![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
84 Cards in this Set
- Front
- Back
|
It is a cold day outside and we feel dry skin. why? |
-an decrease in the amount of particles in the air is related to decreased water vapour pressure AND is related to decreased temperature bc T affects avg energy of particles. -why our skin feels dry = no water vapour
|
|
|
how can you explain condensation and evaporation in terms of Temp, pressure or energy? |
evap = some particles have ^ energy than the avg and these can escape the attractive forces holding the liquid together! (liquid to vapour) conden = transition from vapour to liquid due to cold air not being able to hold water, so water vapour pressure drops and vapour tuns into water |
|
|
it is a cold day outside and we see our own breath. Why? |
we inhale cold air with no water vapour (lwr T, lwr particles), but it mixes with our warm lungs, so when we blow out air we see much higher water vapour in the air! But the temperature outisde is still cold and it causes the warm lung air out of our body now to get colder, cold air can't sustain water vapour, so it condenses and turns into a liquid as water vapour pressure drops. |
|
|
how is respiratory naturally regulated via chemical control? |
-central chemoreceptors sense changes in lwr CO2 lvls (from exhaling) and pH (lwr from ^H+ from bicarbonate rxn) and force inhalalation -peripheral chemo. does the same but in addition monitors oxygen lvls if they are low. -huge but not small changes in core temp = more ventilation |
|
|
how is our respiratory naturally regulated via neural control? |
increase in lung volume from inhalation causes stretch receptors on lungs to force lungs to expire! -medulla oblangta naturally controls breathing rates, inspiratory neurons are stimulating, expiratory neurons are inhibiting -at rest = balance of exp and insp neurons -our cerebral cortex = voluntary changing breathing by affecting medulla -respiratory centrs involuntarily affect medulla. |
|
|
how is our respiratory regulated via muscles? |
-active muscles require more oxygen = ^breathing -diaphragm contracts and external intercostals involved during forced inspiratoin -dipaphgram relaxes internal ints, + abs invovled during forced exhalation
|
|
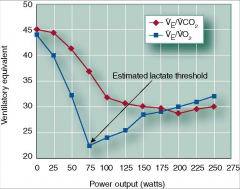
explain this graph! |
first few minutes of ex, oxygen consumption is increasing faster than ventilation! -this is due to affinity of O2 lwring, breathing isn't ^ yet. At 75 watts, ventilation increases ^ than O2 consumption but not CO2, this means that we are producing extra CO2 from krebs. or buffering from lactic acid, eventually CO2 = Ve so as Ve ^, CO2 ^. CO2 drives VENTILATION indepdenent to O2 |
|
|
what is the power output (in watts) that causes our ventilation to be ^ faster than O2 consumption? what is the significance of this? |
75 watts = our estimated lactate threshold! |
|
|
what is defined as the anaerobic threshold? |
it is our lactate threshold, our ventilatory thershold, they all mean the same. all occur at same point, and all mean that ventilation/vo2 + VCO2/VO2 increases without an increase in Ve/VCO2. |
|
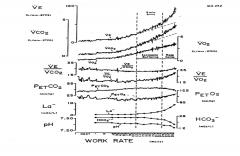
explain this graph! (slide 103) |
pet CO2 and O2 = how much is used during tidal volume for 1 breath. Ve VO2 and VCO2 (3) are per minute in the graph. pedaling with no load = very little effect on (3) as work rate, as load ^, wr^ and slow ^ in (3) eventually though Ve and VCO2 (2) are identically diff from (1) in that they are non-linear. Ve/VCO2 does not change all way through. Notice how pH, and bicarbonate decrease while La increases near the end. therefore pH IS MAIN DRIVE IN VENT! at the end petO2 also is increasing a lot faster than oxygen consumption, so therefore breathing frequency ^ and there is less time for CO2 to dissolve in bloodstream and go to lung causing less CO2 to be breathed out,
|
|
|
what is isocapnio buffering? |
same CO2 lvls are buffering -CO2 lvls aren't changing in the bloodstream even though we are above threshold |
|
|
what is respiratory compensation? |
bicarbonate lvls initally try to manage pH, but when we have run out of bicarbonate, pH gets lower as CO2 production increases and ventilation has to compensate and increase to manage pH lvls |
|
|
is ventilation a limiting facgtor for aerobic exercise? |
no!! bc Ve never approaches MVV (max voluntary vent) and the tidal volume never reaches vital capacity!!!. -only a limitation in very well trained athletes
|
|
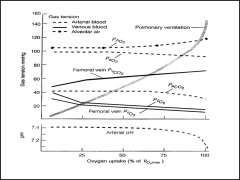
what does this graph indicate? |
it indicates that gas pressures are maintained during ex! (except for highly trained endurance atthletes) which further proves that ventilation is not a limiting factor to aerobic ex. |
|
|
what could be factors to maximal aerobic exercise that would limit it? |
-failure at oxygen delivery -rising pH levels from an increase in Lactate.
