|
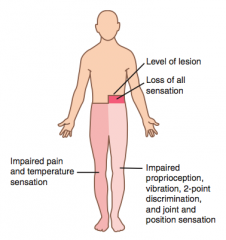
- UMN signs below lesion
- Loss of tactile, vibration, proprioception 1-2 levels below lesion - Loss of all sensation at level of lesion - LMN signs at level of lesion (eg, flaccid paralysis) |
|
|
What are the contralateral findings associated with a hemisection of the spinal cord?
|
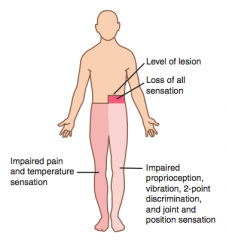
Loss of pain and temperature sensation below level of lesion
|
|
|
What are the symptoms of Horner syndrome?
|
- Ptosis (slight drooping of the eyelid)
- Anhidrosis (absence of sweating) and flushing (rubor) - Miosis (pupil constriction) |
|
|
What happens to the eyelid in Horner Syndrome? Why?
|
Ptosis: slight drooping of eyelid - no input to superior tarsal muscle
|
|
|
What happens to the face in Horner Syndrome? Why?
|
- Anhidrosis: absence of sweating
- Rubor: flushing |
|
|
What happens to the pupil in Horner Syndrome? Why?
|
Miosis: pupil constriction
|
|
|
What lesion is Horner Syndrome associated with?
|
Lesion of spinal cord above T1 (eg, Pancoast tumor, Brown-Séquard syndrome [cord hemisection], late-stage syringomyelia)
|
|
|
What pathway is damaged leading to ptosis, anhidrosis, and miosis?
|
Interruption of the 3-neuron oculosympathetic pathway projects from the hypothalamus to the intermediolateral column of the spinal cord → superior cervical (sympathetic) ganglion → pupil, smooth muscle of eyelids, and the sweat glands of the forehead and face
|
|
|
What is the dermatome associated with the posterior half of the skull "cap"?
|
C2
|
|
|
What is the dermatome associated with the high turtleneck shift?
|
C3
|
|
|
What is the dermatome associated with a low-collar shirt?
|
C4
|
|
|
What is the dermatome associated with the nipples?
|
T4
|
|
|
What is the dermatome associated with the xiphoid process?
|
T7
|
|
|
What is the dermatome associated with the umbilicus?
|
T10 (at the belly butTEN)
|
|
|
What is the dermatome associated with the inguinal ligament?
|
L1
|
|
|
What is the dermatome associated with the kneecaps?
|
L4 (down on ALL 4's)
|
|
|
What is the dermatome associated with the erection and sensation of the penile and anal zones?
|
S2, S3, and S4
(S2, 3, 4 keep the penis off the floor) |
|
|
What nerve root is tested by the biceps reflex?
|
C5 nerve root
|
|
|
What nerve root is tested by the triceps reflex?
|
C7 nerve root
|
|
|
What nerve root is tested by the patellar reflex?
|
L4 nerve root
|
|
|
What nerve root is tested by the achilles reflex?
|
S1 nerve root
|
|
|
What nerve root is tested by the cremaster reflex (movement of testicles)?
|
L1 and L2
|
|
|
What nerve root is tested by the anal wink reflex?
|
S3 and S4
|
|
|
What is the mnemonic to remember the nerve roots associated with the clinical reflexes?
|
S1, 2 - buckle my shoe (Achilles reflex)
L3, 4 - kick the door (patellar reflex) C5, 6 - pick up sticks (biceps reflex) C7, 8 - lay them straight (patellar reflex) L1, L2 - testicles move (cremaster reflex) S3, S4 - winks galore (anal wink reflex) |
|
|
What are primitive reflexes? Types?
|
CNS reflexes that are present in a healthy infant, but are absent in a neurologically intact adult; normally disappear within 1st year of life
- Moro reflex - Rooting reflex - Sucking reflex - Palmar reflex - Plantar reflex - Galant reflex |
|
|
What happens to the primitive reflexes present in healthy infants?
|
- Normally disappear in the first year of life
- These primitive reflexes are inhibited by a mature / developing frontal lobe - They reemerge in adults following frontal lobe lesions → loss of inhibition of these reflexes |
|
|
What reflex causes babies to abduct / extend their limbs when they are startled and then draw them together?
|
Moro Reflex: "Hang on for life" reflex
|
|
|
What reflex causes babies to move their head to one side if the cheek is stroked? Function?
|
Rooting Reflex - nipple seeking
|
|
|
What reflex occurs when the roof of the mouth in a baby is touched?
|
Sucking Reflex
|
|
|
What reflex occurs when the palm of a baby's hand is stroked?
