![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
99 Cards in this Set
- Front
- Back
|
dead space
|
1. part of a tidal volume that does not undergo alveolar ventilation
2 circle system is limited to the area distal to the point of inspiratory and expiratory gas mixing at the Y-piece. |
|
|
causes an increase in dead space
|
1. malfunctioning unidirectional valve will increase circuit dead space and allow rebreathing of expired CO2.
2. Humidifiers 3.ventilation lost to expansion of the breathing circuit during positive-pressure ventilation. 4. Physiologic due to mismatch in V/Q |
|
|
What is added from the alveoli
3 |
Carbon dioxide
Water vapor Gases from the body (methane, acetone, N2) |
|
|
Breathing Circuit Should allow rebreathing of
|
Oxygen not metabolized
Nitrous oxide or air Anesthetic agent |
|
|
Nitrous oxide increases (respiratory related)
|
increases respiratory rate (tachypnea) and decreases tidal volume as a result of central
nervous system stimulation and, perhaps, activation of pulmonary stretch receptors. The net effect is a minimal change in minute ventilation and resting arterial CO2 levels. |
|
|
Hypoxic drive, the ventilatory response
to arterial hypoxia that is mediated by |
peripheral chemoreceptors in the carotid bodies, is markedly
depressed by even small amounts of nitrous oxide. |
|
|
basic breathing rhythm originates in
|
in the medulla.
|
|
|
4 areas that control breathing
|
central respiratory center
peripheral chemoreceptors lung receptors effects of anesthesia |
|
|
areas influence the dorsal (inspiratory) medullary center
|
Two pontine areas,
A lower pontine (apneustic) center is excitatory, whereas an upper pontine (pneumotaxic) center is inhibitory. The pontine centers appear to fine tune respiratory rate and rhythm. |
|
|
Central chemoreceptors (Central Respiratory Centers) are thought to lie on
|
anterolateral surface of the medulla and
respond primarily to changes in cerebrospinal fluid (CSF) [H+]. |
|
|
the principal peripheral
chemoreceptors in humans |
The carotid bodies
are sensitive to changes in PaO2, PaCO2, pH, and arterial perfusion pressure |
|
|
the carotid bodies interact with central respiratory centers via the
|
glossopharyngeal nerves, producing reflex increases in
alveolar ventilation in response to reductions in PaO2, arterial perfusion, or elevations in [H+] and PaCO2. |
|
|
Hypoxic drive, the ventilatory response
to arterial hypoxia that is mediated by |
peripheral chemoreceptors in the carotid bodies, is markedly
depressed by even small amounts of nitrous oxide. |
|
|
Lung Receptors
|
Impulses from these receptors are carried centrally by the vagus nerve. Stretch receptors are distributed in the smooth muscle of airways; they are responsible for inhibition of inspiration when the lung is inflated to excessive volumes (Hering–Breuer inflation reflex) and shortening of exhalation when the lung is deflated
(deflation reflex). |
|
|
(Hering–Breuer inflation reflex
|
they are responsible for inhibition of inspiration when the lung is inflated to
excessive volumes |
|
|
functional residual capacity (FRC).
|
lung volume at the end of a normal exhalation
|
|
|
Induction of anesthesia (and FRC)
|
consistently produces an additional 15–20% reduction in FRC (400 ml in most
patients) beyond what occurs with the supine position alone. |
|
|
Central chemoreceptors are thought to lie on
|
the anterolateral surface of the medulla and respond
primarily to changes in cerebrospinal fluid [H+]. This mechanism is effective in regulating PaCO2, because the blood–brain barrier is permeable to dissolved CO2 but not to bicarbonate ions. |
|
|
principal function of the lungs is to allow
|
gas exchange between blood and inspired air.
