![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
Head shaking
Treatment |
Photic and trigeminal neuralgia
Cyproheptadine and carbamazepine. Avoid stimuli. Sclerosis of posterior nasal nerve. Permanent tracheostomy? |
|
|
Lower respiratory diseases in neonates (x5)
Ddx |
Neonatal pneumonia - Sequel to bacteraemia/septicaemia. Dull, fever, tachypnoea. Broncoscopy, aspirate, US, RG. Antibiotics - C+S. Penicillin/gentamicin. IgG. Oxygen, iv ft, turn. Prognosis - depends on severity.
Prepartum EHV-1 infection - Weak foals. PCR or inclusion bodies in liver, lungs, thymus. Fractured ribs - stabilise with adhesive bandage, confine for a few weeks. Surgical for flail chest. Meconium aspiration - In utero stress. Nursing, broad spectrum antibiotics. Premature/dysmature - severe expiratory effort. Surfactant, respiratory support, antibiotics. |
|
|
Lower respiratory disease in growing foals (x2)
Ddx |
Rhodococcus equine pneumonia - intensive rearing, warm dry climate. Inhalation or ingestion bacteria. Don't develop signs until 2-6 months old. Multifocal pulmonary abscessation. Ill thrift, progressing dyspnoea. RG, US, tracheal aspirate. Rifampin and erythromycin prolonged tx. Prophylaxis - reduce stocking density, poo-pick, antibiotics, hyperimmune serum.
Streptococcus equi var zooepidemicus - groups of growing foals. Nuisance. Cough, nasal discharge, slight submandibular enlargement, mild pyrexia. Penicillin or nothing. |
|
|
Acute infectious respiratory disease in adults (x6 main ones)
DDx General. |
Influenza - ELISA, very high infectivity, spreads quickly. Vaccine.
EHV-1 - Mostly abortion and encephalopathy rather than resp disease. Most horses infected when young, latent. EHV-4 - Commonest resp infection. Young horses in training. Prolonged immunosuppression. Rhinovirus - with other agents. URT. EVA - Resp disease signs and severe conjunctivitis (pink eye), depression, periorbital oedema. Venereal spread. Vaccine. Strangles - Streptococcus equi var equi. Direct contact or fomites. Pyrexia, bilteral purulent nasal discharge, dysphagia, marked swelling of SMLNs. Atypical - no abscessation. Nasopharyngeal swabs or GP washes, tracheal aspirates - PCR or ELISA. Penicillin early (no absc) Mycoplasma felis and equirhinis, Bordatella bronchiseptica, Strep pneumonia, Pasteurella, Actinobacillus - Tracheal aspirates. Feed from ground to allow drainage. Abs if febrile >4-5 days, purulent secretions or persistent marked signs. Clenbuterol for mucociliary clearance. |
|
|
Strangles sequelae
When are horses classed as clear from strangles? |
Bastard strangles - abscessaton in other tissues including mediastinal and mesenteric LNs. Fever, malaise, WL. Poor prognosis
Purpura haemorrhagica - Type 3 mediated vasculitis 1-3 months after infection. Generalised oedema, petechiation, pyrexia, multi-organ failure. High mortality. Immunosuppressive dose of dexamethasone, penicillin and supportive care. Guttural pouch empyema When 3 NP swabs collected at weekly intervals are -ve. |
|
|
Pulmonary and chest wall disorders in individual horses
RAO SPAOPD IAD Lungworm |
Airway inflammatory response to pro-inflammatory agents from poorly conserved hay and straw. Coughing, bilateral mucopurulent nd, ex intol, heave line, crackles and wheezes, dyspnoea in severe. >5yo. Endoscopy, BALF >5% neutrophils. Keep permanently at pasture or best ascan do. Atropine rescue drug, Clenbuterol/salbutamol. Inhaled beclomethasone or oral preds. Maintain hydration.