|
|
|
what is cardiac output (Q)? |
how well the oxygenated blood flows in the body. |
|
|
Can you explain how the lungs are involved during the record free dive attempt at 288 m? |
for the first 50 meters, due to buoyant forces, the person must swim below! thenas pressure ^ lung vol lwrs and he just falls! the opposite is true for when he starts to come up ! pressure decreases and lung volume increases as he floats up! |
|
|
Which vessels are cpacitance and which ones are resistance? why? |
veins = capacitance bc they have about 64% of the total blood volume! arteries = resistance vessels bc they can change their diameter dramatically! |
|
|
how much total blood volume would be in an avg human person? how much blood does the brain receive per minute? what about when you are using your cerebrum actively? |
5 L approx. -abt 715 ml -VO2 can dbl during cerebral activity! which means your brain needs lots of oxygen when it is doing a lot of thinking! |
|
|
how do you calculate VO2 in your body? |
HR x SV x the arterial venous oxygen difference (x amount of o2 arriving at working muscle - the amnt of o2 leaveing mscle) |
|
|
how does the conduction system of the heart go? |
1. An excitation signal (an action potential) is spontaneously created by the sinoatrial (SA) node. |
|
|
Which atria or ventricles get depolarized in which stages of PQRS? |
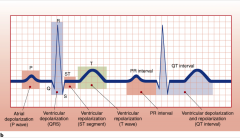
|
|
|
What is Bradycardia? Tachycardia? |
b: = slow heart rate (less than 60 bpm) t= fast. (more than 100) |
|
|
Why is MAP important? how do you calculate this? |
MAP = measure of driving force(how hard the heart works) as the Mean Arterial Pressure -very important for those who are hypertensive! = Dias BP + (0.33(sys BP - dias BP))
|
|
|
how often is the heart systole vs diastole? |
heart is systole 1/3 of the time, 2/3 of the time it is diastole! |
|
|
What does an echocardiography do? How should one use it? |
-measures chamber size and stroke vol. through the cardiac cycle! -once you find a good spot with good echo loighting, you should rotate in circles so you can find the spot and not go off course when investigating atria or venttricles specifically!
|
|
|
What is Hypertrophic Myopathy? how does it occur? why is it bad? |
-most common cause of sudden death in young -genetic disoder -myofibrillar dissaray= mscle fibers shorten but they are all oriented differently so you don't get your blood ejected properly |
|
|
why can we hold our breath longer after hyperventilating rather than not? |
it tkaes longer for CO2 lvls to reach the point where you have to breath again because you got rid of a lot of them via hyperventilating! |
|
|
what is the rate pressure product? |
RPP= estimate of cardiac work from Systolic BP x HR |
|
|
where will there be the most blood pressure in the body after leaving the heart? |
brachial arteries due to being at the same lvl as the heart! |
|
|
what are the respective values of normal circulation systole and diastole blood pressure as well as pulmonary circulation? both at rest any changes to the values when at maximum aerobic ex.? |
n: s: 120 d:80 p: s:25 d:10
max systol = 200 |
|
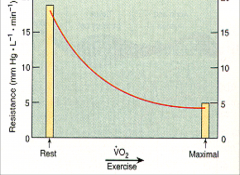
what caused the resistance to exponentially decrease during max ex? |
A decrease in Total Peripheral Resistance! causes increased flow of blood which lowers resistnace! it drops dramatically bc (Q = Pxr^4/lengthx viscosity) the radius has an exponent to it! therefore the radius increases causing a dramatic effect on blood flow |
|
|
how can you change your VO2 if desired? |
you can't really change heart rate but you can change stroke volume! |
|
|
what are some of the factors that affect stroke volume? |
by increasing Contractility, which is done by ^ symp stimulation by sending signals directly to SA node and ventricular tissue + secreting EP and Nep. -^ your ejection fraction (EF) this is caused by ejecting most of your EDV (blood filled) causing a lower ESV which ^ SV!