|
Palmar Reflex - causes them to curl their fingers
|
|
|
What reflex occurs when the plantar surface of a baby's foot is stimulated?
|
Plantar Reflex - causes dorsiflexion of large toe and fanning of other toes
Called the Babinski sign when it occurs in adults (UMN lesion) |
|
|
What reflex occurs when the side of the spine in a baby is stroked when they are in the ventral suspension (face down)?
|
Galant Reflex - lateral flexion of the lower body toward the stimulated side
|
|
|
What CNs lie medially in the brain stem?
|
III, VI, XII
Motor = Medial |
|
|
What is the function of the pineal gland?
|
- Melatonin secretion
- Circadian rhythm |
|
|
What is the function of the superior colliculi?
|
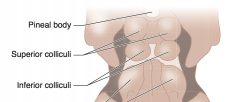
Conjugate vertical gaze center
|
|
|
What is the function of the inferior colliculi?
|
Auditory function
|
|
|
What is the term for the syndrome caused by a lesion of the superior colliculi? What are the symptoms? What can cause this?
|
Parinaud Syndrome
- Paralysis of conjugate vertical gaze - Cause: Pinealoma |
|
|
What is the name and function of CN I? Type?
|
Olfactory (I)
- Smell: only CN without thalamic relay to cortex - Sensory only |
|
|
What is the name and function of CN II? Type?
|
Optic (II)
- Sight - Sensory only |
|
|
What is the name and function of CN III? Type?
|
Oculomotor (III)
- Eye movement (SR, IR, MR, IO) - Pupillary constriction (sphincter pupillae: Edinger-Westphal nucleus w/ muscarinic receptors) - Accommodation - Eyelid opening (levator palpebrae) - Motor only |
|
|
What is the name and function of CN IV? Type?
|
Trochlear (IV)
- Eye movement (SO) - Motor only |
|
|
What is the name and function of CN V? Type?
|
Trigeminal (V)
- Mastication, facial sensation (ophthalmic, maxillary, mandibular divisions) - Somatosensation from anterior 2/3 of tongue - Sensory and motor function |
|
|
What is the name and function of CN VI? Type?
|
Abducens (VI)
- Eye movement (LR) - Motor only |
|
|
What is the name and function of CN VII? Type?
|
Facial (VII)
- Facial movement - Taste from anterior 2/3 of tongue - Lacrimation - Salivation (submandibular and sublingual glands) - Eyelid closing (orbicularis oculi) - Stapedius muscle in ear - Note: nerve courses through parotid gland, but does not innervate it - Both sensory and motor function |
|
|
What is the name and function of CN VIII? Type?
|
Vestibulocochlear (VIII)
- Hearing and balance - Sensory only |
|
|
What is the name and function of CN IX? Type?
|
Glossopharyngeal (IX)
- Taste and somatosensation from posterior 1/3 of tongue - Swallowing - Salivation (parotid gland) - Monitoring carotid body and sinus chemo- and baroreceptors - Stylopharyngeus (elevates pharynx and larynx) - Sensory and motor function |
|
|
What is the name and function of CN X? Type?
|
Vagus (X)
- Taste from epiglottic region - Swallowing - Soft palate elevation - Midline uvula - Talking - Coughing - Thoracoabdominal viscera - Monitoring aortic arch chemo- and baroreceptors - Both sensory and motor function |
|
|
What is the name and function of CN XI? Type?
|
Accessory (XI)
- Head turning (SCM) and shoulder shrugging (trapezius) - Motor only |
|
|
What is the name and function of CN XII? Type?
|
Hypoglossal (XII)
- Tongue movement - Motor only |
|
|
What is the mnemonic for remembering which CNs have motor and sensory function?
|
Some Say Marry Money But My Brother Says Big Boobs Matter More
|
|
|
Where are the cranial nerve nuclei located?
|
Tegmentum portion of the brain stem (between the dorsal and ventral portions)
|
|
|
What CN nuclei are in the midbrain?
|
Nuclei of CN III, IV
>4 |
|
|
What CN nuclei are in the pons?
|
Nuclei of CN V, VI, VII, VIII
5-8 |
|
|
What CN nuclei are in the medulla?
|
Nuclei of CN IX, X, XII
(>9, except 11) |
|
|
What CN nuclei are in the spinal cord?
|
Nucleus of CN XI
|
|
|
Which CN nuclei are located laterally?
|
Lateral nuclei = Sensory (aLar plate)
|
|
|
Which CN nuclei are located medially?
|
Medial nuclei = Motor (basal plate)
|
|
|
What separates the sensory nuclei from the motor nuclei?
