![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
41 Cards in this Set
- Front
- Back
|
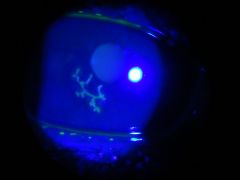
How can you visual where corneal ulceration has occurred?
|
BY using a blue-green dye, having the pt remove their contacts and using your ophthalmoscope.
|
|
|
What is a dendritic ulcer? what typically causes it?
|
(looks like a dendrite) that is located on the surface of the cornea. It has a star-like (or leaf-like) appearance and is caused by herpes simplex.
|
|
|
What are punctate ulcers? what causes them?
|

Dot-like ulcers seen on the surface of the cornea during infections w/ herpes zoster.
|
|
|
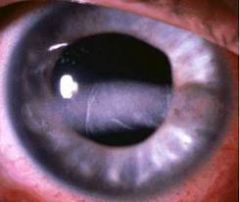
What is a corneal arcus?
|

A gray-white band of lipid depositions that parallels the edge of the cornea at the limbus.
|
|
|
What causes a corneal arcus? what affect on vision does it have?
|
Has no affect on vision and commonly occurs during middle age and later life.
|
|
|
What are pts w/ corneal arcus at risk for?
|
Hyperlipidemia and should be evaluated for another cutaneous signs like xanthalesma.
|
|
|
What is band keratopathy? what causes it?
|
A manifestation of chronic hypercalcemia that is calcium deposits beneath the corneal epithelium and may extend across the pupil to obscure vision.
|
|
|
What causes chronic hypercalcemia?
|
Chronic kidney dz, sarcoidosis and during certain cancers that metastasize to bone or that secrete PTH.
|
|
|
What is a Kayser-Fleischer ring?
|

