![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
|
Define and tell what initiates primary peristalsis versus secondary peristalsis.
|
Primary peristalsis: peristalsis wave that occurs directly after swallowing
Secondary peristalsis: peristalsis elicited by esophageal distention, executed entirely by a local intramural reflex. Its physiologic role is to clear the esophagus of food residues and refluxed materials by moving them to the stomach. A swallow initiates primary peristalsis, whereas secondary peristalsis can be initiated at any level of the esophagus in response to local luminal stimuli such as acid or distention. |
|
|
Regarding esophageal symptoms, define each:
A. dysphagia B. odynophagia C. pyrosis D. globus sensation |
A. dysphagia - difficulty swallowing. 2 types: oropharyngeal dysphagia (transfer dysphagia, inability to initiate swallow or transfer thru pharynx) and esophageal dysphagia (transport dysphagia)
B. odynophagia - pain with swallowing C. pyrosis - heartburn D. globus sensation - feeling a lump or tightness in the throat, unrelated to swallowing |
|
|
There are two types of dysphagia. Name em. Which one is the one more commonly seen in older persons and is usually caused by striated muscle dzs or neurological dsorders and various local structural lesions?
|
2 types: oropharyngeal dysphagia or esophageal dysphagia
That description is oropharyngeal dysphagia, commonly seen with neuromuscular dzs like: CVA esp. stroke, multiple sclerosis, ALS, Parkinson's Dz. Mechanical obstruction in oropharyngeal type is mainly Zenker's diverticulum. |
|
|
Name the common causes of oropharyngeal dysphagia and esophageal dysphagia.
|
Oropharyngeal dysphagia:
Neuromuscular cause- CVA (esp stroke), MS, ALS, Parkinson's dz Mechanical obstruction cause - Zenker's diverticulum Esophageal dysphagia: Mechanical - Webs, rings, strictures, diverticula, eosinophilic esophagitis, congenital malformations, cancers, achalasia |
|
|
True or False:
Zenker's diverticulum is a mechanical cause of esophageal dysphagia. |
FALSE.
Zenker's diverticulum is a mechanical cause of OROPHARYNGEAL dysphagia, one of two types of dysphagia in the esophagus. Zenker's diverticulum is in the elderly population just above the UES! Food can get stuck here and cause halitosis. Other associated symptoms: aspiration and coughing a lot. |
|
|
Which of the following is FALSE about odynophagia?
A. Odynophagia is usually seen only with immunocompromised patients. B. Odynophagia can be caused by meds like quinidine, tetracycline, ferrous sulphate, NSAIDs C. Can manifest as dull retrosternal ache on swallowing to a stabbing pain with radiation to the back D. All of the above a true. |
D. All of the above a true.
|
|
|
Odynophagia is usually only seen with immunocompromised patients or with certain medicines. What are the common pill induced esophagitis causes (4) and infectious esophagitis causers (4).
|
Causes of odynophagia from pills: Quinidine, Tetracycline, Ferrous Sulphate, NSAIDs.
Causes of odynophagia from infections: HIV< CMV< HSV, Candida |
|
|
True or False:
Esophageal disorders are probably the most common causes of non-cardiac chest pain. |
True
|
|
|
What are hiatal hernias and differentiate between the four types.
|
Hiatal hernia is herniation of gastroesophageal junction and/or stomach through diaphragmatic hiatus.
Type 1: sliding herina (~95% of cases), is where the G junction is above diaphragmatic hiatus and stomach is pulled up Type 2: paraesophageal hernia, is where G junction is at correct place but a part of fundus pouch is above diaphragmatic hiatus. Type 3: elements of both Type I and II Type 4: herniation of other organs like colon, small intestine, etc. |
|
|
What is/are the classic symptom (1) , associated symptoms (5), and extra esophageal manifestations (4) associated with GERD?
|
Classic = heartburn
Ass. sympts = dysphagia, odynophagia, regurg, water brash, belching Extra-esophageal sympts = hoarseness, laryngitis, asthma, chronic cough |
|
|
WIth GERD and subsequent esophagitis, what is the strongest predictor of the severity of esophagitis?
A. how hypotensive LES is B. acidic potency of the refluxate C. size of the hiatal hernia |
C. size of the hiatal hernia
|
|
|
What are complications of long-standing GERD? (3)
|
- Peptic ulceration
- strictures - development of Barrett's esophagus (metaplastic columnar epithelium replaces the normal squamous epithelium of the distal esophagus) |
|
|
Which of the following IS NOT AN appropriate management options for GERD?
A. Weight loss for overweight or obese patients B. Avoiding late meals or meals prior to betime C. Avoiding specific foods (varies by patient) D. Proton pump inhibitors like Omeprazole E. Steroids like Fluticasone |
E. Steroids like Fluticasone
|
|
|
In Barrett's esophagus, what histological changes do we see and what are you at higher risk for?
|
With Barrett's esophagus, we see intestinal metaplasia dn goblet cells in the esophagus. Comes with a risk of adenocarcinoma.
|
|
|
___________ is an inflammatory disorder of the esophagus characterized by symptoms of esophageal dysfunction in association with histologic evidence of eosinophilic infiltration of the esophageal mucosa.
|
Eosinophilic esophagitis, aka asthma of the esophagus
Diagnosis is based on seeing 15 eosinophils per high power field in absence of GERD. (Unlike the rest of the GI tract, normally the esophagus does NOT have any resident eosinophils.) Diagnosis is also supported by a family history of EE and other allergy-based disorders like asthma, seasonal allergies. |
|

What condition is depicted and what is the treatment?
|
Eosinophilic esophagitis, "asthma of the esophagus". Classic endoscopy appearance is that of a corrugated or ringed narrow caliber esophagus, commonly associated with multiple strictures.
