![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
136 Cards in this Set
- Front
- Back
|
What is Blood glucose and what 2 antagonistic action controls it?
|
Blood glucose is a homeostatically regulated variable, being controlled by the antagonistic action of two hormones, insulin and glucagon.
|
|
|
What is the range for normal fasting for an individual?
|
Blood glucose is typically regulated at levels between 60 and 120 mg/dl.
|
|
|
How does the regulation of blood glucose achieved?
|
This regulation is achieved through the action of insulin and glucagon both of which are released from the islets of Langerhans (pancreatic islets) in the pancreas.
|
|
|
Glucagon is a peptide hormone that elevates blood glucose by stimulating what 2 processes? *hint 1. (the breakdown of glycogen into glucose) & 2. (making glucose from other sources).
|
Glucagon is a peptide hormone that elevates blood glucose by stimulating glycogenolysis (the breakdown of glycogen into glucose) and gluconeogenesis (making glucose from other sources).
|
|
|
A decrease in the plasma concentration of glucose will stimulate alpha cells to secrete glucagon. What is secreted when concentration levels are increased?
|
Insulin- Insulin has antagonistic actions to that of glucagon. Insulin is often referred to as the hormone of abundance because it is released when energy levels are high. Insulin is a peptide hormone that lowers plasma glucose by stimulating glycogenesis and the increased cellular uptake of glucose. Thus, it lowers blood glucose concentration.
|
|
|
The hypersecretion of the glucagon and/or the hyposecretion of insulin elevates the plasma glucose above normal levels. What is this condition?
|
This condition is known as hyperglycemia. Hypoglycemia can result if there is too little glucagon or too much insulin as well.
|
|
|
Failure of the pancreas to regulate blood glucose levels results in a disease state. Most often, the disease state is a result of the inability of the pancreas to secrete insulin, which causes hyperglycemia. This disease is referred to as?
|
diabetes mellitus.This potentially fatal disease is characterized by glycosuria (glucose in the blood), accelerated lipid and protein metabolism, ketoacidosis, polyuria (increased urine flow), polydipsia (excessive thirst) and polyphagia (excessive eating).
|
|
|
Diabetes Mellitusis a potentially fatal disease characterized by what?
|
This potentially fatal disease is characterized by glycosuria (glucose in the blood), accelerated lipid and protein metabolism, ketoacidosis, polyuria (increased urine flow), polydipsia (excessive thirst) and polyphagia (excessive eating).
|
|
|
What is glycosuria?
|
Glucose in the blood with accelerated lipid and protein metabolism.
|
|
|
What is polyuria?
|
Polyuria is increased urine flow.
|
|
|
What is polydipsia?
|
Polydipsia is excessive thirst.
|
|
|
What is polyphagia?
|
Polyphagia is excessive eating.
|
|
|
In order to diagnose diabetes mellitus, a fasting blood glucose must be obtained, what is the range mg/dl for the disease to be suspected?
|
If the fasting blood glucose is above 126 mg/dl, diabetes mellitus is suspected.
|
|
|
The amount of oxygen that leaves the lungs dissolved in plasma is what?
|
The amount of oxygen that leaves the lungs dissolved in plasma is equal to 0.3 mL of O2 per 100 mL of blood.
|
|
|
The amount of oxygen leaving the lungs in whole blood, however, is equal to what?
|
The amount of oxygen leaving the lungs in whole blood, however, is equal to 20 mL of O2 per 100 mL of blood.
|
|
|
Most of the oxygen (19.7 mL O2 per 100 mL blood), therefore, must be carried within the cellular elements of the blood. This oxygen is carried by what type of molecules within the red blood cells?
|
Most of the oxygen (19.7 mL O2 per 100 mL blood), therefore, must be carried within the cellular elements of the blood. This oxygen is carried by hemoglobin molecules within the red blood cells
|
|
|
Each hemoglobin molecule consists of two pairs of what and four disc organic groups called what?
|
Each hemoglobin molecule consists of two pairs of polypeptide chains (one pair called the alpha chains and one pair called the beta chains) and four disc-shaped organic groups called heme groups.
|
|
|
Explain heme group and its properties?
|
Each heme group contains one central ferrous ion (Fe2+) capable of bonding with one molecule of oxygen (fig. 6.1b). Thus, one molecule of hemoglobin can combine with four molecules of oxygen.