|
|
|
What is Contractility? |
force at which heart contracts |
|
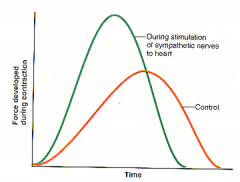
what does this graph mean? |
it means that when your heart is sympathetically activated, it results in a increased force in less time which causes storke volume to increase! |
|
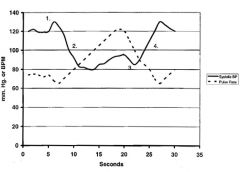
Explain this graph. |
That is valsalva! which the isometric contraction of your muscles while you are holding your breath in and exhaling! slight increase of BP bc it is exhalation. then a moderate decreae in BP due to muscles contracting and blocking venous pathway back to the heart! Then the increase in BP once you relax may cause you to feel dizzy :) 3= a slight BP drop because vessels re-expand as heart is filled. |
|
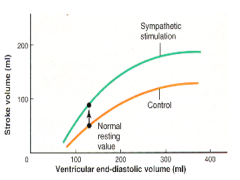
explain. |
intially as you ^ EDV there will be a linear ^ in SV but then it lvls off! (keep in mind ESV ^ always, but may ^ in diff proportions) in the presence of sympathetic activation though, EDV remains the same but SV changes which means ESV must be dramatically lower |
|
|
why do venous tone? Ventricular size? Distensiblity and resp pump affect EDV? |
1.venous tone (more tone = constrictoin of surrounding veins which brings more pre-load which ^ EDV) 2.^ventricular size = ^ EDV 3. ^distensibility = ^ EDV and lwr pressure. (ability of myocardium to stretch under pressure) 4.Resp pump (when exhaling, lung vol lwrs ^ pressure by pushing against veins ^ EDV) |
|
|
how does the muscle pump and the venous valves affect EDV? |
larger muscles (or contracting) squishes veins which ^ EDV venous valves help blood flow up from the legs in one direction, if these didn't work = vericose veins |
|
|
What is Hydrostatic load and how does that affect stroke volume? |
ability of blood to return to herat depending on body position! easier to do if lying down! lying down causes an ^ in SV but lwr HR! |
|
|
What is a coronary bipass? |
a blockage in one coronary artery can be fixed by planting a new "bipass" artery in front of the blockage and returning it to the direction of travel! |
|
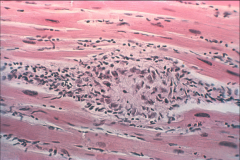
What is this? and what is it due to? |
a narcosis develops from a coronary bipass due to hypoxia. Essentially this is a wound and scar which causes the surrounding myocardium tissue to not shorten causing a lwr SV |
|
|
why is it easier to return blood when supine? how does the hydrostatic load affect SV overall? |
standing up causes a lwring of ESV but a GREATER lwring of EDV. lwring of ESV is due to it being easier to pump blood out of the heart because of gravity's help! Standing up will essentially cause a 10% difference in SV |
|
|
You have a HR of 180, and you have a 8mls/beat change in Stroke volume difference 1.What is your cardiac output? 2.how much of that blood per 100 ml is O2? 3.how much of that blood is O2? 4.how many more watts of work do you do aerobically? |
1.Q = 1.44L 2. 14 g Hb/100 ml in the blood x (1.34mlo2/gram of Hb) = 18.76 mls O2/100ml 3. 18.76 x 14.4 (unit conversion (L-> 100ml) = 270.14 4. 10 mlO2/min/watt x 270.14(unit conversion 100 ml-> ml) = 27 watts more work |
|
|
how does stroke volume differ based on your athleticism? |
higher lvl elite ahtletes have a linear relationship with heart rate and stroke volume so they can do less ananerobic work and just keep going! other athletes or unatthletic not so much! (it increases linearly but levels off at 40-60% VO2 max) |
|
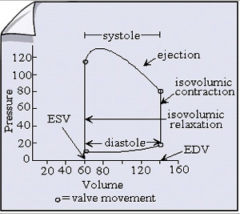
explain! |
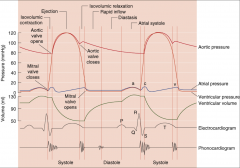