|
Sulcus Limitans separates Alar plate (sensory/lateral) from the Basal plate (motor/medial)
|
|
|
What makes up the afferent and efferent branches of the corneal reflex?
|
- Afferent: V1 ophthalmic (nasociliary branch)
- Efferent: VII (temporal branch: orbicularis oculi) |
|
|
What makes up the afferent and efferent branches of the lacrimation reflex?
|
- Afferent: V1 (loss of reflex does not preclude emotional tears)
- Efferent: VII |
|
|
What makes up the afferent and efferent branches of the jaw jerk reflex?
|
- Afferent: V3 (sensory - muscle spindle from masseter)
- Efferent: V3 (motor - masseter) |
|
|
What makes up the afferent and efferent branches of the pupillary reflex?
|
- Afferent: II
- Efferent: III |
|
|
What makes up the afferent and efferent branches of the gag reflex?
|
- Afferent: IX
- Efferent: X |
|
|
What are the nuclei of the vagus nerve?
|
- Nucleus Solitarius
- Nucleus Ambiguus - Dorsal Motor Nucleus |
|
|
What kind of information comes through the nucleus solitarius? What CNs have their nuclei here?
|
Visceral sensory information (eg, taste, baroreceptors, gut distention): CN VII, IX, and X
|
|
|
What kind of information comes through the nucleus ambiguus? What CNs have their nuclei here?
|
Motor innervation of pharynx, larynx, and upper esophagus (eg, swallowing, palate elevation): CN IX, X, and XI (cranial portion)
|
|
|
What kind of information comes through the dorsal motor nucleus? What CNs have their nuclei here?
|
Sends autonomic (parasympathetic) fibers to the heart, lungs, and upper GI: CN X
|
|
|
Which CNs pass through the Cribriform Plate?
|
CN I (Olfactory)
|
|
|
Which CNs pass through the middle cranial fossa of the sphenoid bone?
|
2-6
- CN II (Optic) - CN III (Oculomotor) - CN IV (Trochlear) - CN V (Trigeminal) - CN VI (Abducens) |
|
|
Which structures pass through the optic canal?
|
- CN II
- Ophthalmic artery - Central retinal vein |
|
|
Which structures pass through the superior orbital fissure?
|
- CN III, IV, V1, VI
- Ophthalmic vein - Sympathetic fibers |
|
|
Which structures pass through the Foramen Rotundum?
|
CN V2
|
|
|
Which structures pass through the Foramen Ovale?
|
CN V3
|
|
|
Which structures pass through the Foramen Spinosum?
|
Middle Meningeal Artery
|
|
|
Which CNs pass through the posterior cranial fossa of the temporal and occipital bone?
|
7-12
- CN VII: Facial - CN VIII: Vestibulocochlear - CN IX: Glossopharyngeal - CN X: Vagus - CN XI: Accessory - CN XII: Hypoglossal |
|
|
Which structures pass through the internal auditory meatus?
|
- CN VII
- CN VIII |
|
|
Which structures pass through the jugular foramen?
|
- CNs IX, X, XI
- Jugular vein |
|
|
Which structures pass through the hypoglossal canal?
|
CN XII
|
|
|
Which structures pass through the Foramen Magnum?
|
- Spinal roots of CN XI
- Brain stem - Vertebral arteries |
|
|
Through what structures do the divisions of CN V exit the skull?
|
Middle cranial fossa in sphenoid bone
- V1: Superior orbital fissure - V2: Foramen rotundum - V3: Foramen ovale |
|
|
What is the cavernous sinus?
|
Collection of venous sinuses on either side of the pituitary
|
|
|
What blood drains into the cavernous sinus? Where does it drain next?
|
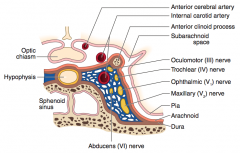
- Drains from eye and superficial cortex → cavernous sinus
- Cavernous sinus drains → internal jugular vein |
|
|
What structures are found within the cavernous sinus?
|
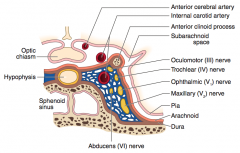
- CN III, IV, V1, V2, and VI and post-ganglionic sympathetic fibers (nerves that control extra-ocular muscles (plus V1 and V2))
- Internal carotid artery |
|
|
What causes cavernous sinus syndrome?
|
- Mass effect
- Fistula - Thrombosis |
|
|
What are the symptoms of cavernous sinus syndrome?
|
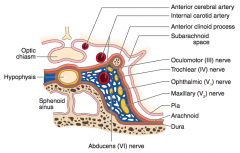
- Ophthalmoplegia (paralysis of the muscles within or surrounding the eye)
- ↓ Corneal and maxillary sensation with normal visual acuity - CN VI commonly affected |
|
|
What are the common cranial nerve lesions?