Pastured horses spring-autumn. Dyspnoea. Crackles and wheezes. Neutrophilic secretions. Move to different area if possibe. Bronchodilators and GCs. Coughing, ex intollerance, neutrophilic mucopus, nasal discharge. Not depressed. All ages. May self-resolve or persist. Bacteria and inhaled allergen. Antibiotics (C+S) - oxytet, TMPS. Rest, dust-free. Chronic - GCs. Dictyocaulus arnfieldi - Summer-autumn. Pastured with donkeys. Eosinophilia in BALF. Response to anthelmintic. Avermectin or benzimidazole. Clean pasture. |
|
|
Pulmonary oedema
Pleural effusion EIPH |
URT obstruction, cardiac failure, alveolitis, smoke, neoplasia, toxicity, IM, volume overload. Frothy nasal discharge, increased effort, crackles. Endoscopy - frothy fluid. RG - diffuse interstitial pattern or mixed interstitial/alveolar pattern.
Neoplasia, bacterial pleuropneumonia (transit), pnetrating wound, peritonitis, CHF, hypoproteinaemia, chylothorax, diaphragmatic hernia. Auscultation, precussion, US. Pleural fluid analysis. Cytology of fluid. Treat cause and perform thoracocentesis. Exercise induced pulmonary haemorrhage. Bleed from dorsocaudal lung during fast exercise. Most asymptomatic but severe - epistaxis, poor performance, pulling, up, death. Bronchoscopy. Haemosiderophages in BALF. x - rest, treatment of underlying cardiac or respiratory disorders, NSAIDs to reduce fibrosis, dust free, training at lower speed. Retired. |
|
|
Causes of poor performance
Increased jugular filling causes (>1/3). Reduced. Where do horses develop oedema What murmurs are developed in response to training? Treatment of pericardial effusion |
Musculoskeltal, respiratory tract, lack of fitness, owner's unrealistic expectations, inappropriate training, cardiovascular, medical/neurological.
Cranial thoracic obstruction, pericardial effusion, right sided failure. Reduced - hypovolaemia, low output failure. Plaque along ventral thorax and can extend to cranial abdomen. Upper forelimbs in severe. Lower limbs - non-cardiac. Tricuspid and mitral regurgitation. Drain, lavage with saline, steroids in non-septic, septic - penicillin/gentamicin and steroids into pericardial sac, systemic antibiotics too. |
|
|
Tachyarrhythmias
Atrial fibrillation Premature systoles |
Common cause of poor performance in hunters and TBs. Caused by atrial dilation secondary to valvular dysfunction, secondary to electrolyte abnormality or medical conditions such as peritonitis, alpha 2 agonists (increase vagal tone), recovery from GA. PP at max speed. Irregularly irregular rhythm. No P waves. Tx - underlying cause. If evidence of cardiac failure - Quinidine sulphte per os. (Tx can lead to SVT - digoxin, sodium bicarbonate). Non-responders - second treatment after 24 hours, then every 6h, digoxin every 12 h until sinus rhythm restored. Once converted - rest for 5-7 days, over 3-4 weeks return to training. Electric defibrillation or cardioversion an option.
Atrial or ventricular. Hypoxia, myocardial disease, electrolyte and metabolic disturbances, elevated sympathetic tone, fever and toxaemia. Atrial may predispose to atrial fib. Ventricular may predispose to ventricular fib. Atrial - early P waves. Ventricular - premature QRS. Life threatening vent tachyc - lidocain |
|
|
Bradydysrhythmias
|
AV blocks
Sinus block and AV block normal First degree - Long P-Q Second degree AV block - Some P waves not leading to QRS. If profound and causing bradycardia, daily oral administration of alpha 2 adrenoreceptor agonists - clenbuterol. Third degree - Total block in conduction at AV node. P waves not associated with QRS. Inflammation/degeneration of AV node. Multiple P waves not associated with QRS. Escape rhythm. Pace maker. Some resolve spontaneously or anti-inflammatory drugs. |
|
|
Mitral regurgitation
Tricuspid regurgitation Aortic insufficiency Ventricular septal defect |
Develops in response to training, thickineing/fibrosis of leaflets - atrium dilates (predisposes to atrial fib, leads to biventricular failure), rupture of chordae tendinae, secondary to DCM/aortic insufficiency/ VSD, congenital dysplasia, endocarditis. Excluded from loss of use, won't cause sudden death.