A golden-brown or green ring that occurs at the periphery of the cornea due to copper deposition in Descemet's membrane.
***Characteristic of Wilson's dz. |
|
|
What other places are affected by wilson's disease?
|
Copper will accumulate in the liver and in the brain.
|
|
|
What is glaucoma?
|
A group of diseases associated w/ inc. intraocular pressure that is complicated by progressive optic nerve damage and visual loss.
|
|
|
What is the anterior chamber of the eye?
|
A aqueous chamber behind the cornea and in front of the lens that maintains corneal shape and provides nutrient support to the lens and cornea.
|
|
|
What produces aqueous humor?
|
The ciliary body.
|
|
|
What are the major and minor outflow tracts of aqueous humor?
|
80% of aqueous humor goes through the trabecular outflow tract (through the trabecular meshwork and out through the canal of schlemm)
20% of aqueous humor goes through the uveoscleral outflow tract (ciliary muscles and suprachoroidal space) into the venous system. |
|
|
What is normal intraocular pressure?
|
B/e 10-21 mmHg.
|
|
|
What does a intraocular pressure > 21mmHg put you at risk for?
|
Glaucoma
|
|
|
How is IOP measured?
|
W/ a Goldmann applanation tonometer.
A noncontact tonometer can also be used where it uses the puff of air to measure intraocular pressure. |
|
|
What IOP do most pts w/ glaucoma have?
|
An IOP > 30mmHg
|
|
|
What are the two types of Glaucoma?
|
1. Open angle Glaucoma (POAG)
2. Closed angle Glaucoma (narrow-angle) |
|
|
What is the most common type of Glaucoma?
|
Open-angle Glaucoma (POAG)
|
|
|
What is open-angle Glaucoma?
|
A slowly-progressive dz of gradual onset that commonly involves both eyes (bilateral) of middle aged-older adults.
|
|
|
What factors cause POAG?
|
*Familial and hereditary factors play a role in developing POAG.
|
|
|
What is the mechanism that causes POAG?
|
Caused by aqueous outflow obstruction from degenderative changes in the conventional and/or unconventional outflow tracts.
*so it is caused by degeneration of the trabecular meshwork or uveoscleral outflow tract. |
|
|
Why does POAG cause visual loss?
|
B/c the inc. IOP decreases axoplasmic flow in the optic nerve and causes retinal ganglion cell loss through a process that closely resembles apoptosis.
|
|
|
What is the normal cup to disc ratio? what is the ratio in pts w/ increased IOP?
|
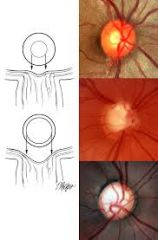
.3 in adults and >.5 in pts w/ inc. IOP
|
|
|
When is a referral to a ophthalmologist required based on cup-to-disc ratio?
|
when the c/d is >.5 in either eye, it is also required if the c/d in one is >20% larger than the ratio in the other eye.
|
|
|
What is the first symptom of POAG?
|
Decreased peripheral vision.
*"i keep running into trashcans on the side of the road" |
|
|
What is acute angle closure (narrow angle) glaucoma?
|
An ophthalmologic emergency that accounts for 10% of glaucoma cases.
|
|
|
What people does acute angle glaucoma typically occur in?
|
Occurs primarily in far-sighted asian women 55-70 y.o.
|
|
|
What are the presenting symptoms of a pt with acute angle glaucoma?
|
SEVERE eye pain that can also manifest as a severe pain in the brow or temple, nausea and vomiting.
|
|
|
What causes acute angle glaucoma?
|
Affects one eye that has a shallower anterior chamber and a narrow irido-corneal angle in a genetically predisposed person.
SO the affected eye is often smaller than normal and hyperopic (far-sighted) |
|
|
What is the mechanism behind acute angle glaucoma?
|
The iris obstructs the conventional aqueous outflow tract when the iris makes contact w/ the trabecular meshwork and blocks the canal of Schlemm.
This causes IOP to RAPIDLY increase up to 30-50 mmHg. |
|
|
What immediate affects on the eye and vision does acute angle glaucoma have?
|
corneal edema causes decreased visual acuity (visual clarity), blurred or foggy vision and colored halos around points of light.
|
|
|
What affect on the ocular muscles does acute angle glaucoma have?
|
The high IOP may cause ischemia and paralysis of the circular and radial muscles of the iris, thus the affected pupil is non-reactive and mid-dilated in size.
|
|
|
What affect in blood vessels does acute angle glaucoma have?
|
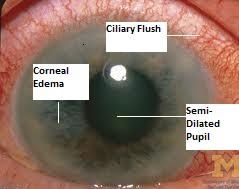
Causes congestion of the deep conjunctival and episcleral blood vessels, so the conjunctiva produces a red eye w/ a ciliary flush around the corneal limbus.
|
|
|
What affect on vision does acute angle glaucoma have?
|
Causes papilledema (inc. c/d ratio) and will cause blindness w/in hours-days depending on severity.
|
|
|
What situations can precipitate ACG?
|
1. pupil dilation due to dec. ambient light
2. pupil dilation from anti-cholinergic or sympathetic enhancing drugs. |
|
|
What causes "red eye"?
|
Congestion or hemorrhage of the conjunctival vascularture.
|
|
|
What the most common dx'es that cause red-eye? which one is NOT severe?
|
1. conjunctivities *not severe*
2. anterior uveitis 3. acute angle closure glaucoma 4. corneal trauma or infection. |
|
|
What are the danger signals that suggest sight-threatening dz?
*this is important espec. the top 5! |
1. blurred vision that doesn't disappear w/ blinking
2. dec. visual acuity 3. pain 4. photophobia 5. halos/rainbows around points of light 6. ciliary flush 7. corneal opacity (haziness0 8. abnormalities of pupil size and/or pupillary reaction to light 9. presence of a shallow anterior chamber 10. increased intraocular pressure 11. sudden proptosis. |
|
|
How can you determine iritis/uveitis from conjunctivitis?
|
By determining whether pupillary constriction causes pain in the red eye. If there is pain on pupillary constriction in response to light it is uveitis.
|

