![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
|
Outline the basic mechanisms of defence against microbes.
|
• Physical: epithelial barriers (skin, mucosa)
• Chemical: tears (lysozyme), pH of stomach • mechanical: bronchial cilia, peristalsis • Physiological: cough reflex, vomiting & diarrhoea, voiding bladder • Competitive: commensal organisms - natural flora |
|
|
Compare cells and soluble factors of the innate and adaptive immune system.
|
Innate cells include: granulocytes, macrophages, dendritive cells and natural killer cells. Innate soluble factors include complements, cytokines, chemokines, acute phase reactants, antimicrobial peptides.
Adaptive cells include: lymphocytes ( T and B cells) and soluble factors include antibodies and cytokines/ chemokines. |
|
|
Define the meaning of the terms innate and adaptive immunity and the differences between the 2
|
Innate immunity is the first line of immune protection the body has against pathogens after the physical barriers have been breached. It involves cellular components and solluble factors, mainly neutrophils, macrophages and complements. The system does not have specificity and therefore does not have memory and is a very rapid response. The cells have toll like receptors that recognise PAMP (pathogen associated molecular patterns ) which may be mannose or LPS( gram negative outer membrane). The pathogen receptors on components of the innate system are germline encoded.
The adaptive immune system involves components which do have specificity, they retain memory of a pathogen once they have been in contact and so on the second exposure, the pathogen is destroyed much more quickly. The pathogen receptors on the T and B cells and antibodies are rearranged from multiple gene segments and they recognise antigen specific receptors. The system has a delayed primary response where the antibody IgM has a low affinity for the antigen but on the second exposure the lag phase is much shorter and the concentration of high affinity antibody, IgG, is much greater. |
|
|
Describe phagocytosis.
|
Phagocytosis is carried out by phagocytes eg neutrophils and macrophages. These cells travel in the blood and penetrate the endothelium to enter the cells ( rolling, adhesion, migration) following a chemotactic gradient created by chemokines - complements, leukotrienes, bacterial agents. A phagocyte recognises a microbe by specific sugar residues (PAMPs) eg manose or lipopolysaccharide but binding is helped by opsonisation with IgG and/or C3b. Phagocytes bind to the opsonins by their Fc and C3b receptors. The microbe is internalised by endocytosis and intracellular vesicle buds of called a phagosome. A lysosome fuses with the phagosome to form a phagolysosome ( secondary lysosome) and the microbe is destroyed by oxygen dependent and oxygen independent pathways.
|
|
|
List the oxygen dependent and independent pathways adopted in phagocytosis.
|
Oxygen dependent:
ROS - Hydrogen peroxide, hydroxyl radical, singlet oxygen, hypohalite, nitric oxide. The reactive oxygen species are formed in the NADPH-oxidase system. A deficiency of this system leads to an inability to cope with bacteria eg staphylococci and fungi like the mould aspergillus eg chronic granulomatous disease – a hereditary condition where there is a defect in the PHOX enzyme complex (NADPH-Oxidase leading to decreased respiratory burst). Oxygen independent: Lysozyme, acid hydrolases, lysosomal contents, lactoferrin, neutral proteases, cationic proteins. |
|
|
Define an antigen, an immunogen, a hapten, an epitope and an antibody.
|
An antigen is a molecular structure that can be recognised by the specialised receptors of T and B cells.
An immunogen is a molecular structure that is able to initiate an immune response after being recognised as antigenic. (usually the same as an antigen). A hapten is a smaller molecule that is not able to initiate an immune response but can interact with a complimentary antibody. An epitope is the exact molecular sequence or structure that is recognised by an individual antibody or T cell receptor ( ie an antigen may contain more than one epitope). |
|
|
Define hummoral and cell-mediated immunity.
|
Hummoral immunity relates to the antibody response to antigens whereas cell mediated immunity refers to adaptive immunity not involving antibodies but T lymphoctyes.
|
|
|
Describe the primary and secondary adaptive immune responses.
|
When the antigen is encountered for the first time there is initially a lag phase, before any antibody against the antigen is detected. During this phase the antigen is being recognised, processed and presented by APCs ( antigen presenting cells) to lymphocytes. This is the primary response and the immunoglobulin produced is IgM which stays in the blood for a little while before disappearing. Memory lymphocytes however remain in the blood so that on the second encounter of the antigen there is very little lag phase and the antibody concentration is much larger than in the primary response. IgG is the immunoglobulin of the second phase response which has a higher affinity for the antigen and it remains in the blood for much longer.
|
|
|
Describe active and passive immunisation
|
In active immunisation the adaptive immune system is triggered by injecting a weakened form of the live organism responsible for the disease, killed organisms or a denatured toxin. There is an initial lag phase as primary response occurs and then memory lymphocytes specific to that antigen are produced so that on exposure to the real pathogen, they will mount a rapid and great response.