|
|
|
The rate of red blood cell production by the bone marrow is regulated by the hormone _______ secreted by the kidneys.
|
The rate of red blood cell production by the bone marrow is regulated by the hormone erythropoietin, secreted by the kidneys.
|
|
|
What is a hemocytometer?
|
The hemocytometer or haemocytometer is a device originally designed for the counting of blood cells.
|
|
|
In a hemocytometer grid 1-5 are used for what and squares A-D are used for what?
|
The hemocytometer grid. Squares 1-5 are used for red blood cell counts; squares A-D are used for white blood cell counts.
|
|
|
What is a hematocrit?
|
The ratio of the volume of packed red blood cells to the total blood volume is called the hematocrit.
|
|
|
What is red blood count (RBC)?
|
An RBC count is a blood test that tells how many red blood cells (RBCs) you have.
RBCs contain hemoglobin, which carries oxygen. How much oxygen your body tissues get depends on how many RBCs you have and how well they work. |
|
|
What is hemoglobin?
|
Hemoglobin is a protein-based component of red blood cells which is primarily responsible for transferring oxygen from the lungs to the rest of the body. Hemoglobin is actually the reason red blood cells appear red, although oxygen-rich blood is noticeably brighter than the depleted blood returning to the heart and lungs. Fresh hemoglobin is produced in the bone marrow as needed.
|
|
|
Hemoglobin absorbs light in the visible spectrum and hence is a what?
|
Hemoglobin absorbs light in the visible spectrum and hence is a pigment (a colored compound).
|
|
|
When the oxygen concentration of the blood is high, such as in the capillaries of the lungs, normal deoxyhemoglobin combines with oxygen to form the compound _______?
|
When the oxygen concentration of the blood is high, such as in the capillaries of the lungs, normal deoxyhemoglobin combines with oxygen to form the compound oxyhemoglobin.
|
|
|
When the concentration of oxygen in the blood is low, such as in the capillaries of the tissues, the oxyhemoglobin dissociates (comes apart) to form ______ and __________?
|
When the concentration of oxygen in the blood is low, such as in the capillaries of the tissues, the oxyhemoglobin dissociates (comes apart) to form reduced hemoglobin and oxygen.
|
|
|
What is carboxyhemoglobin and its properties?
|
A less common though clinically important form of hemoglobin is carboxyhemoglobin, a complex of hemoglo¬ bin and carbon monoxide. This complex, unlike oxyhemo¬ globin, does not readily dissociate; thus, the hemoglobin bonded to carbon monoxide cannot participate in oxygen
|
|
|
What is the color of carboxyhemoglobin?
|
The carboxyhemoglobin complex has a bright, cranberry red color.
|
|
|
What is methemoglobin and its properties?
|
A small percentage of hemoglobin contains iron oxidized to the ferric state (Fe3+) instead of being in the normal ferrous state (Fe2+). Hemoglobin in this oxidized state is called methemoglobin and is incapable of bond¬ ing with either oxygen or carbon monoxide.
|
|
|
An abnormally low hemoglobin, hematocrit, or red blood cell count may indicate a condition known as _______?
|
An abnormally low hemoglobin, hematocrit, or red blood cell count may indicate a condition known as anemia.
|
|
|
Anemia can be caused by what? List some examples?
|
Anemia may be caused by iron deficiency, vitamin BJ2 and folic acid deficiencies, bone marrow disease, hemolytic disease (e.g., sickle-cell anemia), loss of blood through hemorrhage, or
|
|
|
What is MCV and its formula?
|
mean corpuscular volume (MCV) =
hematocrit x 10 ----------------------------------- RBC count (millions per mm3 blood j |
|
|
What is MCHC?
|
mean corpuscular hemoglobin concentration (MCHC).
|
|
|
What is the normal range for MCV in adults? (in cubic micrometers?
|
The normal adult male and female mean corpuscular volume (MCV) ranges from 82-92 cubic micrometers.
|
|
|
What is the range for microcytic, normocytic, and macrocytic MCV?
|
microcytic <82
normocytic 82-92 macrocytic >92 |
|
|
The average normal adult male and female mean corpuscular hemoglobin concentration (MCHC) is what (in percent)?
|
The average normal adult male and female mean corpuscular hemoglobin concentration (MCHC) is
32-36 (in percent). |
|
|
What is the formula for corpuscular hemoglobin concentration MCHC?