|
- CN V motor lesion
- CN X lesion - CN XI lesion - CN XII lesion (LMN) |
|
|
What nerve lesion could cause the jaw to deviate to one side? How?
|
CN V motor lesion: jaw deviates TOWARD the side of the lesion due to unopposed force from the opposite pterygoid muscle
|
|
|
What nerve lesion could cause the uvula to deviate to one side? How?
|
CN X lesion: uvula deviates AWAY from side of lesion, weak side collapses and uvula points away
|
|
|
What nerve lesion could cause weakness of turning the head and shoulder droop? How?
|
CN XI lesion: weakness turning the head toward the CONTRALATERAL side of the lesion (SCM), shoulder droop on side of lesion (trapezius); the left SCM contracts to help turn the head to the right
|
|
|
What nerve lesion could cause the tongue to deviate to one side? How?
|
CN XII lesion (LMN): tongue deviates TOWARD side of lesion ("lick your wounds") due to weakened tongue muscles on the affected side
|
|
|
What are the components and function of the outer ear?
|
- Consists of the visible portion of the ear (pinna), including the auditory canal and eardrum
- Transfers sound waves via vibration of eardrum |
|
|
What are the components and function of the middle ear?
|
- Air filled space with three bones called the ossicles (malleus, incus, stapes)
- Ossicles conduct and amplify sound from the eardrum to the inner ear |
|
|
What are the components and function of the inner ear?
|
- Snail-shaped, fluid-filled cochlea
- Contains basilar membrane that vibrates 2° to sound waves - Vibration transduced via specialized hair cells→ auditory nerve signaling → brainstem |
|
|
How does the frequency of sound waves relate to the basilar membrane?
|
Tonotopy:
- Low frequency heard at apex hear helicotrema (wide and flexible) - High frequency heard best at base of cochlea (thin and rigid) |
|
|
Where are low frequency sounds heard best?
|
Apex of basilar membrane (wide and flexible)
|
|
|
Where are high frequency sounds heard best?
|
Base of cochlea / basilar membrane (thin and rigid)
|
|
|
What are the types of hearing loss?
|
- Conductive
- Sensorineural - Noise-induced |
|
|
What type of hearing loss causes an abnormal Rinne test (bone > air) and a Weber test that localizes to the affected ear?
|
Conductive Hearing Loss
|
|
|
What type of hearing loss causes a normal Rinne test (air > bone) and a Weber test that localizes to the unaffected ear?
|
Sensorineural Hearing Loss
|
|
|
What causes noise-induced hearing loss?
|
Damage to sterociliated cells in organ of Corti
- Loss of high frequency hearing first - Sudden extremely loud noises can produce hearing loss due to tympanic membrane rupture |
|
|
What is a normal Rinne test result?
|
Air conducts sound/vibration better than bone
|
|
|
How does the Weber test help you determine the type of hearing loss?
|
- Localizes to AFFECTED ear: CONDUCTIVE hearing loss
- Localizes to UNAFFECTED ear: SENSORINEURAL hearing loss |
|
|
How does the Rinne test help you determine the type of hearing loss?
|
- Abnormal (bone > air): Conductive
- Normal (air > bone): Sensorineural |
|
|
What type of hearing loss is characterized by loss of high frequency hearing first?
|
Noise-induced hearing loss
|
|
|
How can sudden extremely loud noises produce hearing loss?
|
Due to tympanic membrane rupture
|
|
|
What are the types of facial lesions?
|
- UMN lesion
- LMN lesion - Facial nerve palsy |
|
|
What kind of lesion causes paralysis of the lower face with the forehead spared?
|
- UMN lesion of facial nerve (contralateral to lower face paralysis)
- Forehead spared because of bilateral UMN innervation |
|
|
What kind of lesion causes paralysis of the upper and lower face?
|
- LMN lesion of facial nerve (ipsilateral to face paralysis)
- Forehead affected unlike in an UMN lesion |
|
|
What causes facial nerve palsy?
|
Complete destruction of the facial nucleus itself or its branchial efferent fibers (facial nerve proper)
|
|
|
What are the symptoms of facial nerve palsy?
|

Peripheral ipsilateral facial paralysis (drooping smile) with inability to close eye on involved side
|
|
|
What can cause a facial nerve palsy (destruction of facial nucleus or its branchial efferent fibers)?
|
- Idiopathically (Bell palsy)
- Lyme disease - Herpes simplex - Less common: Herpes Zoster, Sarcoidosis, tumors, and diabetes |
|
|
How do you treat facial nerve palsy?