National hunt horses. Develops as result of pulmonary hypertension caused by left ventricular failure, ruptured chordae, congenital dysplasia. Not likely to be caused by thickening so unlikely to progress but this must be proven. Excluded from loss of use, won't cause sudden death. Progressive, thickening and fibrosis of aortic valve leaflets. 10 years+. Decreased perfusion to myocardium - sudden death. Cardiac failure may also occur. Most common congenital abnormality. Shetlands, Welsh, Arab. If small - no effect. If large - left ventricular overload and cardiac failure. Membranous septum below aortic and tricuspid valves mostly, sometimes muscular septum. Not sudden deat |
|
|
Diarrhoea
Mechanisms Acute Chronic (>1 month) Treatment of acute |
Malabsorption, increased secretion, abnormal motility, osmotic overload, increased hydraulic pressure from blood to intestinal lumen.
Infectious - Salmonella typhimurium, Clostridium difficile, Clostridium perfringens); Cyathostomiasis; Toxic - NSAIDs; antibiotic associated; carbohydrate overload. Chronic inflammatory conditions - Chronic salmonellosis, chronic cyathostomiasis, Lawsonia intracellularis, sand, NSAID; IBD - granulomatous, lymphocytic plasmacytic, multisystemic eosinophilic epitheliotropic disease; dietary; non-GI (liver, CHF, renal disease) Fluids, NSAIDs? -flunixin, Metronidazole, Bismuth subsalicylate, sucralfate?, butorphanol, broad spectrum antibiotics in neutropaenic (antibiotic use CI in salmonella, metronidazole clostridia), heparin if hypercoagulable, probiotics, pellet diet, limit long stem roughage. |
|
|
Treatment of cyathostomiasis
CHO overload Treatment of chronic diarrhoea if undifferentiated |
Larvicidal anthelmintics (Fenbendazole) then ivermectin on day 6. Dexamethasone.
Exclude grains from diet, mineral oil/magnesium sulphate to clear CHO, charcoal to decrease absorption of endotoxin, bicarbonate solutions iv Change diet to hay and alfalfa, stop NSAID and antibiotic therapy, caecal transfaunation or probiotics, larvicidal dose anthelmintics (and CS if suspect cyathostomiasis), CS last resort - may improve inflammatory enteritis. |
|
|
Colic history
|
Age,breed, sex, insurance, when first noticed, how rapidly progressed, feed/water intake, faeces and urine output, repeated?, weight loss, worming, in or out, recent diet change, stage of work, bedding, season
|
|
|
Colic Clinical exam
Degree/nature of pain Abdominal distension Rectal temperature Heart and pulse rate/quality Respiration MM Abdominal auscultation Digital pulses Muscle tremors. Faeces |
Intermittent/continuous/increasing/decreasing Visceral (unrelenting) - spasm, distension, ischaemia, stretching. Parietal - agony - peritonitis (boarding of abdomen).
Large colon/caecal distension. Raised - enteritis, colitis, peritonitis, abscessation. Low - Shock (rapid weak pulse too) Tachy - dehydration, endotoxaemia. Pulse strength rough guide to peripheral perfusion. Increased rate - pain, acidosis, distension Pink - mild, pale - haemorrhage, red - endotoxaemia, cyanotic - euth. CRT prolonged - endotoxaemia. Haustral (short) and peristaltic (long). Increased sounds with spasmodic/tympanic. Decreased with others. Increase with laminitis - caused by EnT Common. GS - triceps and flanks (fine). Not much with severe. Check it. |
|
Colic rectal findings
Pelvic flexure impaction Small intestinal distension Caecal intussusceptions Large intestinal gaseous distension Nephrosplenic entrapment of large colon (left dorsal displacement) |
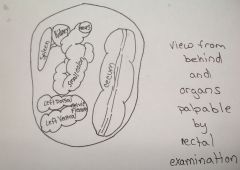
Doughy mass indented with pressure. Wall smooth. Severe - felt in pelvis.
Secondary - with colonic stasis e.g. grass sickness - absorption of fluid from colon, firm ingesta, corrugated. Bicycle tyres, no taenial bands. Grass sickness, enteritis, strangulation, ileal impactions, intuss, non-strangulating infarctions. Caecocaecal - mass within caecum. Ileocaecal - painful oedematous mass within caecal base. Flatulent colic, transverse or small colon obstruction, large colon displacements, torsions. Feel large colon between body wall and spleen. |
|
|
What must you always do with a colic?