In passive immunisation the adaptive immune system is NOT triggered. A serum containing antibodies against the disease is injected eg anti-tetanus serum and so the individual is immediately immunised without much of a lag phase. However, the immunity is only short lived as there is no immunological memory. |
|
|
What is C-reactive protein and what triggers its release?
|
C reactive protein is an acute phase protein that is released from hepatocytes stimulated by IL-6. C reactive protein reacts with the cell wall of group C streptococci.
|
|
|
What is the difference between a lymphocyte and a lymphoblast?
|
The lymphocyte is initially small but after responding to an antigen it becomes larger, the nuclear chromatin becomes less dense and the volume of cytoplasm increases to form a lymphoblast.
|
|
|
Describe the concept of bone marrow stem cells giving rise to all cells of the immune system.
|
The bone marrow is primary lymphoid tissue along with the thymus.
There are 3 types of stem cells within the bone marrow: haemopoietic, mesenchymal and endothelial. Haemopoietic stem cells differentiate into myeloid and lymphoid progenitor cells. The myeloid cells differentiate into reticulocytes -> erthyrocytes, megakaryocytes,basophils, eosinophils, mast cells, neutrophils, monocytes ( dendritic cells and macrophages) The lymphoid cells differentiate into natural killer cells and small b and t lymphocytes. The b cells will mature within the bone marrow where as the t cells ( thymocytes) travel to the thymus where they mature and are educated to recognise MHC. |
|
|
What is secondary and primary lymphoid tissue?
|
The lymphoid tissues are the sites where the cells of the immune system are organised into specific structures.
Primary lymphoid tissues include the bone marrow and thymus and is where the lymphocytes are formed and mature. Secondary lymphoid tissues are arranged as a series of filters monitoring the contents of the extracellular fluids, i.e. lymph, tissue fluid and blood. The lymphoid tissue filtering each of these fluids is arranged in different ways. Secondary lymphoid tissues are also where lymphocytes are activated. It includes lymph nodes, spleen, tonsils, peyers patches and mucosa-associated lymphoid tissue (MALT) |
|
|
Describe the anatomical location of the thymus.
|
The thymus is found in the thorax in the anterior superior mediastinum. It enlarges throughout childhood until puberty where atrophy of the gland occurs but it continues to function throughout life.
|
|
|
Describe the structure of the thymus gland.
|
The thymus gland comprises of lobules containing an outer more cellular cortex and in inner less cellular medulla. There is a fibrous capsule surrounding the gland, beneath which lies a subcapsular epithelial layer which extends into the cortex and the medulla. Within the medulla the specialised epithelial cells aggregate to form hassall’s corpuscles which are involved in the maintenance of self tolerance. There are many APCs – macrophages, dendritic cells and B cells. T Lymphoid cells migrate to the cortex via the circulation where they proliferate, mature and pass on to the medulla where the mature T cells are released into the circulation
|
|
|
Describe aplastic anaemia.
|
Aplastic anaemia is a condition where the bone marrow fails to produce enough blood cells to replenish the old and damaged ones. There are low counts of erthryocytes, leucocytes and platelets and this is called pancytopenia. It is usually idiopathic but can be autoimmune.
|
|
|
Describe the passage of cells through the thymus gland during the process of T cell maturation.
|
Immature T cells ( thymocytes) migrate from the bone marrow to the thymus where differentiation, TcR gene rearrangement and expression and positive and negative selection are carried out into mature T lymphocytes.