|
Corticosteroids
|
|
|
What muscles are involved in mastication?
|
- Masseter
- Temporalis - Medial Pterygoid - Lateral Pterygoid |
|
|
Which muscles close the jaw?
|
M's Munch:
- Masseter - Temporalis - Medial pterygoid "It takes more muscle to keep your mouth shut" (opening uses gravity) |
|
|
Which muscles open the jaw?
|
Lateral Pterygoid (lateral lowers)
"It takes more muscle to keep your mouth shut" (opening uses gravity) |
|
|
What innervates the muscles of mastication?
|
Trigeminal nerve (V3)
|
|
|
What kind of eye conditions improve with glasses?
|
Refractive Errors
|
|
|
What eye condition causes light to focus behind the retina? What is wrong with the eye?
|
Hyperopia: eye is too short for refractive power of cornea and lens
|
|
|
What eye condition causes light to focus in front of the retina? What is wrong with the eye?
|
Myopia: eye is too long for refractive power of cornea and lens
|
|
|
What eye condition causes an abnormal curvature of the cornea? Effect on vision?
|
Astigmatism
- Results in different refractive power at different axes |
|
|
What eye condition causes a decrease in focusing ability during accommodation? Why?
|
Presbyopia - due to sclerosis and ↓ elasticity
|
|
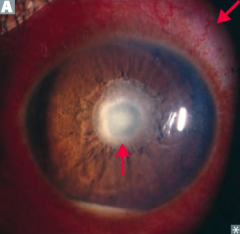
What causes sterile pus (hypopyon) and conjunctival redness?
|
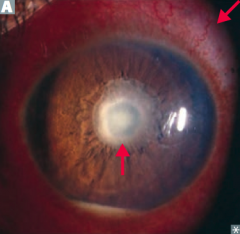
Uveitis - inflammation of anterior uvea and iris
|
|
|
What is uveitis associated with?
|
Systemic inflammatory disorders
- Sarcoid - Rheumatoid arthritis - Juvenile idiopathic arthritis - TB - HLA-B27-associated conditions |
|
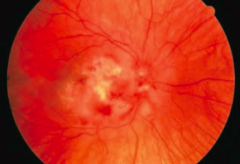
What eye condition is associated with retinal edema and necrosis leading to a scar?
|
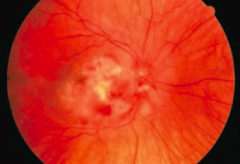
Retinitis
- Often viral (CMV, HSV, HZV) - Associated with immunosuppression |
|
|
What happens to an eye with retinitis?
|
- Retinal edema
- Necrosis leading to scar |
|
|
What causes acute, painless monocular vision loss? What is the appearance of the retina in this condition?
|
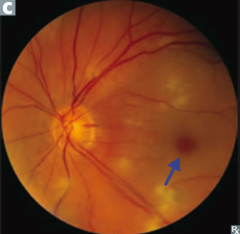
Central Retinal Artery Occlusion:
- Retina appears cloudy with attenuated vessels - Cherry-red spot at fovea |
|
|
What happens if there is central retinal artery occlusion?
|

Acute, painless monocular vision loss
|
|
|
What causes retinal hemorrhage and edema in the affected area?
|
Retinal Vein Occlusion
- Blockage of central or branch retinal vein due to compression from nearby arterial atherosclerosis |
|
|
What happens due to retinal vein occlusion?
|
- Retinal hemorrhage
- Retinal edema |
|
|
What happens to the eye in patients with diabetes?
|
Diabetic Retinopathy:
- Non-proliferative type - Proliferative type |
|
|
What causes the non-proliferative type of diabetic retinopathy? How do you treat it?
|
- Damaged capillaries leak blood → lipids and fluid seep into retina → hemorrhages and macular edema
- Treat with blood sugar control and a macular laser |
|
|
What causes the proliferative type of diabetic retinopathy? How do you treat it?
|
- Chronic hypoxia results in new blood vessel formation with resultant traction on retina
- Treat with peripheral retinal photo-coagulation and anti-VEGF injections |
|
|
What happens to the eye with glaucoma?
|
- Optic disc atrophies
- Characteristic cupping of optic disc - Usually ↑ intra-ocular pressure (IOP) - Progressive peripheral visual field loss |
|
|
In whom is there greater incidence of open angle glaucoma?
|
- ↑ Age
- African-American race - Family history - More common in US |
|
|
What is the cause of primary open angle glaucoma?
|
Causes is unclear
|
|
|
What is the cause of secondary open angle glaucoma?
|
Blocked trabecular meshwork from WBCs (eg, uveitis), RBCs (eg, vitreous hemorrhage), retinal elements (eg, retinal detachment)
|
|
|
What is the cause of primary closed/narrow angle glaucoma?