What conditions cause gastric dilation/reflux Interpreting abdominal paracentesis |
Pass a nasogastric tube.
Acute grass sickness, ileus, small intestine strangulation, proximal jejunitis, large intestinal obstruction. Increased fibrinogen and protein initially. Progressive insult - neutrophilia, increased erythrocytes. Normal - straw coloured, some turbidity, doesn't coagulate Turbid - Can't read newspaper through (high protein or cell count) Purulent - peritonitis Serosanguinous - infarction Fresh blood - haemoperitoneum or iatrogenic (streaking, clots) Digesta - iatrogenic or rupture (shock and endotoxaemia present). |
|
|
Indications for surgery/euthanasia
|
Severe continuous pain showing no or short duration improvement with analgesia
Pulse >60, progressively rising and weakening Progressive cardiovascular collapse, PCV>55, injected/cyanotic mm despite fluids Rectal findings positive for acute abdominal disease Progressive reduction in intestinal motility or continued gastric reflux. Increasing abdominal distension Serosanguinous peritoneal fluid with high protein and WBCs Treat medically if none of these are present. |
|
|
What to do when referring colics
|
EARLY
Decompress stomach Analgesia - minimum to keep comfy otherwise mask it. Stabilise prior to referral Rug and leg bandages Send referral letter with good history and treatments given. Directions to referral centre. |
|
|
Medical treatment of colic
Analgesics Sedatives Spasmolytics Laxatives, with FT (soften impactions) - polyionic fluids most practical and cost effective for iv therapy for horses. |
NSAIDs
Phenylbutazone suitable as first choice in many types of colics. May last for 12 hours or more with low grade pain. Less likely than flunixin to mask endotoxaemia. Flunixin meglumine - May last >12h. Reduces effects of endotoxins. Ketoprofen similar. Opioids Butorphanol - 3-4 h. Good analgesic, minimal sedation. May decrease gut motility. Used with alpha 2s to provide better analgesia. Morphine - Gold standard visceral analgesia. Premed with alpha 2. Duration of action depends. Alpha 2 agonists Romifidine - moderate/mild visceral analgesia 30-40 mins. Least amount of ataxia Xylazine - 20 -30 mins. Potent analgesic. Some ataxia Detomidine - Potent visceral analgesic and sedative. 60+ mins. Greatest ataxia. Buscopan compositum - metamizole (NSAID) and butylscopolamine (spasmolytic). Buscopan - no NSAID. Liquid paraffin (watch asp), dioctyl sodium sulfosuccinate, oral magnesium sulphate (toxic @ high doses) |
|
|
General management of simple colics
|
Analgesics
Warm, deep inedible bedding, muzzle, remove injurious items. Remove feed for several hours (up to 12), make sure horse passes several piles of normal faeces before eating. Free access to water. Hand walk every 2-3 hours for 10-15 minutes. Reassess regularly. |
|
|
Specific medical colics
|
Gastric ulcers, gastric dilation - may lead to rupture, gastric impaction, anterior enteritis, spasmodic colic, tympanic colic, abdominal neoplasia
Obstructive Intraluminal - large colon impaction, small colon impaction, ileal impaction, caecal impaction, sand impaction Extraluminal, functional |
|
|
What causes the most pronounced jaundice?
Jaundice most likely with acute or chronic liver disease? What can cause an increase in unconjugated bilirubin? Liver derived enzymes Increase in serum levels of bile acids indicates loss of what % of liver function? High unconjugated bilirubin and normal PCV and liver enzymes High unconjugated bilirubin and low PCV High unconjugated and conjugated bilirubin and high liver enzymes and bile acids |
Conjugated bilirubin therefore most pronounced jaundice seen with hepatic or biliary obstruction.