|
|
|
Hypercarbia is often associated
|
with
hypertension. |
|
|
if lash reflex abolished then
|
eyelid reflex diminished
|
|
|
Inhalation agents lower
|
lower tidal volumes
increase respiratory rate |
|
|
Limbic System Stimulation 3 points
|
Anticipation of activity
Emotional anxiety Increases rate and depth of ventilation |
|
|
temperature and ventilation
4 points |
Increased temperature increases respiratory rate
Decreased temperature decreases respiratory rate Controlled ventilation recommended for febrile patient Controlled ventilation recommended for cold patient |
|
|
Pain and apnea
3 points |
Sudden severe pain causes apnea
Prolonged somatic pain increases respiratory rate Visceral pain decreases respiratory rate (deep abdominal pain) |
|
|
Stretching the Anal Sphincter
4 points |
Stimulates respiration
Consider intubating these cases Frequent episode laryngospasm Watch the surgeon and have patient deep |
|
|
general rule with intubation
|
do not want alot of stim
Take patient through Stage II gently or IV induction |
|
|
respiration
Sudden rise in blood pressure |
decreases respiration
|
|
|
respiration
Sudden drop in blood pressure |
increases respiration
|
|
|
Pleural cavity pressure always
|
subatmospheric
|
|
|
Diaphragm
2 points |
Skeletal muscle
Innervated from phrenic nerve C 3-4-5 |
|
|
Diffusing capacity for hemoglobin
|
Volume of a gas that diffused through membrane each minute for a pressure difference of 1 mmHg
Normally 21 ml/min/mmHg Mean oxygen pressure difference = 11 mmHg 21 ml/min/mmHg X 11 mmHg = 230 ml/min |
|
|
Basal metabolic oxygen consumption ( VO2) equals
|
10 times a patient's weight in kilograms to
the three-quarters power: |
|
|
Oxygen requirements decrease by 10%
|
for each degree below 37.6°C:
|
|
|
Increasing depth of anesthesia does not significantly alter basal metabolic rate
|
unless tissue perfusion is compromised.
|
|
|
Tidal volume = (formula)
|
500 ml or 7 cc/kg IBW
70% of TV reaches alveoli 30% does not-anatomic dead space |
|
|
Forceful exhalation =
|
expiratory reserve volume
Residual volume left over |
|
|
Functional residual capacity
|
The lung volume at the end of a normal exhalation
(expiratory reserve volume + Residual volume) Stays in lungs at end expiration |
|
|
Alveolar Ventilation =
|
Total volume of new gas entering each minute
AV = RR x (TV – dead space) |
|
|
Alveolar gas consists
|
Fresh gas - metabolized gas
Carbon dioxide Water vapor |
|
|
Slow Replacement of Alveolar Air?
|
Prevents sudden changes in gas concentration
Respiratory control more stable |
|
|
transport protein
|
albumin
|
|
|
goal blood pressure
|
20% of norm
|
|
|
Ventilation not necessary for ______, but necessary for removal ______.
|
oxygenation, CO2
High solubility necessitates removal |
|
|
CO2 produced dictates
|
dictates minute ventilation
i.e. Cardiopulmonary bypass (low levels) ECMO only exceptions |
|
|
Spontaneous breathing keeps PCO2
(can be affected by 3X) |
PCO2 - 40mmHg
Absence of disease (copd, smoker) High altitude and Pharmacologic intervention |
|
|
Carbon Dioxide Production
Resting adult produces |
.008 gm molecules/min
|
|
|
In the open system, the patient
|
inhales only the mixture
delivered by the anesthesia machine. Valves direct each exhaled breath into atmosphere. A reservoir bag mayor may not be present. Rebreathing is minimal, and there is no carbon dioxide absorption. |
|
|
In the semiopen system,
|
exhaled gases flow out of the
system and to the inspiratory line of the apparatus to be rebreathed. There is no chemical absorption of carbon dioxide. Rebreathing depends on the fresh gas flow. A reservoir bag and a directional valve are optional. |
|
|
In the semi-closed system,
|
part of the exhaled gases
passes into atmosphere and part mixes with fresh gases and is rebreathed. Chemical absorption of carbon dioxide, directional valves, and a reservoir bag are present |
|
|
In the closed system,
|
there is complete rebreathing
of expired gas. Carbon dioxide absorption, a reservoir bag, and directional valves are present. |
|
|
Open circuit
reservoir? rebreathing? example? |
reservoir? no
rebreathing? no example? open drop, insufflation, nasal cannula |
|
|
Semiopen
reservoir? rebreathing? example? |
reservoir? Yes
rebreathing? no example? nonrebreathing circuit or a circle at high fresh gas flows |
|
|
Semiclosed
reservoir? rebreathing? example? |
reservoir?Yes
rebreathing? Yes(partial) example? circle at fresh gas flow less that minute ventilation |
|
|
Closed
reservoir? rebreathing? example? |
reservoir?Yes
rebreathing? Yes complete example? circle at extremely low fresh gas flow with a adjustable pressure limiting valve closed |
|
|
(open) insufflation system is one in which gases are
5 points |
1. (blowing of gases across a patients face.