The thymocytes enter the subcapsular region and are initially double negative – CD3 – 4 – 8 – . TCR gene rearrangement occurs and any T cells with defects in their receptors are destroyed. The successful thymocytes then enter the cortex as double positive thymocytes( this is the only place in a healthy person where double positive should be seen) and undergo positive selection ( self restriction) where they are presented with MHCs. If they can’t recognise and bind to self MHCs they are destroyed as they are not functional. They then enter the corticomedullary junction where they undergo negative selection (self tolerance) where thymocytes,which have a high affinity for self antigens, are destroyed as they would initiate autoimmune attacks. The thymocytes then differentiate into single positive cells either CD8+ which recognise MHC 1 or CD4 + which recognise MHC 2. They enter the medulla as mature T cells and then enter the circulation where they travel to secondary lymphoid tissue. . Only 1-3% of thymocytes survive the education to be released into the circulation. Lymphoid cells, epithelial cells, macrophages and other supporting cells are all found within the thymus gland. |
|
|
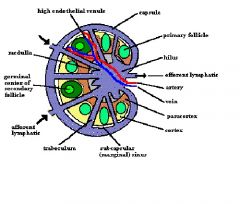
Describe lymph nodes.
|
Lymph nodes are secondary lymphoid tissue. Their role is to filter lymph, phagocytose pathogens and present antigens.
They are bean shaped structures which lie along the course of the lymphatics and aggregate at particular sites. Enlargement of nodes may indicate inflammation or malignancy except for those in the groin where enlargement is common. In the lymph nodes, phagocytic cells destroy foreign bodies and antigens are presented to the immune system. The lymph node is surrounded by a fibrous capsule which extends into the parenchyma producing supportive trabeculae. Within the node there are lymphatic sinuses, blood vessels and parenchyma (functional tissue – cortex, paracortex and medulla). |
|
|
Describe the cortex of the lymph nodes.
|
The cortex comprises of several compartments each containing a lymphatic nodule which contains B cells, APCs and macrophages. B cells enter the lymph node via High endothelial venules ( post- capillary venules) and pass into the follicles. If they are activated by the presence of a specific antigen then they proliferate in the lymphoid follicles. The activated b cells are then called follicle centre cells and the area is known as the germinal centre in the secondary follicle.The germinal centre is surrounded by a mantle zone containing small, naive b cells and some t cells. The follicle centre cells consist of centrocytes- cleaved nuclei and centroblasts – larger, more open nuclei and some nucleoli.
The cortex also contains many accessory cells eg sinus macrophages which are highly phagocytic, tangible body macrophages which are found in germinal centres, marginal zone macrophages found beneath the subcapsular sinus and follicular dendritic cells. |
|
|
Describe the paracortex of lymph nodes
|
The paracortex is the region between the cortex and the medulla which houses mostly T cells, APCs and macrophages. The T cells enter from the circulation via HEVs. When activated they form lymphoblasts ( larger chromatin and cytoplasm) which divide to produce a clone of cells specific to a certain antigen. The cells enter the circulation.
|
|
|
Describe the medulla of the lymph nodes.
|
The medulla consists of medullary sinusoids, medullary sinuses and medullary cords.
Cells that arrive at the medulla from the cortex and paracortex form medullary cords composed of T cells, B cells and MANY plasma cells. the t cells and b cells enter the medullary sinusoids and leave the node via the efferent vessels. |
|
|
What happens to the activated B cells in the germinal centre?
|
The b cells proliferate and undergo somatic hypermutation where their surface immunoglobulin become specific to the antigen displayed on follicular dendritic cells ( higher affinity antibody). They take up the antigen and present it to T cells in the follicles which react by releasing cytokines eg IL-4.
B cells -> centrocytes -> centroblasts -> leave follicle and pass to paracortex and medullary sinuses where they become immunoblasts -> plasma cells or memory cells. |
|
|
Describe the passage of lymph
|
Lymph passes into the node via the afferent lymphatics into the marginal sinuse, through the cortical sinuses to reach the medullary sinuses and then leave via the efferent lymphatics. In the lymph node the lymph is filtered and pathogens are phagocytosed by macrophages. Antigens are taken up by APCs eg dendritic cells to present to the lymphoctyes. Less than 10% of lymphocytes enter within the lymph, most enter within the blood via the HEVs.
|
|
|
Describe the anatomy of the lymphatic system.
|
The lymphatic system comprises organs eg thymus, bone marrow and spleen, ducts and nodes and transports the watery, clear fluid lymph around the body. Lymph is the fluid and protein that has been squeezed out of blood
The functions of the lymphatic system are to collect and return interstitial fluid, including plasma protein to the blood, and thus help maintain fluid balance, to defend the body against disease by producing lymphocytes, to absorb lipids from the intestine and transport them to the blood (chylomicrons) |
|
|
Describe the structure of the spleen
|
The spleen is located in the upper left quadrant of the abdomen, anterior to the left kidney and superior to the splenic colonic flexure. The spleen is the largest lymphoid organ of the body and functions to filter blood, phagocytose old red blood cells and microbes, supply immunocompetent T and B cells and manufacture antibodies.