Acute Fasting/anorexia GLDH - hepatocytes, GGT - biliary tract, AP - not liver specific. 70% Anorexia Haemolysis Liver disease |
|
|
DDx of equine liver disease
CS Lab diagnosis of liver disease Other diagnostics |
Ragwort toxicity, undifferentiated hepatic failure, haemachromatosis, echinococcosis, liver abscesses, aflatoxicosis, hepatic neoplasia, cholangiohepatitis, leptospirosis, liver fluke, obstructive cholelithiasis, portocaval shunts, Tyzzer's disease, hyperlipaemia, Cushing's
Gradual WL, decreased appetite, photosensitization. Failure - die within a few weeks. General signs of ill health. Icterus, photosensitisation (cutaneous accumulation phylloerythrin - pruritus, hepatic encephalopathy, coagulopathy, petechiae, bilateral laryngeal paralysis (inspiratory dyspnoea and stridor at rest) Liver enzymes, bilirubin, bile acids, ammonia (acute severe or end stage chronic), hypoglycaemia, coagulation indices reduced, bilirubinuria, peritoneal fluid US, biopsy |
|
|
Treatment of liver disease
Treatment of hepatic encephalopathy |
Supportive until regeneration occurs. Acute failure has best prognosis. Chronic with fibrosis - hopeless.
Remove source of hepatotoxins. High carbohydrate, low protein diet - can graze if photosensitisation not an issue. Beet pulp, maise and mollasses, fibre - fresh grass. Antibiotics - only when suppurative cholangitis or abscessation. Tracheostomy if bilateral laryngeal paralysis CS - chronic nonsuppurative cholangiohepatitis. HE - Sedation (low dose alpha 2s) if dangerous. Correct metabolic, fluid and electrolyte abnormalities, reduction in GIT absorption/production of neurotoxins (laxatives and neomycin/metronidazole), lactulose |
|
|
Grass sickness
|
Dysautonomia of unknown aetiology. Neuronal degeneration in autonomic ganglia and enteric neurones. (Myenteric). Very selective.
GI motility disturbance, dysphagia. Acute, sub-acute, (both fatal), chronic (45% survive) Acute - depression and muscle tremors, mil/moderate colic, inability to swallow, salivation, megaoesophagus, oesophageal ulcers. Fluid secreted into small bowel leads to small bowel distension, fluid not absorbed from large bowel (dessication), gastric distension, ileal impaction, large bowel impaction, black coating on large bowel contents, dry firm faeces, inspissated mucus coating, abdominal distension. Generalised/focal sweating, piloerection. Ptosis. Phenylephrine eye drops test. Tachycardia, dehydration, pyrexia, peritoneal fluid grossly normal. Subacute/chronic EGS - Weight shifting, narrow based stance, tucked up, rhinitis sicca, penile paralysis, aspiration pneumonia. Diagnosis of acute GS more problematic than for sub-acute and chronic GS. |
|
|
How can we improve diagnostic accuracy of acute/chronic GS
Treatment Risk factors Protective factors |
Visualise intestinal tract - rule out surgical lesions, not 100% accurate. Histology of ileal biopsy - not 100% accurate. PM - autonomic ganglia - gold standard.
SA and acute - euth Chronic - intensive nursing of selected. Selection criteria no continuous moderate/severe pain, some ability to swallow, no complete, persistent anorexia, some audible intestinal motility. Nursing care, analgesics, fluids, laxatives, cisapride. Horse-related (2-7 yo, good BCS or fat, low antibody level to clostridium botulinum), season/climate related (spring and early summer, recent cool/dry spells), premises related (previous occurence, stud farms, livery/riding, soil type), management related (grazing, recent movement, recent change of feed type/quantity, pasture disturbance, large horse numbers, frequent anthelmintic administration). Horse (older, contact with previous case (immunity?), chalk, co-grazing with ruminants, supplementary forage feeding, grass cuttings, hand remove droppings |
|
|
Brain and cranial nerve syndromes
Behavioural changes Seizures Obtundation, coma and sleep disorders Abnormal head posture Visual disturbances Facial and nasal hypalgesia/analgesia |
Forebrain
Physical expression of abnormal electrical discharges in forebrain neurones that reach motor areas and initiate spontaneous, involuntary movements. Foals more likely than adults. ARAS, hypothalamus, medulla oblongata, thalamus and cerebral cortex. Asymmetric forebrain lesions lead to holding head to side. Head tilt - vestibular syndromes - trauma or temporohyoid osteopathy. Forebrain - blind, depressed menace. Optic nerve lesions alter PLR. Thalamus, sensory lobe. |
|
|
Conditions causing brain and cranial nerve syndromes
Septicaemia-meningitis in foals West Nile virus Hepatic encephalopathy Neonatal hypoxia/ischaemia - maladjustment syndrome Neoplastic Idiopathic seizures foals Narcolepsy/cataplexy [Head trauma, intra-carotid injection] |
Failure of passive transfer, G-ve organisms, diffuse signs, CSF cloudy with low glucose, grave.