|
- Enlargement or forward movement of lens against central iris (pupil margin)
- Leads to obstruction of normal aqueous flow through pupil - Fluid builds up behind iris, pushing peripheral iris against cornea and impeding flow through the trabecular meshwork |
|
|
What is the cause of secondary closed/narrow angle glaucoma?
|
Hypoxia from retinal disease (eg, diabetes or vein occlusion) induces vasoproliferation in iris that contracts angle
|
|
|
How does the time course over which closed/narrow angle glaucoma occurs affect the prognosis?
|
- Chronic closure: often asymptomatic with damage to optic nerve and peripheral vision
- Acute closure: ophthalmologic emergency, very painful, sudden vision loss, halos around lights, rock-hard eye, frontal headache |
|
|
What are the symptoms of an acute closed/narrow angle glaucoma?
|
- Very painful
- Sudden vision loss - Halos around lights - Rock-hard eye - Frontal headache |
|
|
What should you not give a patient with acute closed/narrow angle glaucoma?
|
Don't give epinephrine because of its mydriatic effect
|
|
|
What happens in cataracts?
|
Painless, often bilateral, opacification of the lens → ↓ in vision
|
|
|
What are the risk factors for cataracts?
|
- ↑ Age
- Smoking - EtOH - Excessive sunlight - Prolonged corticosteroid use - Classic galactosemia - Galctokinase deficiency - Diabetes (sorbitol) - Trauma - Infection |
|
|
What is the term for optic disc swelling?
|
Papilledema
|
|
|
What is Papilledema? Cause?
|
- Optic disc swelling (usually bilateral)
- Due to ↑ intracranial pressure (2° to mass effect) |
|
|
What is the appearance of Papilledema on physical exam?
|
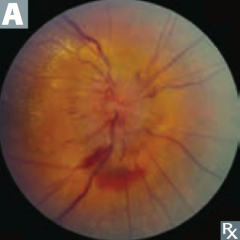
Enlarged blind spot and elevated optic disc with blurred margins on fundoscopic exam
|
|
|
What nerves innervate the extraocular muscles?
|
(LR6 SO4)3
- CN VI innervates Lateral Rectus - CN IV innervates Superior Oblique - CN III innervates Superior Rectus, Medial Rectus, Inferior Rectus, and Inferior Oblique |
|
|
What is the function of the superior oblique? Innervation?
|
- Abducts, intorts, and depresses while abducted
- Innervated by CN IV |
|
|
What lesion causes the eye to look down and out?
|
CN III damage
- Superior Rectus - Medial Rectus - Inferior Rectus - Inferior Oblique |
|
|
What are the effects of CN III damage?
|
- Eyes look down and out
- Ptosis - Pupillary dilation - Loss of accommodation |
|
|
What lesion causes the eye to move upward, particularly with contralateral gaze and head tilt toward the side of the lesion?
|
CN IV damage
- Superior Oblique |
|
|
What are the effects of CN IV damage?
|
- Eye moves upward
- Particularly moves upward with contralateral gaze and head tilt toward the side of the lesion - Problems going downstairs, may present with compensatory head tilt in the opposite direction |
|
|
What lesion causes the eye to look medially and cannot abduct?
|
CN VI damage
- Lateral Rectus |
|
|
What are the effects of CN VI damage?
|
- Medially directed eye
- Eye cannot abduct |
|
|
How does the action of the superior and inferior obliques compare to the rectuses?
|
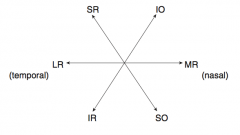
- S & I Obliques: medial
- S & I Rectuses: lateral (Obliques move the eye in the Opposite direction) |
|
|
How do you test the superior oblique?
|
Have patient depress eye from adducted position (medial)
|
|
|
How do you test the inferior oblique?
|
Have patient elevate eye from adducted position (medial)
|
|
|
How do you test the superior rectus?
|
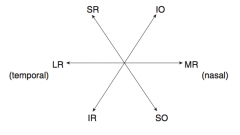
Have patient elevate eye from abducted position (lateral)
|
|
|
How do you test the inferior rectus?
|
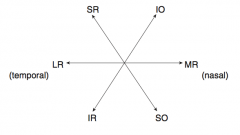
Have patient depress eye from abducted position (lateral)
|
|
|
What is the term for constriction of the pupil? How is this mediated?
|
Miosis (parasympathetic)
- 1st neuron: Edinger-Westphal nucleus → ciliary ganglion via CN III - 2nd neuron: short ciliary nerves → pupillary sphincter muscles |
|
|
What is the term for dilation of the pupil? How is this mediated?