A capsule surrounds the spleen and extends septa inwards which are connected to a complex reticulin framework. The red pulp of the spleen consists of pulp cords and sinusoids and it functions to filter. There is a complex system of blood vessels arranged to remove old or damaged erthryocytes from the circulation. The globin part of haemoglobin is broken down into amino acids whereas the haem part is broken down into bilirubin, which travels to the liver to become conjugated and removed. The white pulp of the spleen consists of lymphoid tissue associated with arteries and is the immunological part of the spleen. It contains t cells within the periarteriolar lymphoid sheath and b cells within lymphoid nodules. accessory cells ( sinus macrophages, tingible body macrophages, marginal zone macrophages, dendritic cells) are found throughout. The branches of the splenic artery leave the trabeculae and enter the white pulp, surround by a periarteriolar lymphoid sheath, which contains b cell follicles and t cells. Between the red pulp and white pulp lies the marginal zone where larger lymphoctyres and dendritc cells are located. |
|
|
Describe the splenic blood supply.
|
The splenic artery, a branch of the celiac trunk, enters the spleen via the hilum and passes into the interior via trabeculae as trabecular arteries. The trabecular arteries enter the white pulp and become surrounded by the periarteriolar lymphoid sheath which houses T cells, and occasional lymphoid nodules which house B cells. It is called the central artery. Central arteries enter the red pulp by losing the sheath and divide into penicillar arteries which posess 3 regions: pulp arterioles, sheathed arterioles and terminal arterial capillaries.
|
|
|
Predict the possible effects of splenectomy.
|
The removal of the spleen is often performed to prevent the patient from bleeding to death. Total spenectomy does not produce serious effects because other reticuloendothelial organs eg liver and bone marrow can take over the spleens functions. However there is greater susceptibility to bacterial infections which can result in sepsis. The common infections are NHS – Neisseria meningitis, Haemophilius influenza, streptococci pneumoniae.
The spleen cleans all blood borne pathogen, so clearance of opsonised blood borne bacteria will be reduced, patients will have decreased IgM due to fewer mature b cells and immune response against polysaccharide antigens will be reduced. |
|
|
Describe the common sites and the cellular constituents of mucosa associated lymphoid tissue.
|
MALT comprises of the other sites where lymphoid tissue is found eg GI tract, respiratory tract and urogenital tract.
In the gi tract it is called GALT –gut associated lymphoid tissue. This comprises of - Tonsils- lymphoid tissue in submucosa of orophranx, many lymphoid follicles with germinal centres - Adenoids – lymphoid tissue in nasopharynx - Peyer’s patches – lymphoid tissues in submucosa of the small intestine, mainly the illeum - Lymphoid tissue in colon and appendix Lymphoid tissue accumulate with age in the stomach. SALT - Langerhans cells - Skin homing T lymphocytes |
|
|
Describe the role of M cells in peyer’s patches.
|
Peyer’s patches are a type of GALT, found in the small intestine but mainly in the ileum. The m cells ( microfold cells ) are able to transport antigens from the lumen via transcytosis across the gut wall to dendritic cells and lymphocytes in the peyer’s patches. The b cells are stimulated by the antigen in peyer’s patches to secrete IgM. The stimulated B cells and memory cells pass to the mesenteric lymph nodes where the immune response is amplified. Activated lymphocytes pass into the blood stream via the thoracic duct and then hone into the gut and carry out their final effector functions.
|
|
|
Describe the mononuclear phagocyte system.
|
The mononuclear phagocyte system is a part of the immune system that consists of the phagocytic cells located in reticular connective tissue. The cells are primarily monocytes and macrophages, and they accumulate in lymph nodes and the spleen. The Kupffer cells of the liver, alveolar macrophages in the lungs, microglia in the central nervous system and tissue histiocytes are also part of the MPS.