2 no contact airway or breathing circuit. 3. valuable with pediatric anesthesia 4. no rebreathing of exhaled gases if high flows are used. 5. ventilation not controlled. gases are delivered directly into the patient's airway. There are no valves, reservoir bag, or carbon dioxide absorption. |
|
|
insufflation usually denotes
|
the blowing of anesthetic gases across a patient's face.
|
|
|
open-drop anesthesia
|
highly volatile anesthetic, halothane—is dripped onto a gauze covered mask (Schimmelbusch mask) applied to the patient's face. As the patient inhales, air passes through the gauze, vaporizes the liquid agent, and carries high concentrations of anesthetic to the patient. (rebreathing may be significant)
|
|
|
4 Disadvantages of Open
|
poor control of inspired gas concentration and depth of anesthesia
inability to assist or control ventilation no conservation of exhaled heat or humidity pollution of OR with large volumes of waste gases |
|
|
Draw-over anesthesia 5 points
|
1 nonrebreathing circuits that use ambient air as carrier gas
2 can use supplemental O2 3 inspired vapor and O2 concentrations are predictable and controllable 4 allow IPPV and passive scavenging 5 allow CPAP and PEEP 6 low resistance vaporizers 7 never use N2O 8 may have low O2 saturation with room air |
|
|
Draw-over anesthesia pro and con
|
advantage: simple and portable
disadvantages: depth of TV not well known due to no rebreathing bag; awkward to use for ENT/head surgery due to components located near patient’s head |
|
|
used to prevent rebreathing of CO2
|
high FGF’s
|
|
|
3 performance characteristics of Mapleson
|
1 lightweight, inexpensive and simple
2 some rebreathing occurs (flow controls amount) 3 allow quick change in anesthetic concentration due to high FGF (key) |
|
|
Mapleson_____ best for spontaneous ventilation
|
A
|
|
|
Mapleson ____ best for controlled ventilation
|
D
|
|
|
Bain circuit is modification of_____
|
D
|
|
|
Mapleson best for Spontaneous ventilation __ __ __ __
|
(A, D, F, E )
|
|
|
Mapleson best for controlled ventilation ___ ___ ___ ___
|
(D, F, E, B, C )
|
|
|
6 Advantages of Mapleson system
|
Low resistance to breathing made them popular in pediatrics
Less work of breathing Simple, portable Easy to assemble Minimal moving parts Some retention heat & humidity |
|
|
6 Disadvantages of Mapleson
|
Most advantages overshadowed by need for high flow rates
Costs Dry & cold airway OR pollution Difficult to change from spontaneous to controlled ventilation Has led to many ‘modifications’ of Mapleson systems for modern use |
|
|
mapleson A, best for spontaneous
|
|

|
mapleson B
|
|
|
Mapleson C
|
|

|
Mapleson D (Bain)
|
|

|
mapleson E
|
|

|
mapleson F
|
|
|
Mapleson A system differs from the other Mapleson
systems in that |
fresh gas does not enter the system near
the patient connection but enters at the other end of the system near the reservoir bag. |
|
|
The Mapleson B system the
fresh gas inlet and APL valve are both located near |
patient port.
|
|
|
The Mapleson C system is identical to X except
|
except that the corrugated tubing is omitted
|
|
|
The Mapleson D system is popular because
|
excess gas scavenging is relatively easy, and it is the most efficient of the Mapleson systems during controlled ventilation.