|
Hemoglobin (g/dL) x 100
----------------------------------- Hematocrit |
|
|
Calculate your mean corpuscular volume (MCV), and enter it in the laboratory report using these examples
Hematocrit = 46 RBC count = 5.5 million |
46 X 10
--------------- = 84 5.5 |
|
|
Calculate your mean corpuscular hemoglobin concentration (MCHC) using these examples
Hematocrit = 46 Hemoglobin =16 g/dL |
16 X 100
---------------- = 35 46 |
|
|
What is the ranges for
hypochromic, normochromic, hyperchromic in mean corpuscular hemoglobin concentration (MCHC)? |
hypochromic < 32
normochromic 32-36 hyperchromic > 36 in percents |
|
|
What is the tool the Unopette System?
|
This consists of a reservoir containing the premeasured amount of diluent (left) and a plastic capillary tube within a shield (right) for puncturing the reservoir top and delivering a measured amount of whole blood to the reservoir. It looks like a dropper with a tube.
|
|
|
What is a hyperemia?
|
When your fingers become engorged with blood (hyperemia).
|
|
|
This is an anticoagulent found in the capillary tube that temporarily stops the clogging of blood so you bleed continuously.
|
Heparin
|
|
|
Normal _____________ combines with oxygen to form the compound ________.
|
Normal deoxyhemoglobin combines with oxygen to form the compound oxyhemoglobin.
|
|
|
Deoxyhemoglobin + oxygen goes to _______ and makes oxyhemoglobin.
Oxyhemoglobing goes to _________ and becomes deoxyhemoglobin + oxygen. |
Deoxyhemoglobin + oxygen goes to LUNGS and makes oxyhemoglobin.
Oxyhemoglobing goes to TISSUESand becomes deoxyhemoglobin + oxygen. |
|
|
Tell me the properties of Carboxyhemoglobin? (carbo oxy sounds like carbon dioxide)
|
Carboxyhemoglobin, a complex of hemoglobin and carbon monoxide. This complex, unlike oxyhemoglobin, does not readily dissociate; thus, the hemoglobin bonded to carbon monoxide cannot participate in oxygen transport. The carboxyhemoglobin complex has a bright, cranberry red color.
|
|
|
What are the properties of methomoglobin? (* this hemoglobin is not capable of bonding with 02 or CO2)
|
A small percentage of hemoglobin contains iron oxidized to the ferric state (Fe3+) instead of being in the normal ferrous state (Fe2+). Hemoglobin in this oxidized state is called methemoglobin and is incapable of bonding with either oxygen or carbon monoxide.
|
|
|
What are the Normal ranges for HEMOGLOBIN (males and females),
MEAN CORPUSCULAR VOLUME (MCV), and MEAN CORPUSCULAR HEMOGLOBIN CONCENTRATION (MCHC)? |
Normal hemoglobin concentration for an adult male is 13-16 g/dL, and for an adult female is 12-15 g/dL.
The normal adult male and female mean corpuscular volume (MCV) ranges from 82-92 cubic micrometers. The average normal adult male and female mean corpuscular hemoglobin concentration (MCHC) is 32-36 (in percent). |
|
|
What is the formula for Mean Corpuscular Volume (MCV)?
|
hematocrit X10
-------------------- = MCV RBC |
|
|
What is the formula for Mean Corpuscular Hemoglobin Concentration (MCHC)?
|
Hemoglobin (g/dL) x100
--------------------------------- = MCHC Hematocrit |
|
|
What is the scientific term when red blood cells sometimes clump together?
|
AGGLUTINATE
When blood from one person is mixed with plasma from another person, the red blood cells will sometimes agglutinate, or clump together |
|
|
The antigen Rh factor was named because?
|
Rh factor wasnamed because it was first discovered in rhesus monkeys.
|
|
|
What is immunological competence?
|
Since the mother is Rh positive, her immune systerm cannot be stimulated to produce antibodies by the presence of an Rh positive fetus. The development of immunological competence does not occur until shortly after birth, so that an Rh negative fetus in an Rh positive mother would not yet have an immune response during normal gestation (pregnancy).