Exotic. Bird-mosquito cycle. Dead birds precede outbreak. 60% survival with nursing. Diffuse brain disease. Severe liver failure due to pyrolizidine, signs can be sudden in onset, mycotoxicosis, portal shunts, treat underlying disease. Bad to hopeless if severe signs. TB foals, rapid birth, delayed signs hours - 2days. Dummy, barker or convulsive foal. Passive transfer and nursing. Cholesterol granuloma Adolescent epilepsy associate with other illness e.g. pneumonia. Arabs. Self limiting. Phenobarb. Suffolk, shetland and shire foals. Can respond to imipramine HCl. Physiological in foals when restrained firmly. Rule out sleep deprivation. |
|
|
Vertebral column and spinal cord disease (see spinal segments in dog and cat neuro)
Wobblers Cervical vertebral malformation Spinal cord trauma EHV1 Equine protozoal myeloencephalitis (EPM) West nile virus Equine degenerative myeloencephalopathy Occipito-atlanto-axial malformation Cerebellar hypoplasia [Vertebral osteomyelitis, discospondylosis, verminous myelitis, neoplasia, cauda equina syndrome (fracture of S2)] |
Ataxia and paresis.
Fast growing males TBs and WBs. Ataxia and paresis due to cord compression. Stenosis of vertebral canal. Type 1 - osteochondral disease, type 2 - severe OA. Intervertebral corrected MSD measurements. Can surgically fuse vertebrae. If can't rise after several hours (especally 24, euth. Rest, CS, DMSO, mannitol to reduce oedema. Myeloencephalopathy. Groups of adults (previously abortions). Ataxia and paraparesis, worse over 24 hours then resolve. Recumbency - poor. Hind limbs, bladder. GCs. All sorts of neuro including ataxia. Sarcocystits. Antifolate, antimicrobial (sulphonamides) and toltrazuril. Mosquitoes and birds. Mild illness, spinal cord disease, muscle fasciculations. Mortality 40%. Vaccine twice a year. 3 m - 2 years. Diffuse spinal cord involvement. Tetraparesis and ataxia. Low vitamin E - low green forage. Supplement. Arabs. Birth - 1 y. Crepitus to tetraplegia. Arabs. Ataxia without weakness. First few months. Intention tremor. |
|
|
Ryegrass staggers
Temporohyoid osteoarthropathy. |
Symbiotic fungus (Neotyphodium lolii) - mycotoxicosis. Spino-cerebello-vestibular ataxia and tremor. Can look like spinal cord compression but do recover so don't destroy!
Proliferative osteopathy of temporal bone, temporohyoid joint and hyoid bone. Adults. Trauma or otitis? Fractures of petrous temporal bone or stylohyoid due to tongue movement in eating. May impinge on facial nerve and vestibulocochlear (vestibular signs) nerves. Partial unilateral styloidectomy may reduce progression and reduce risk of fracture. |
|
|
Which parasites are most often related to weight loss?
Diagnostic steps Symptomatic treatment of weight loss |
Cyathostomes.
PE, rectal , paracentesis, faecal analysis, haematology (neutrophilia with neoplasia or other inflammatory) biochemistry. Assess weight and re-evaluate. Diet change - ad lib good quality grass, hay, haylage, high energy feed - beet. Stop or start long term medication. Anthelmintics - where suspect cyathostomes - fenbendazole 5d then ivermectin on 6th day. |
|
|
Equine metabolic syndrome
What can lead to insulin resistance? Measures of insulin sensitivity and glycaemic status How to treat/manage MS |
AKA endocrinopathic laminitis. Obese horses/ponies predisposed to laminitis. Insulin resistance syndrome predisposes to laminitis.