as your heart is filling, and getting close to EDV there is very little change in pressure from 60-120. Once at 120, the heart is trying to generate a huge pressure and it is pushing againt the valvesreally hard even though vol. not changing. once at 80mmHg blood leaves, pressure still ^! but once heart repolarizes volume still doesn't change until ESV. cycle repeats! |
|
|
pre-load vs afterload? (what they are) |
pre-load = volume at EDV (vol you will move in circ.) afterload = pressure ventircle has to generate b4 ejecting blood(resistance to BF) as AL^ heart will not generate enough pressure and blood flow will go down which lwrs Q! (bad for ppl who have hypertension!) |
|
|
how does pre-load and afterload affect BP? how would have the loads been affected? |
^ afterload increases both systolic and diastolic pressure! ^ in pre-load ^ only systolic which is ok, it is the afterload which is the problem. easiest way to increase pre and after loads are to ^ resistance in vessels! |
|
|
What is the Or flow formula? what can we manipulate for exercise purposes? What is the normal flow formula? |
Pressure x r^4/(length x viscosity)
-we can't change length
Pressure/resistance |
|
|
in normal blood what are the %'s of the comonents that make up the blood? |
55% plasma (90 H20, 7 plasma proteins, 3 other) 45% formed elements (99 RBC and 1 WBC and platelets |
|
|
How would one practically change their viscosity? |
1. hemoconcentration (plasma vol lwrs which ^ conc.. of RBC's. e.g. when sweating you are losing water from the plasma and you get more viscous) 2.Blood Doping (freeze RBC's and inject, your heart has to pump harder as a result! bc blood is more viscous) 3.EPO (from kidneys or bone marrow = stimulates RBC growth) |
|
|
what is hematocrit? what is its significance? |
hematocrit = % of blood volume composed of cells any ^ in hematrocrit ^ viscosity |
|
|
what is anemia? |
it is when you are low on Hb which puts emphasis on plasma protein and water contnet in blood |
|
|
What is the Frank-Starling Mechanism? |
energy of contraction is proportional to the length of the fibers in the heart!, causes an increase in EDV and ventricular stretch as well as a lwr ESV! |
|
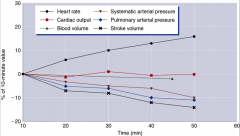
explain this type of graph!!! |
this graph represents cardio. drift at steady state, it shows that cardiac output remains the same as time increases but heart rate ^ and Stroke vol lwrs, this makes sense as the muscle requires more blood so total blood vol. lwrs! Overtime, This makes arterial radius ^ causing lower arterial pressure thrfre less blood to return to the heart thereby reducing EDV! |
|
|
If you are running a longer marathon... how would the ex. heat, and duration affect cardiovascular drift? |
as temperature (outside and our core body temperature) continues to increase, our ability to saturate O2 to Hb is decreasing so at any given time, when the blood is pumped, there is less cardiac output as less O2 is being delievered. |
|
|
What would be the difference in blood pressure between aerobic feata like Rick Hansen vs Linda Jackson? |
at both systolic and diastole, BP is ^ for arm work than leg work, reason why is that the arteries and veins are much smaller in the arms than the legs! |
|
|
What is Fick's Equation? and how would it influence cardio. work? |
VO2 = HR x SV x (a-VO2 diff)
-as CO ^ O2 consumption ^ since a-VO2 diff essentially measures oxygen extraction. |
|
|
how does oxygen extraction from Hb differ between resting and exercise? How does this relate to a-VO2 diff? |