|
|
|
What is erythroblastosis fetalis and its properties? (*usually in pregnant women and concerning Rh + and - antibodies factors)
|
ERYTHROBLASTOSIS FETALIS
When an Rh negative mother is carrying an Rh positive fetus, some of the Rh antigens may enter her circulation when the placenta tears at birth (red blood cells do not normally cross the placenta during pregnancy). Because these red blood cells express an antigen (the Rh factor) foreign to the mother, her immune system will eventually be stimulated to produce antibodies capable of destroying the red blood cells of subsequent Rh positive fetuses, a condition known as hemolytic dis¬ ease of the newborn, or erythroblastosis fetalis. |
|
|
Erythroblastosis fetalis can be prevented by the administration of exogenous Rh antibodies known as ____________ (e.g., RhoGAM) to the mother within 72 hours after delivery.
|
Rho(D) immune globulin (e.g., RhoGAM)
Erythroblastosis fetalis can be prevented by the administration of exogenous Rh antibodies known as Rho(D) immune globulin (e.g., RhoGAM) to the mother within 72 hours after delivery. These antibodies prevent the Rh positive red blood cells that have entered the maternal circulation from stimulating an immune response in the mother. |
|
|
The most common blood types are type __ and type ____; the rarest is type ___ (table 6.1).
|

|
|
|
Show the antibody properties of Blood type A, B, O, and AB?
|
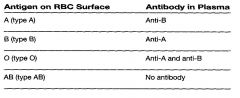
|
|
|
What is the order from biggest to smallest in percent of the following Blood Cells? Neutrophils, Eosinophils, Basophils, Lymphocytes, and monocytes.
|

|
|
|
What acronym would you use to remember the order from the Most to the least concentration of blood cells?
|
Never Let Me Eat Beans
Never = Neutrophils Let = Lymphocytes Me = Mesophils Eat = Esonophils Beans= Basophils |
|
|
What are Leukocytes?
|
White Blood Cells (5 types)
|
|
|
What are the 5 types of Leukocytes?
|
1.Neutrophils (polymorphonuclear)
2. Eosinophils 3. Basophils 4. Monocytes 5. Lymphocytes |
|
|
Which of the 5 types of Leukocytes (WBC) are granular?
|
1.Netrophils (Polymorphonuclear)
2. Eusinophils 3. Basophils NEVER EAT BEANS |
|
|
Which of the 5 types of Leukocytes (WBC) are non granular?
|
4. Monocytes
5.Lymphocytes MY LOVE |
|
|
What acronym is helpful when identifying the 5 Leukocytes (WBC) and their granular (1-3) and nongranular (4-5) classifications?
|
Never Eat Bean My Love
Never = Neutrophils Eat = Eosinophils Beans = Basophils My = Monocytes Love = Lymphocytes |
|
|
When finding venous pressure, how did we do it in lab and what were we trying to measure?
|

|
|
|
What is the standard mercury in mmHg count?
|
13.6 mmHg
|
|
|
What is the cuff we used to find blood pressure?
|
Sphygmomanometer
|
|
|
What is normal blood pressure?
systolic ----------- diastolic |
120
---------- 80 |
|
|
Arterial blood pressure is directly dependent on _________(the amount of blood pumped by the heart per minute) and _________ (the resistance to blood flow through the arterioles).
|
CARDIAC OUTPUT & PERIPHERAL RESISTANCE
Arterial blood pressure is directly dependent on cardiac output (the amount of blood pumped by the heart per minute) and peripheral resistance (the resistance to blood flow through the arterioles). |
|
|
What is cardiac output?
|
CARDIAC OUTPUT
The amount of blood pumped by the heart every minute. |
|
|
What is peripheral resistance?
|
PERIPHERAL RESISTANCE
The resistance to blood flow though arterioles. |
|
|
What is Laminar Flow?
|
LAMINAR FLOW
occurs when all parts of a fluid move in the same direction. Laminar means layered. |
|
|
What is Turbulent Flow?
|
TURBULENT FLOW
occurs when some parts of the fluid move in radial and circumferential directions, churning and mixing the blood. |
|
|
What are the sounds of Korotkoff? (names after the Nikolai S. Korotokoff the Russian physician who first described them)
|
KOROTKOFF SOUNDS
The 5 stages of sounds you hear when measuring blood pressure through a sphygmomanometer. |
|
|
The cuff pressure at which the first sound is heard (the beginning of phase 1) is the ________ pressure.