Obesity, ECD, genetics (native ponies), exogenous steroids, stress. Fasting insulin and glucose. Oral glucose tolerance test. Control calorie intake (low glycaemic index, strip graze, soak hay 12 hours, sugar beet, antioxidant vitamins E and C) exercise, identifiable cause (ECD - treat with pergolide). Thyroid supplements? |
|
|
PUPD - definitions and common causes
CS of ECD, Dx, Tx |
PU >50ml/kg/day, PD 100ml/kg/day
Primary/psychogenic polydipsia, ECD/PPID, primary renal disease. (Less common - psychogenic salt consumption, diabetes insipidus, drug induced/iatrogenic) Hirsuitism, sweating, laminitis, lethargy, fat redistribution, predisposed to infections, weight loss, PUPD, polyphagia (Secondary DM), blindness, seizures. Dx - Basal glucose in starved non-stressed. Basal ACTH. Tx - clip hair!, farriery, Pergolide (dopamine agonist) |
|
|
Urinary incontinence causes
Tx Uraemia Azotaemia |
Reflex/upper motor neurone, paralytic LMN, non neurogenic (cystitis, urolithiasis, myogenis, neoplasia, ectopic ureter, breeding trauma, hypo-oestrogenism).
Palliative care - drainage and flushing, washing and vaseline, antibiotics, oestrogen to mares, alpha adrenergic blockers decrease sphincter tone, parasympathomimetics promote detrusor function. Signs associated with increased nitrogenous compounds - Anorexia, WL, bedraggled hair coat. Abnormal increase in biochemical parameters. Pre-renal - decreased perfusion in dehydration, renal - failure, post-renal - obstructive, uroperitoneum. |
|
|
Causes of acute renal failure
Causes of chronic renal failure Dx Tx |
Acute tubular necrosis - aminoglycosides, NSAIDs, polymixin B, Hb, Mb, vitamins D and K, heavy metals, acorns. Vasomotor nephropthy, acute glomerulonephropathy (immune-mediated, bacteria - Strep, E.coli), interstitial nephritis, leptospirosis - L. interrogans pomona
Glomerular disease, chronic interstitial nephritis, end stage renal disease, amyloidosis, neoplasia. CS, Isosthenuria, increased urinary enzymes, haematuria, casts, PUPD. Acute - Fluids, monitor urination, dialysis?, creatinine should decrease by 30% in first 24 hours, wean off fluids. Chronic - Fluid therapy, treat primary cause, diet - small frequent meals, avoid high calcium, increase CHO, anabolicsteroids may increase appetite. Blood transfusions. Erythropoeitin supplementation? |
|
|
Haematuria DDx
Timing |
Urethral tears, cystitis, urolithiasis, idiopathic renal haematuria (Arabs), neoplasia, NSAIDs, vaginal varicosities, exercise induces haematuria, non-urinary (haemolysis, acute myopathies, coagulopathy)
Throughout urination - kidneys, ureters, bladder Beginning of urination - distal urethra. End of urination - proximal urethra and bladder neck. |
|
|
Skin
Photosensitisation Cellulitis Chorioptic mange Coronitis Eosinophilic collagen necrosis Lymphangitis |
Primary - plant or chemical poisoning (St John's wort) - photodynamic agent delivered to skin.
Secondary - Digestion of chlorophyll produces phylloerythrin normally detoxified and excreted by liver but not in liver failure. Wound infection that rapidly spreads along tissue planes. Number of bacteria. Limbs. Painful. Antibiotics, NSAIDs, hydrotherapy, cleaning, gentle exercise. Chorioptes equi - feathers. Fomites. Pruritic. Remove hair and scabs. Insecticdes - permethrin and fipronil. Systemic ivermectin. Seleen shampoo. Immune- mediated - hyperkeratotic changes to hooves and chestnuts. Cracks, fissure, bleed, ooze. Symptomatic tx and CS. Firm, painless nodules, back and sides. Biopsy. Steroids. Inflammation of cutaneous lymphatics maybe secondary to bacterial infection. Hindlimbs. MArked swelling, lame, serum exudation, antibiotics, NSAIDs, potassium iodide and diuretics. Exercise. Ulcerative - Corynebacterium paratuberculosis, staph, strep. |
|
|
Melanomas
Mud fever Pediculosis Rain scald |
Greys. Benign. Perineum, sheath, parotid, GP, eyelids, lips, iris. Melanosarcomas rare - do metastasise and are invasive. Tx - Excision, cryosurgery, intralesional cisplatin, cimetidine orally.