Appropriate treatment is typically with steroid fluticasone (22 mcg/puff, without spacer). |
|
___________ is a primary esophageal motor disorder of unknown etiology characterized by insufficient lower esophageal sphincter relaxation and loss of esophageal peristalsis.
|
Achalasia!!
Radiographically there is aperistalsis, esophageal dilation, minimal LES opening with a birdbeak appearance and poor esophageal emptying of barium. Symptoms are: dysphagia for solid and liquid, regurgitation, heartburn Diagnosed via esophageal manometry. |
|
|
Which of the following is FALSE regarding achalasia?
A. Upon barium esophagram study, there is smooth tapering of the lowerr esophagus leading to the closed LES, resemblinga "bird's beak" B. There is esophageal aperistalsis upon esophageal manometry C. Golden test for diagnosis is endoscopy D. there is no cure but goal of treatment should be relief of patient symptoms and improved esophageal emptying. |
FALSE is: C. Golden test for diagnosis is endoscopy
The diagnosis is established by B. There is esophageal aperistalsis upon esophageal manometry. |
|
|
What are the appropriate treatments for each?
A. GERD B. Eosinophilic esophagitis C. Achalasia D. Zenker's diverticulum |
A. GERD: PPIs
B. Eosinophilic esophagitis: Steroid Fluticasone C. Achalasia: no cure, but goal is relief of patient symptoms and improved esophageal emptying. Two most effective treatments are: graded pneumatic dilation and surgical myotomy. D. Zenker's diverticulum: resection of diverticulum and myotomy of cricopharyngeus muscle |
|
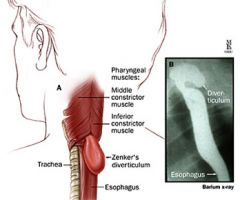
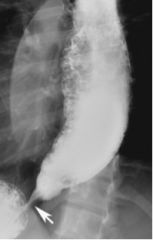
What is depicted and what is its treatment?
|
Zenker's diverticulum! Treatment is resection of diverticulum and myotomy of cricopharyngeus muscle.
|
|

1. A 79 year old male is admitted to the hospital with aspiration pneumonia. He gives a significant history of dysphagia and regurgitation of undigested food material. His wife of 55years complains of severe bad breath. Below is the endoscopic appearance, Pick the most likely anatomical location for this condition.
A. Between the oblique fibers of the inferior pharyngeal constrictor and transverse fibers of the cricopharyngeus muscle B. Between the cricopharygeus and the cervical esophagus. C. Between the oblique and the transverse fibers of the cricopharyngeus muscle D. Between the middle and inferior pharyngeal constrictors |
A. Between the oblique fibers of the inferior pharyngeal constrictor and transverse fibers of the cricopharyngeus muscle
|
|
|
Select the mechanism that best describes the
contribution of hiatal hernia to GERD. A. Loss of augmentation of the antireflux barrier by the crural diaphragm B. Impaired esophageal acid clearance. C. Transient lower esophageal sphincter relaxation (TLESR) may be elicited more easily. D. Trapping of gastric content that may reflux during TLESR E. All the above. |
E. ALL OF THE ABOVE!!
The size of the hiatal hernia is the strongest predictor of the severity of esophagitis. However the mechanistic causes are multi-factorial. |
|
|
Which of the following are considered to be the gold standard for the diagnosis of GERD?
A. Upper Endoscopy B. 24-hour pH monitoring C. Barium Esophagram D. Esophageal impedance testing E. None of the above |
E. None of the above
Despite being a common problem, there is no gold standard for this disease. 25-30% of patients with GERD have no increase in acid exposure. 50% of endoscopies are negative in symptomatic people. Barium radiograph is has a sensitivity of 25-75% and is false positive in 20%. Impedance, promising not yet established. |
|
|
A 22 year old medical student presents with significant history of atopy and asthma, presents with history of gradually worsening solid food dysphagia. He had been a slow eater most of his life. Over thanksgiving he had acute impaction of turkey in his esophagus that required Endoscopic disimpaction. What diagnosis best fits this description?
a) Nutcracker esophagus. b) Eosinophilic Esophagitis c) LA grade D esophagitis d) Congenital esophageal stenosis e) Schatzki’s ring |
b) Eosinophilic Esophagitis
|
|
|
If the dysphagia occurs more with solids rather than liquids, the problem is likely [ motility / obstructive ] related; If the dysphagia occurs equally with solids and liquids, then the problem is likely [ motility / obstructive ] related.
|
Solids > liquids = likely obstructive problem
Solids = liquids = likely motility problem |