at rest only 25% of avaialbe O2 is being used as ex ^ extraction of O2 ^ -relates as the capillaries carry more blood in ex while the veins carry less blood back to the heart therefore causing an increase in a-Vo2 diff causing an increae in Cardiac ouput! |
|
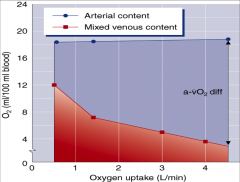
explain this graph. |
as ex^ you can see a-vo2 diff becoming bigger and bigger, but notice the steep slope initially during lower state ex. this Relates to a resp graph that shows VE/O2, essetially the body is consuming O2 a lot faster than ventilation bc the body is extracting it rather than ingesting it from the air! |
|
|
how does a-vo2 diff compare from a trained athlete and an untrained athlete? |
if you are an endurance runner your resting values of CO and a-vo2 diff will be the same as an untrained athlete. the main difference is that endurance atheltes have more lean mscle mass requiring more oxygen to be kept in muscles causing ^ a-vo2 diff which causes an increase in stroke volume due to ESV being lower than b4. which causes an increase in VO2 (CO) |
|
explain this graph. How would it change in the concept of ex? |
pressure drives everything, notice that there is a delay in depol and contraction as well as repol and relaxation of the heart! Also, if you look at ventricular volume, 80% of ventricular filling is passive, once the atria contracts it is that last (20%) that gets filled. This is why venous return is impnt bc the heart can only re-fill so much due to contractions! -if you look at aorta pressure it is always high due to blood flow always being continuous, even when ventricles are empty! -know there is periods of isovolumetric pressure ^. -during ex. all of this would be more compressed together occuring quicker. |
|
|
what is angioplasty? |
it is the widening of blocked arteries! |
|
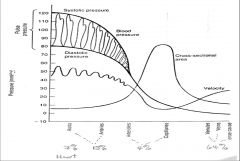
explain this graph! |
keep in mind that while we have normal BP (120-80), and even though velocity changes we still have continous flow during the system! -the further we get away from the heart = less pressure and less velocity but ^ x sectional area (capillaires) -low blood velocity in caps. bc oxygen needs time to diffuse, even during ^ ex int. blood is slow in caps. |
|
|
How does blood flow distribution afffect a-vo2 diff? also how does blood vol affect a-vo2 diff? |
a-vo2 diff is better due to blood flow distribution, dlood distribution is set up as parallel vascular beds, which can easily help change flow of the blood to other parts of the body if it needs to!
-more blood can result in a higher a-vo2 diff! |
|
|
Regarding to the relative distribution of blood flow, where does blood flow in comparison to at rest up to maximal ex? |
-very high initially in liver, kidneys, but cardiac output to myocardium is small! blood to the muscle is also high *as ex ^ to max, skel and cardio mscle BF increases more! -cerebral BF does not change at alll! -renal and kidney BF reduces, and skin increases up until maximum.
|
|
|
why does the skin need lots of blood flow during heavy ex? but not so much during maximal ex? |
as ex ^, blood needs to go to the skin so we can dissipate heat! but when at maximal, it is more impnt for the heart and mscle to receive BF, so BF to the skin reduces dramatically! |
|
|
Explain how the distribution of BF relates to thermoregulation? |
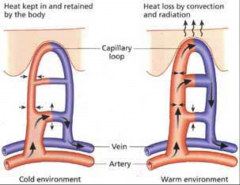
-we re-distribute heat from the core body to the periphery depending on the situation!