|
|
|
Mapleson D system and peep
|
A bidirectional positive end-expiratory pressure
(PEEP) valve may be placed between the corrugated tubing and the APL valve |
|
|
In the Bain modification
|
the fresh gas supply
tube runs coaxially inside the corrugated tubing and ends at the point where the fresh gas would enter if the classic Mapleson D form were used |
|
|
Bain System Hazards
|
inner tube of the Bain system becomes detached
from its connections at either end or develops a leak at the machine end, if the fresh gas supply tube becomes kinked or twisted |
|
|
Semi-closed (Circle System)
5 points |
Most commonly used
Adults and pediatrics More complex but more efficient than Mapleson Prevents rebreathing of CO2 Allows use of low flows |
|

|
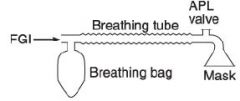
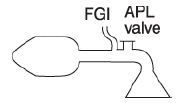
circle system with APL,
|
|
|
3 keys of closed system to prevent rebreathing
|
valve must be between patient and rebreathing bag on both inspir/expir limbs
FGF cannot enter circuit between expir. valve and patient APL cannot be located between patient and inspir. valve |
|
|
6 Valve ASTM Requirements
|
Flow direction shall be permanently marked
Functioning of valves should be visible Resistance of dry & moist valves shall not exceed a pressure drop of 0.15 kPa (1.5cmH2O) at 1L/second flow (60L/min-test flowrate for adults) Opening pressure of moist valve should not exceed 0.15 kPa (1.5cmH2O) Reverse flow shall not exceed 60mL/min at any pressure differential to 0.5 kPa (5cmH2O) Determined to be clinically acceptable & detectable with currently available volume monitors Valve shall not become dislocated with a reversed pressure differential of 5 kPa (50cmH2O) Maximum pressure in bag mode of circle system |
|
|
Malfunction of either valve may allow (3 things)
|
1. rebreathing of CO2, resulting in hypercapia
2. Faulty valve can lead to increased PIP’s or increased ETCO2 with elevated baseline on waveform 3. Increased resistance |
|
|
Incompetent Expiratory Valve
|
Capnograph shows ‘elevated baseline’
Baseline should always return to zero if you have no re-breathing Re-breathing occurring on expiratory limb of waveform Anatomic dead space exhaled at baseline Also look at inspired CO2 numeric – FiCO2 |
|
|
Incompetent Inspiratory Valve
|
Capnograph shows abnormal ‘beta angle’
Normal beta angle approximately 90° Re-breathing occurring during inspiration Shows on inspiratory side of waveform Shaded area represents approximately 180° beta |
|
|
Obstruction to Gas Flow
|
Disc damaged and jams valve seat
Disc lost during cleaning & not recovered Migrated down into bag mount or vent hose Functioned as one-way valve Gas could flow into circuit & patient Gas could not flow out Bilateral tension pneumothorax |
|
|
FDA Checkout 12.1:
|
Check for proper action of the unidirectional valves
|
|
|
Tubes of Breathing Circuit internal volume
|
400-500ml per meter
|
|
|
Always test circuit before using by determining oxygen flow required to maintain
|
30 cm H2O pressure in circuit
|
|
|
Dead space is
|
1. space in circuit occupied by gases that are rebreathed without any change in composition
2 Part of TV that doesn’t undergo alveolar ventilation 3 Dead space begins at Y piece and extends to any adapters distal to Y piece (distal limb of Y piece and any ETT or mask between it and patient’s airway) NOT at end of breathing circuit |
|
|
Common (Fresh) Gas Outlet
|
only one outlet that supplies gas to the circuit
adds new gas of fixed and known composition has anti-disconnect device used to prevent detachment of hose usually latex-free oxygen flush valve provides O2 to common gas outlet |
|
|
Fresh Gas Inlet
3 points |
1 gases (anesthetics with oxygen/air/nitrous) from the machine continuously enter the circuit through this inlet
2 placed between absorber and inspiratory valve 3 connected with flexible rubber tubing (delivery hose) |
|
|
Reservoir bag
6 points |
attached to bag mount
3 functions reservoir for anesthetic gases from which patient can inspire provide visual/tactile means of existence and of volume of ventilation serve as means for manual ventilation usually elliptical in shape nonslippery plastic or latex rubber sizes from 0.5 to 6L 3 L bag is usually sufficient for most adults ****think of breathing bag as patient’s lungs |
|
|
If high pressure alarm
|
disconnect patient from vent and bag till you find out what is wrong
|