|
SYSTOLIC
The cuff pressure at which the first sound is heard (the beginning of phase 1) is the systolic pressure. |
|
|
The cuff pressure at which the sound becomes muffled (the beginning of phase 4) and the pressure at which the sound disappears (the beginning of phase 5) are taken as measurements of the _______ pressure.
|
DIASTOLIC
The cuff pressure at which the sound becomes muffled (the beginning of phase 4) and the pressure at which the sound disappears (the beginning of phase 5) are taken as measurements of the diastolic pressure. |
|
|
How do u calculate pulse pressure? (formula)
|
PULSE PRESSURE FORMULA
systolic - diastolic = Pulse Pressure (PP) |
|
|
What is the formula for Mean Arterial Pressure (MAP)?
|
Mean arterial pressure (MAP) is equal to the diastolic pressure plus one-third of the pulse pressure.
diastolic + 1/3 systolic = Mean Arterial Pressure (MAP) |
|
|
Describe hypertension and its classifications.
|
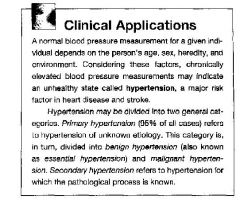
|
|
|
What are the ranges for systolic and diastolic pressure for prehypertension?
|
PREHYPERTENSION ranges
Systolic 120-139 mm Hg ----------------------------- Diastolic 80-89 mm Hg |
|
|
What are the ranges for systolic and diastolic pressure for stage 1 hypertension?
|
STAGE 1 HYPERTENSION ranges
Systolic 140-159 mm Hg ----------------------------- Diastolic 90-99 mm Hg |
|
|
What are the ranges for systolic and diastolic pressure for Stage 2 hypertension?
|
STAGE 2 HYPERTENSION ranges
Systolic 160+ mm Hg ----------------------------- Diastolic 100+ mm Hg |
|
|
What is ossitation?
|
OSSITATION
is listening |
|
|
When measuring venous pressure- what is the formula?
|
VENOUS PRESSURE FORMULA
Calculate your normal venous pressure in mmHg by dividing the measured distance between the points by 13.6. This is a needed adjustment since mercury has a density that is 13.6 times that of water |
|
|
What is the normal venous pressure?
|
Normal Venous Pressure
is between 4 and 10 mm Hg |
|
|
What is the difference between arteries and veins?
|
ARTERIES are more muscular and generally carry oxygen away from the lungs towards tissues.
VEINS carry deoxygenated blood from tissues to lungs. *with a few exceptions |
|
|
What are capillaries?
|
Capillaries are tiny blood vessels that pass blood from the arteries into the veins. They are very small, the largest being about 10 micrometers in diameter. Their walls are thin which allows materials to pass into the capillaries. Different types of capillaries exist and perform different functions for the body. Primarily, however, the capillaries are able to profuse the tissues of the body with needed oxygen and important nutrients supplied by blood.
|
|
|
What are starling forces and its properties? (*hint net change in what?)
|
STARLINGS FORCES (The Law of Capillaries)
There are many forces acting on capillaries that determine whether or not there will be a net change in the fluid passing through the capillary. These forces are often referred to as Starling's Forces (Starling's Law of the Capillaries) because he was the first scientist to elucidate the formula. |
|
|
What two forces promote filtration out of the capillary and into the interstitial fluid?
|
Two pressures promote filtration out of the capillary and into the interstitial fluid; blood hydrostatic pressure (BHP) and interstitial fluid osmotic pressure (IFOP).
|
|
|
What is the acronym BHP?
|
BLOOD HYDROSTATIC FLUID (BHP)
one of the two pressures that promote filtrations out into the capillary into the interstitial fluid. |
|
|
What is the acronym IFOP?
|
INTERSTITIAL FLUID OSMOTIC PRESSURE (IFOP)
one of the two pressures that promote filtrations out into the capillary into the interstitial fluid. |
|
|
What are the properties of BHP (blood hydrostatic Pressure)?
|
BHP (Blood Hysdrostatic Pressure) is the blood pressure in the capillaries and this force tends to push blood out of the capillaries. Because of the resistance to flow in the capillaries, this value is higher at the arterial end (beginning) of the capillary and lower and the venous end (ending) of the capillary.
|
|
|
What are the properties of of IFOP (interstitial Fluid Osmotic Pressure)
|
IFOP (Interstitial Fluid Osmotic Pressure) refers to the pulling action of proteins from the interstitial space. This tends to pull water out of the capillary into the interstitial fluid.
|
|
|
What are the two pressures that favor filtration ? (* ___ + ___ )
|
BHP (blood hydrostatic pressure) + IFOP (Interstitial Fluid Omostic Pressure)
Thus, the forces that favor filtration are known as BHP + IFOP. There are also two pressures that promote reabsorption into the capillary. |
|
|
What are two pressure that promote reabsorption into the capillary?