|
|
|
How are arterioles related to the principle of bloodflow distribution? how are they controled? |
arterioles are what controls flow to the parallel vascualr beds (capillaries), arterioles are controled by extrinsic neural control firstly, THEN autoregulation |
|
|
with regards to distribution of blood flow, how does vasoconstriction and vasodilatoin influence BF? when does VC and VD occur? any other names for VC or VD? why does VC and VD occur? http://www.livestrong.com/article/429813-what-happens-to-your-vessels-when-you-exercise/ |
VD cholinergic) allows more O2 blood to be delivered to the muscles. Acetycholine is an NT that is secreted allowing more VC. -Symp. = widespread VC (adrenergic) through whole body. The chemical byproducts produced by working muscles override this response where necessary. |
|
|
how does extrinsic neural control affect arterioles and bloodflow distribution? |
it causes an ^ in symp. tone which results in ^ in H.R. therefore maintaining CO! as well, it causes ^ in arterial vasomotor tone which causes more resistance inside the vessel, so for BP to be maintained, blood pressure has to increase (^ afterload as well) which forces blood flow! remember arterial pressure decreases in CV drift! |
|
|
how does autoregulation affect arterioles and bloodflow distribution? |
autoregulation influences the local factors affecting BF! for example when the body senses that it is low in oxygen or other related metabolites, the working tissue has receptors that facilitate vasodilation!. These receptors have a DIRECT EFFECT. non-working tissue also have receptors which increases VC causing an INDIRECT EFFECT! |
|
|
what factors can receptors in the muscle cause a direct effect on vasoconstriction? |
lwr oxygen, ^CO2 lvls , ^ temperature, lwr pH, ^ potassium, ^ nitric oxide, and adenosine |
|
|
What are Intrinisc ways we can have Cardiac Control? |
*Frank starling mechanism: ^ length of myocardium tissue ^ contractibility, also the ^ in EDV can stretch the ventricles (^ in length of myocardium) causing a greater contractility which ^ Stroke volume (and coincidently heart rate) |
|
|
how does the ANS affect cardiac control?? how do well trained athletes affect their cardiac ctonrol extrinsically? |
Symp: catecholines cause ^ in HR and contractility which lwrs ESV bc PS: vagus nerve can stimulate lwrd heart rate when acetycholine (cholinergic) is present which vasodilates vessels! *Trained = lwr HR due to ^ PS and lwr Symp, causes by ^ SV! |
|
|
what are extrrinsic factors that affect cardiac control? |
ANS, baro + chemoreceptors |
|
|
how do baro and chemoreceptors affect cardiac control? |
baro: -in aortic arch and carotid sinus, respond to changes in pressure, chemo: alter CO in response to lower O2, ^ CO2 and lwr pH |
|
|
Perforation vs ventilation |
vent:moving gases in and mixing with the alveolus perf: blood flowing through the vasculature! |
|
|
Whatis the functional residual capacity? |
FRC: ncludes the expiratory reserve volume and the residual volume. The FRC measures the amount of additional air that can be exhaled after a normal exhalation.
there is always some air left in the lungs after a maxexhalation. If RV didn't exist, lung tissues would stick together. The energy necessary to re-inflate the lung could be too great to overcome. Therefore, there is always some air remaining in the lungs. Residual volume is also important for preventing large fluctuations in respiratory gases (O2 and CO2). The residual volume is the only lung volume that cannot be measured directly
|
|
|
what is the purpose of residual volume? how does residual volume change? |
there is always some air left in the lungs after a maxexhalation. If RV didn't exist, lung tissues would stick together. The energy necessary to re-inflate the lung could be too great to overcome. Therefore, there is always some air remaining in the lungs. Residual volme is also important for preventing large fluctuations in respiratory gases (O2 and CO2). The residual volume is the only lung volume that cannot be measured directly. AS we age, our lungs are less resilient and our residual volume increases! |
|
|
What are the factors affecting gas exchange? |
1. an ^ partial pressure grad. (greatest one) 2. Hb and Mb conc. 3.diffusion and diffusion path length (longer length is = more resp) |
|
|
what is the difference between cardiac output and vo2 calculations? |
Q =HR x SV VO2= HR x SV x a-vo2 diff |
|
|
what is the main differnece between Heart rate and ventilation when exercise increases? |
heart rate always increases linearly, ventilation does so too but at a certain point, the slope changes A LOT! |