|
Mydriasis (sympathetic)
- 1st neuron: hypothalamus → ciliospinal center of Budge (C8-T2) - 2nd neuron: exits at T1 to superior cervical ganglion (travels along cervical sympathetic chain near lung apex and subclavian vessels) - 3rd neuron: plexus along internal carotid → cavernous sinus → enters orbit as long ciliary nerve to pupillary dilator muscles |
|
|
What is the function of the short vs long ciliary nerves?
|
- Short ciliary nerves → pupillary sphincter muscle (miosis / constriction)
- Long ciliary nerves → pupillary dilator muscles (mydriasis / dilation) |
|
|
What happens when light hits the retina?
|
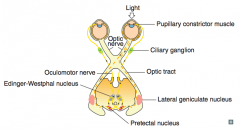
- Sends a signal via CN II → pretectal nuclei in midbrain → activates bilateral Edinger-Westphal nuclei
- Pupils contract bilaterally |
|
|
What does the swinging flashlight test check?
|
Checks for "Marcus Gunn Pupil"
- Afferent pupillary defect - Optic nerve damage or severe retinal injury → ↓ bilateral pupillary constriction when light is shone in affected eye relative to unaffected eye |
|
|
If there is an afferent pupillary defect, what would you expect to happen when you shine the line in the affected eye vs the unaffected eye?
|
When you shine in the affected eye there is less of a pupillary constriction bilaterally
|
|
|
What kind of fibers are in CN III?
|
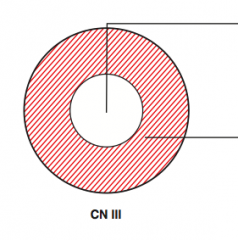
- Motor output: interior of nerve (white)
- Parasympathetic output: peripheral part of nerve (red) |
|
|
What can affect the motor output from CN III? Signs?
|
- Vascular disease (eg, diabetes: glucose → sorbitol) due to ↓ diffusion of O2 and nutrients to interior fibers from compromised vasculature that resides on outside of nerve
- Signs: ptosis, "down and out" gaze |
|
|
What can affect the parasympathetic output from CN III? Signs?
|
- Fibers on periphery are first affected by compression (eg, posterior communicating artery aneurysm or uncal herniation)
- Signs: diminished or absent pupillary light reflex, "blown pupil", often with "down-and-out" gaze |
|
|
What happens in a Retinal Detachment?
|
Separation of neurosensory layer of retina (photoreceptor layer with rods and cones) from outermost pigmented epithelium (normally shields excess light, supports retina) → degeneration of photoreceptors → vision loss
|
|
|
What can cause retinal detachment?
|
May be secondary to:
- Retinal breaks - Diabetic traction - Inflammatory effusions |
|
|
In what patients is retinal detachment more common? Clinical course?
|
- Breaks more common in patients with high myopia (nearsightedness)
- Often preceded by posterior vitreous detachment (flashes and floaters) - Eventual monocular loss of vision like a "curtain drawn down" - Surgical emergency |
|
|
What are the complications of macular degeneration?
|
Causes distortion (metamorphopsia) and eventual loss of central vision (scotomas)
|
|
|
What are the types of macular degeneration? Which is more common?
|
- Dry (non-exudative, >80%)
- Wet (exudative, 10-15%) |
|
|
What happens in dry, non-exudative macular degeneration?
|
- Deposition of yellowish extracellular material in and beneath Bruch membrane and retinal pigment epithelium ("drusen")
- Gradual ↓ in vision |
|
|
How can you prevent progression of dry, non-exudative macular degeneration?
|
Prevent progression with multivitamin and anti-oxidant supplements
|
|
|
What happens in wet, exudative macular degeneration?
|
Rapid loss of vision due to bleeding secondary to choroidal neovascularization
|
|
|
How do you treat wet, exudative macular degeneration?
|
Anti-vascular endothelial growth factor injections (anti-VEGF) or laser
|
|
What causes this visual defect?
|
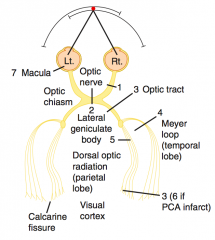
1. Right Anopia - lesion to R optic nerve
|
|
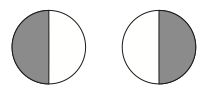
What causes this visual defect?
|
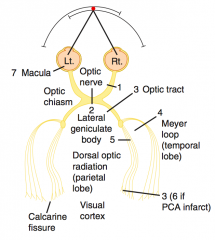
2. Bitemporal Hemianopia - pituitary lesion, lesion at chiasm
|
|
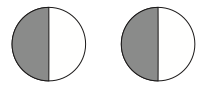
What causes this visual defect?
