![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
|
Evidence-based medicine : define
|
uses the best available evidence from published research as the foundation for clinical decision making.
|
|
|
What is the benefit of evidence based practice?
|
1) clinical expertise
2) respect for patient preference 3) aides the physician in providing optimal outcomes and a quality of life for the patient. |
|
|
What is a con for evidence based practice?
|
1) strain the ability of a society to fund and provide such services.
2) Critical appraisal of both new and traditional diagnostic and treatment modalities is thus needed. |
|
|
What two categories can research studies can be divided into?
|
PRIMARY
SECONDARY |
|
|
Name the types of Primary research studies.
|
Randomized control
Case control Cohort studies Cross sectional Case series Case report |
|
|
Name the type of Secondary research studies.
|
Meta-analyses
Clinical practice guidelines Decision analysis Cost-effectiveness analysis |
|
|
Primary Study: Randomized Control: define
|
participants in the trial are randomly allocated to one intervention or another.
Both groups are followed for a specified period and analyzed in terms of specific outcomes defined at the outset of the study A study in which people are allocated at random (by chance alone) to receive one of several clinical interventions. One of these interventions is the standard of comparison or control. The control may be a standard practice, a placebo ("sugar pill"), or no intervention at all. Someone who takes part in a randomized controlled trial (RCT) is called a participant or subject. RCTs seek to measure and compare the outcomes after the participants receive the interventions. Because the outcomes are measured, RCTs are quantitative studies |
|
|
Primary Study: Randomized Control: pros
|
allows rigorous assessment of a single variable in a defined patient group
has a prospective design that potentially eradicates bias by comparing two otherwise similar groups allows for meta-analysis. |
|
|
Primary Study: Randomized Control: cons
|
these studies are expensive and time-consuming.
|
|
|
Primary Study: Randomized Control: example
|
Women's Health Initiative randomized controlled trial.
This study was designed to assess the risks and benefits for postmenopausal hormone use in healthy women. However, the trial was stopped early because of an increased incidence of breast cancer, coronary heart disease, stroke, and thromboembolic disease in the hormone-treated group. |
|
|
Primary Study: Case Control: define
|
involves patients with a particular disease or condition who are identified and matched with control patients.
The control participants can be patients with another disease or individuals from the general population. The validity of these retrospective studies depends on careful selection of the control group. A study that compares patients who have a disease or outcome of interest (cases) with patients who do not have the disease or outcome (controls), and looks back retrospectively to compare how frequently the exposure to a risk factor is present in each group to determine the relationship between the risk factor and the disease. Case control studies are observational because no intervention is attempted and no attempt is made to alter the course of the disease. The goal is to retrospectively determine the exposure to the risk factor of interest from each of the two groups of individuals: cases and controls. These studies are designed to estimate odds. Case control studies are also known as "retrospective studies" and "case-referent studies." |
|
|
Primary Study: Case Control: example
|
CARDIO 2000 Study.
The authors evaluated 848 hospitalized patients after their first episode of acute coronary syndrome and used 1078 age- and sex-matched controls. The data revealed that women experiencing their first event were significantly older than men. |
|
|
Primary Study: Cohort Studies: Define
|
have two or more groups of participants selected on the basis of differences in their exposure to a particular agent.
The participants are prospectively followed to see how many in each group develop a disease or other specific outcome. A study design where one or more samples (called cohorts) are followed prospectively and subsequent status evaluations with respect to a disease or outcome are conducted to determine which initial participants exposure characteristics (risk factors) are associated with it. As the study is conducted, outcome from participants in each cohort is measured and relationships with specific characteristics determined |
|
|
Primary Study: Cohort Studies: Example
|
A well-known example is the Framingham Heart Study that enrolled 5200 participants in 1948 and followed them forward in time to examine the progression and risk factors for heart disease. The data provided from the Framingham Study have helped clinicians understand the development and progression of heart disease and its risk factors.
|
|
|
Primary Study: Cohort Studies: cons
|
As with randomized trials, cohort studies are time-consuming.
|
|
|
Primary Study: Cross sectional: define
|
This type of study utilizes different groups of people who differ in the variable of interest, but share other characteristics such as socioeconomic status, educational background, and ethnicity.