(*not BHP + IFOP) |
IFHP + BCOP
Interstitial Fluid Hydrostatic Pressure (IFHP) and Blood Colloid Osmotic Pressure (BCOP) |
|
|
What is IFHP?
|
Interstitial Fluid Hydrostatic Pressure
1) IFHP is the force that pushes against the capillary, keeping fluid inside. |
|
|
What is BCOP?
|
Blood Colloid Osmotic Pressure
2) while the BCOP is an osmotic force that pulls water back into the capillary. |
|
|
What are the two forces that favor absorption? (filtrations is favored by BHP + IFOP)
|
Interstitial Fluid Hydrostatic pressure and Blood Colloid Osmotic Pressure.
IFHP + BCOP favor reabsorption. |
|
|
What is NFP and its formula?
|
NET FILTRATION PRESSURE (NFP)
We can put these ideas together to calculate what the net filtration pressure (NFP) will be: NFP = (BHP + IFOP) - (BCOP + IFHP) |
|
|
What is an easier way to determine Net Filtration Pressure (NFP)?
|
FILTRATION - ABSORPTION = NFP
|
|
|
What is the calculation for filtration?
|
BHP + IFOP
Blood Hydrostatic Pressure + Interstitial Fluid Osmotic Pressure = Filtration |
|
|
What is the calculation for reabsorption?
|
IFHP + BCOP
Interstitial Fluid Hydrostatic Pressure + Bloof Colloid Osmotic Pressure = reabsorption |
|
|
What is an easier way to remember Starlings Forces and the different pressure?
|
( _HP + _ _ OP ) - ( _ _ HP + _ _ OP )
*both are hydrostatic pressure (HP) and Osmotic Pressure (OP) (B and IF) - (IF and BC) *like yoda says- b no if and if then BeCome |
|
|
What does it mean when you have positive (+) Net Filtration Pressure (NFP) and negative (-) NFP?
|
If the sign for NFP is positive, there is a net outward flow of fluid, while a negative NFP indicate net reabsorption.
|
|
|
Does it make sense that getting a negative NFP is reabsorption and positive NFP is outward flow?
|
YES
Negative is less and positive is more. |
|
|
Using Krotokoff sounds what pressure indicated systolic and diastolic sounds using a sphymomanometer?
|
First Sound is systolic
Last Sound is diastolic |
|
|
What is the average blood pressure or BP? (use systolic/ diastolic)
|
120/80 mmHg is considered normal BP
|
|
|
What is the formula for Venous Pressure?
|
distance/ 13.6 mmHg
normal is 4-12 in lab |
|
|
What is Lanthanic ?
|
LANTHANIC
is a silent disease type usually concerning hypertension |
|
|
What is Idiopatic?
|
IDIOPATIC
sounds like idiot and dont know where it comes from. |
|
|
What is the formula for PP (Pulse Pressure)? (use systolic and diastolic)
|
PP = S - D
Pulse pressure = Systolic - diastolic in mm Hg |
|
|
What is the magic number for Mercury (Hg) used in physiology?
|
13.6 mm Hg
|
|
|
True or False
Pulse Pressure (PP) is a good indicator of stroke? |
True high PP = High Risk of stroke
|
|
|
What is the formula for Mean Arterial Pressure (MAP)? (there are two)
|
1) MAP = 2/3 D + 1/3 S
2) MAP = 1/3 PP + D MAP answer is always between S & D S (Systolic) D (Diastolic) PP (Pulse Pressure) MAP (Mean Arterial Pressure) |
|
|
What is orthostatic pressure? (sounds like orthopedic beds)
|
ORTHOSTATIC PRESSURE
is hypertension with change in position. Like an orthopedic bed that moves with u as u sleep. |
|
|
What is the main function of the heart and what are its two circuits?
|
The main function of the heart is to pump blood through two circuits:
1. Pulmonary circuit: through the lungs to oxygenate the blood and remove carbon dioxide; and 2. Systemic circuit: to deliver oxygen and nutrients to tissues. |
|
|
What is function of the pulmonary circuit?
|
Pulmonary circuit: through the lungs to oxygenate the blood and remove carbon dioxide;
Like "Pulling factory" to get CO2 out and get O2 out to blood. |
|
|
What is the systemic circuit?
|
to deliver oxygen and nutrients to tissues.