|
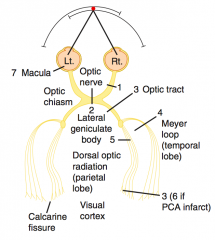
3. Left Homonymous Hemianopia - lesion to Optic Tract (after chiasm)
|
|
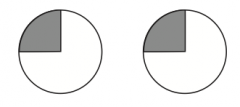
What causes this visual defect?
|
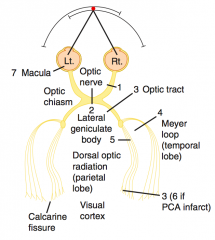
4. Left Upper Quadrantic Anopia - R temporal lesion (Meyer loop), MCA
|
|
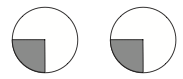
What causes this visual defect?
|
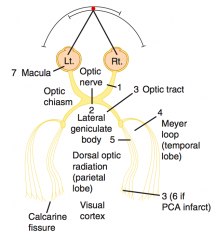
Left Lower Quadrantic Anopia
- Right parietal lesion (dorsal optic radiation), MCA |
|
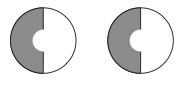
What causes this visual defect?
|
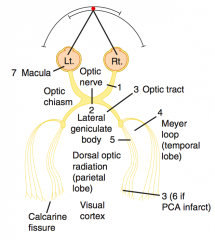
6. Left Hemianopia with Macular Sparing (PCA infarct)
|
|
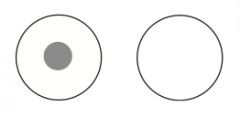
What causes this visual defect?
|
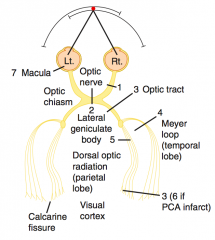
Central Scotoma
- Macular degeneration |
|
|
What is the path of Meyer's loop? What information does it carry? Lesion?
|
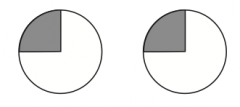
- Loops around inferior horn of lateral ventricle
- Contains visual images of inferior retina (so lesion to it causes loss of upper quadrant) |
|
|
What is the path of dorsal optic radiation? What information does it carry? Lesion?
|
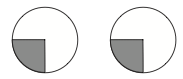
- Takes shortest path via internal capsule
- Contains visual images of superior retina (so lesion to it causes loss of lower quadrant) |
|
|
What are the characteristics of an image as it hits the primary visual cortex?
|
It is upside down and left-right reversed
|
|
|
What structure allows for crosstalk between CN VI and CN III nuclei?
|
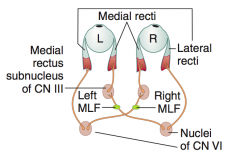
Medial Longitudinal Fasciculus (MLF)
|
|
|
What is the function of the Medial Longitudinal Fasciculus (MLF)?
|
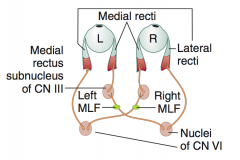
- Pair of tracts that allows for crosstalk between CN VI and CN III nuclei
- Coordinates both eyes to move in same horizontal direction - Highly myelinated (must communicate quickly so eyes move at same time) |
|
|
What disease causes injury to Medial Longitudinal Fasciculus (MLF)? Implications?
|
- Can be demyelinated in multiple sclerosis
- Causes Internuclear Ophthalmoplegia (INO) |
|
|
What is wrong in Internuclear Ophthalmoplegia (INO)?
|
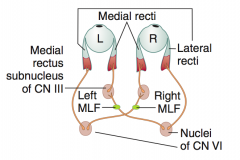
Lesion of Medial Longitudinal Fasciculus (MLF)
- Lack of communication, such that when CN VI nucleus activates ipsilateral lateral rectus, contralateral CN III nucleus does not stimulate medial rectus to fire - Abducting eye gets nystagmus (CN VI overfires to stimulate CN III) - Convergence is normal |
|
|
What happens when you look left?
|
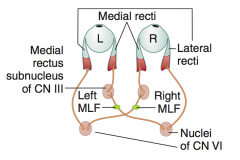
- Left nucleus of CN VI fires, which contracts the Left Lateral Rectus
- Stimulates the contralateral (right) nucleus of CN III via the Right MLF to contract the right medial rectus |
|
|
What does the "right" or "left" refer to in Right INO or Left INO?
|
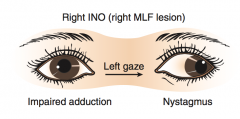
Directional term - refers to which eye is paralyzed
|