For example, researchers studying developmental psychology might select groups of people who are remarkably similar in most areas, but differ only in age. By doing this, any differences between groups can presumably be attributed to age differences rather than to other variables. |
|
|
Primary Study: Case Series: Define
|
When medical histories of more than one patient with a particular condition are described together to illustrate one aspect of the disease process
A case series (also known as a clinical series) is a medical research study that tracks patients with a known exposure given similar treatment or examines their medical records for exposure and outcome. |
|
|
Primary Study: Case Report
|
describe the medical history of a single patient.
An article that describes and interprets an individual case, often written in the form of a detailed story. Case reports often describe: Case reports are considered the lowest level of evidence, but they are also the first line of evidence, because they are where new issues and ideas emerge. This is why they form the base of our pyramid. A good case report will be clear about the importance of the observation being reported. |
|
|
Define Secondary (integrative studies)
|
Secondary (integrative) studies attempt to summarize and draw conclusions from primary information.
|
|
|
Secondary Study: Meta analysis: define
|
Uses statistical techniques to combine and summarize the results of primary studies.
A subset of systematic reviews; a method for systematically combining pertinent qualitative and quantitative study data from several selected studies to develop a single conclusion that has greater statistical power. This conclusion is statistically stronger than the analysis of any single study, due to increased numbers of subjects, greater diversity among subjects, or accumulated effects and results. |
|
|
Secondary Study: Meta analysis: pros
|
By combining the results from many trials, meta-analyses are able to estimate the magnitude of the effect of an intervention or risk factor as well as evaluate previously unanswered questions by performing subgroup analyses.
|
|
|
Secondary Study: Meta analysis: cons
|
i. The use of meta-analysis has provoked some controversy.
ii. Some investigators believe that meta-analyses may be as reliable as randomized controlled trials, whereas others believe that the technique should be used only as an alternate to randomized trials. However, in the absence of a large randomized controlled study, a meta-analysis of multiple smaller studies may be the best source of information to answer a specific question. |
|
|
Secondary Study: Clinical Practice Guidelines
|
attempt to summarize diagnostic and treatment strategies for common clinical problems to assist the physician with specific circumstances.
They are usually published by medical organizations, such as the American College of Physicians, and government agencies, such as the Agency for Health Care Policy and Research and the United States Preventive Services Task Force. |
|
|
Secondary Study: Cost effectiveness analysis
|
evaluates whether a particular course of action is an effective use of resources.
|
|
|
Define: Screening tests
|
performed on asymptomatic healthy people to detect occult disease
Screening tests are most useful when a high prevalence of disease is present in the population and the test has adequate sensitivity and specificity parameters. When applied to a disease with low prevalence, a test with low specificity would have an unacceptable number of false-positive results, which would lead to further procedures that are often invasive and expensive. |
|
|
What are the requirements of a screening test?
|
Prevalence of disease must be sufficiently high.
Disease must have significant morbidity and mortality rates. Effective treatment must be available. Improved outcomes from early diagnosis and treatment must be present. Test should have good sensitivity and specificity parameters. Test should carry acceptable risks and be cost-effective. |
|
|
Diagnostic tests
|
Used to determine the cause of illness in symptomatic persons and can be helpful in patient management by evaluating the severity of disease, determining prognosis, detecting disease recurrence, or selecting appropriate medications or other therapies.
When considering diagnostic tests, the physician should weigh the potential benefits against the risks and expense. |
|
|
Define: Sensitivity
|
an index of the diagnostic test's ability to detect the disease when it is present.
|
|
|
Define: Specificity
|
is the ability of the diagnostic test to identify correctly the absence of the disease.
|
|
|
Define; Likelihood ratio
|
uses both sensitivity and specificity, and gives an even better indication of the test's performance.
A high positive likelihood ratio indicates a high likelihood of the presence of disease, whereas a high negative likelihood ratio identifies the absence of disease. |
|
|
Positive likelihood ratio
|
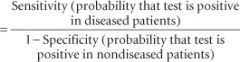
|
|
|
Negative likelihood ratio
|
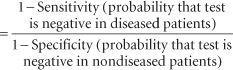
|
|
|
Quality of life
|
the subjective perception of the patient and includes physical, emotional, social, and cognitive functions and the disease symptoms and side effects of a given treatment or intervention.
For example, in examining the efficacy of a drug for postchemotherapy anemia, it would not only be important to know whether the hemoglobin rises appropriately but also to know whether the patient subjectively has more energy and is able to perform the normal duties of life. |