Its functions include: - Formation of new red blood cells (RBCs) and white blood cells (WBCs). - Destruction of old RBCs and WBCs. - Formation of antibody. - Formation of plasma proteins. - Formation of bile pigments. "Reticuloendothelial system" is an older term for the mononuclear phagocyte system, but it is used less commonly now, as it is understood that most endothelial cells are not macrophages.[ |
|
|
Draw a lymph node
|
|
|
|
Describe the process and purpose of lymphocyte recirculation.
|
The patterns of recirculation depend on the state of activation of lymphocytes, the adhesion molecules expressed by endothelial cells and the presence of chemotactic molecules which selectively attract specific populations of lymphocytes and macrophages.
The main processes involve: - Naive lymphocytes travelling from primary to secondary lymphoid tissue via the blood - Activated lymphocytes travelling from spleen, lymph nodes and MALT into the blood and to other lymphoid and non-lymphoid tissues - APCS eg macrophages and dendritic cells carry antigen back to lymphoid tissues from periphery. The purpose of recirculation of lymphocytes and APCS is to expose the cells to more antigens. |
|
|
What is the principal antibody class of the secondary immune response and can cross the placenta?
|
IgG which is a very small antibody and so can cross easily through barriers.
|
|
|
Which antibody class is produced at mucosal surfaces.
|
IgA
|
|
|
Which antibody class is produced in the primary immune response?
|
IgM
|
|
|
What is pernicious anaemia?
|
Vitamin B12 absorption from the gut requires intrinsic factor and must take place at the terminal ileum. Malabsorption of vit B12 can be caused therefore by damage to parietal cells which secrete intrinsic factor along with acid and HCO3 or due to damage to the terminal ileum. Atrophic gastritis causes pernitious anaemia as it causes chronic inflammation of gastric mucosa, destroying gastric pits containing parietal cells. It may be casued by the presence autoantibodies agaisnt the parietal cells or due to helicobacter pylori infection.
|
|
|
Describe atrophic gastritis.
|
Atrophic gastritis is chronic inflammation of the gastric mucosa leading to the destruction of the gastric pits containing parietal cells, chief cells, g cells etc. It can be an autoimmune disease, which usually affects the body and fundus and is associated with pernicious anaemia or can be caused by helicobacter pylori infection which mainly affects the antrum
|
|
|
What is found following antigen challenge in the cortex of lymph nodes? What is found predominatly in lymph node medullary cords?
|
The primary follicle become secondary follicles with germinal centres indicating activated B cells.
Medullar cords house many plasma cells. |
|
|
What occurs in the thymus in health but rarely seen in secondary lymphoid organs?
|
During education of thymocytes which are - cd3, 4, 8, they are initially made into double posiitve T cells in marginal zone ( CD4+, CD8 +). They then undergo positive selection in the cortex, negative selection in the corticomedullary junction and then differentiate into either CD4+ OR CD8+ and enter the medulla where they can leave via the blood to secondary lymphoid tissue. In health T cells are only single positive.
|
|
|
Give examples of why the spleen would be removed?
|
The spleen, similar in structure to a large lymph node, acts as a blood filter. Current knowledge of its purpose includes the removal of old red blood cells and platelets, and the detection and fight against certain bacteria. It is also known to function as a site for the development of new red blood cells from their hematopoietic stem cell precursors, and particularly in situations in which the bone marrow, the normal site for this process, has been compromised by a disorder such as leukemia. The spleen is enlarged in a variety of conditions such as malaria, mononucleosis and most commonly in "cancers" of the lymphatics, such as lymphomas or leukemia.
It is removed under the following circumstances: When it becomes very large such that it becomes destructive to platelets/red blood cells For diagnosing certain lymphomas Certain cases of wandering spleen When platelets are destroyed in the spleen as a result of an auto-immune process (see also idiopathic thrombocytopenic purpura) When the spleen bleeds following physical trauma Following spontaneous rupture For long-term treatment of congenital erythropoietic porphyria (CEP - gunther disease) if severe hemolytic anemia develops[1] The spread of gastric cancer to splenic tissue When using the splenic artery for kidney revascularisation in renovascular hypertension. For long-term treatment of congenital pyruvate kinase (PK) deficiency As a treatment for idiopathic thrombocytopenic purpura (ITP) when steroids and other medication have proven ineffective.[citation needed] The classical cause of traumatic damage to the spleen is a blow to the abdomen during a sporting event. In cases where the spleen is enlarged due to illness (mononucleosis), trivial activities, such as leaning over a counter or straining while defecating, can cause a rupture. |