The "delivery system" that delivers o2 and nutrients to tissues |
|
|
The heart needs 3 types of cell to beat- what are they?
|
1. rythm generators, 2. conductors, 3. contractile cells
In order to beat, the heart needs three types of cells: 1. Rhythm generators, which produce an electrical signal (SA node or normal pacemaker); 2. Conductors to spread the pacemaker signal; and 3. Contractile cells (myocardium) to mechanically pump blood. |
|
|
The heart needs these three cells (rhythm, conductors, and contractile) to beat- how can u remember these three cells?
|
The heart is like a battery used for remote control to make things go like RCC
Remote Control Cars = Rythm Conductors Contractiles or Conducts Rythms Contracts Rythms |
|
|
What kind of cells start depolarization and repolarization in the heart?
|
Pacemaker Cells
The heart has specialized pacemaker cells that start the electrical sequence of depolarization and repolarization. |
|
|
The property of cardiac tissue is called inherent rhythmicity or what?
|
AUTOMATICITY
This property of cardiac tissue is called inherent rhythmicity or automaticity. |
|
|
The electrical signal is generated by what node and spreads to the ventricular muscle via particular pathways and what fibers? ( one node, one path, one fiber, another node, one bundle and two branched bundles and one fiber)
*HINT SIAABBP |
SA NODE, INTERNODAL PATHWAY, ATRIAL FIBERS, AV Node, BUNDLE OF HIS, BUNDLE OF HIS RIGHT AND LEFT BRANCHES, AND PURKINJE FIBERS
The electrical signal is generated by the sinoatrial node (SA node) and spreads to the ventricular muscle via particular conducting pathways: internodal pathways and atrial fibers, the atrioventricular node (AV node), the bundle of His, the right and left bundle branches, Purkinje fibers . |
|
|
What is the acronym SIAABBP?
|
Some = SA NODE
Idiot = Internodal Pathway Accidentally= atrioventricular fibers Ate = AV Node Big = Bundle of His Bad = R/L Bundle Branches Pears = Purkinje Fiber |
|
|
What are the components of an ECG (electrocardiogram) wave?
|
P wave, QRS complex, T waves
(its alphabetical) |
|
|
What is the P wave?
|
The P wave results from atrial depolarization. (one event)
|
|
|
What is the QRS complex? (they are blips on the ECG wave)
|
The QRS complex is a result of ventricular depolarization and indicates the start of ventricular contraction and atrial repolarization. (2 events)
|
|
|
What is the T wave?
|
The T wave results from ventricular repolarization and signals the beginning, of ventricular relaxation.
|
|
|
What are the order or depolarization and repolarization that corresponds to PQRST waves? (AD VD AR VR)
|
P wave = 1event = Atrial Polarization
QRST complex = 2 event= Ventricular Depolarization and Atrial Repolarizatiojn T Wave= 1 event = Ventricular Polarization |
|
|
Simplify the event of depolarization and repolarization?
|
it is either Atrial or Ventricular depolarization or repolarization.
One letter wave = one event +2 letter waves = 2 events Thus AD VD AR VR with one eventin P wave, two events in QRS complex, and one event in T wave |
|
|
What is the ECG wave doing in terms of polarizing?
|
depolarize, depolarize, repolarize, repolarize
in either atrial and ventricular |
|
|
Segment (waves ) QT is systolic or diastolic?
|
Systolic
*QT is my sis (for systolic) |
|
|
Segment (waves) TQ is systolic or diastolic?
|
Diastolic
|
|
|
QT composes of 1/3 systolic and TQ 2/3 diastolic. Thus if QT = 0.30 then what is TQ?
|
TQ is diastolic and it is 0.60
twice the number of QT |
|
|
What is Plethysmography?
|
PLETHYSMOGRAPHY
The study of blood volume changes within an organ by using volume displacement techniques is known as plethysmography. |