Dermatophilus congolensis. Exudation, scabs, matted hair of distal white limbs. Staph and strep too. Antibiotics, AI, soak with chlorhexidine, clip, dry, fuciderm/flamazine. Pastern/cannon leucocytic vasculitis can look similar, treatment similar but with CS too. Damalinia equi (biting) and Haematopinus asini (suck), pruritus, scaling and alopecia. Winter. Common in ECD. Pyrethrins/pyrethroins. 2 apllications at 14 day intervals. Dermatophilus congolensis. Exudations, matted hairs, back. Paint-brush lesions. Antibiotics and clipping, soaking with CH. |
|
|
Ringworm
SCC Staphylococcal dermatitis Sweetitch Trombiculosis Urticaria Vasculitis |
Trichophyton equinum var equinum and var autotrophicum. Spores highly resistant. Abrasions. Circular areas of erect hairs followed by alopecia and scaling. Microscopy of hair pluck/scrape. Resolve spontaneously but tx limits spread. Enilconazole.
Microsporum gypseum, M. equinum, M. canis - less common. Can be spread by flies. Fluoresce. Enilconazole. Miconazole (malaseb) - not licensed. Invasive. UV and smegma. Excision, intralesional cisplatin, RT. Painful - folliculitis, furunculosis. S. aureus, S. intermedius and S. hyicus. Tx - ABs, CH. Hypersensitivity to Culicoides midge bites. Worse with age. Mane and tail, ventral abdo. Pruritus worst at dawn and dusk. Manage lesions, CS, immunotherapy, fly repellents (permethrin), prevent biting. T. autumnalis. Pruritus of head, legs. Late summer - autumn. Topical insecticides Pit on press. Allergens. Dex or preds. Inflam of blood vessel walls - I-M. Infections/drugs. Oedema, necrosis, ulceration lower limbs. CS, ABs |
|
|
Vulval conformation
What can clitoris harbour? Failure to show oestrus Small ovaries Enlarged ovary Normal sized ovaries Persistent oestrus |
Good - Vulval lips vertical, closely apposed, >80% below ischium
Fair - inclined < 80 degrees, apposed Poor - Inclined <80 degrees, poor seal. >50% above bony brim, sunken anus. Needs Caslick's vulvoplasty. CEM - Taylorella equigenitalis, Klebsiella pneumoniae and Pseudomonas aeruginosa. Winter anoestrus. Hypoplasia. Atrophied ovaries (emaciation, parasitism, age, stress, debilitating disease) GTCT - Inhibin A, testosterone. Unilateral ovariectomy. Stallion-like behaviour. Prolonged dioestrus - failure of luteal regression. Treat with PGF2alpha. Pregnancy. Seasonal anoestrus, spring transition, GTCT. |
|
|
Failure to become pregnant
4 types of endometritis (inflammation of endometrium) Causal agents of endometritis Clinical signs of endometritis Diagnosis Tx Predispositions to endometritis |
Endometritis, priglandular fibrosis, endometrial cysts, endometrial transluminal adhesions, CEM.
Chronic uterine infection (bacteria in uterus) - may have poor conformation, Venereal disease - CEM, persistent mating induced endometritis, endometriosis - degeneration of endometrium. Beta haemolytic streptococci (S. zooepidemicus), E. coli, P. aeruginosa, Klebsiella pneumoniae, yeasts, fungi. Discharge from vulva/uterus, fluid in uterus on US, may have no visual CS, infertility. Culture of uterine swabs, histological or cytological, CS, discharge, uterine fluid Short cycle with PGF2alpha, oxytocin and lavage with sterile saline, antibiotics into uterus (Ceftiofur for strep, Gentamycin for Kleb, Pseudomonas - timentin. Clitorectomy? Caslick's. Good hygiene. 3 sets of swabs 2 day intervals at 7 days. Pneumovagina, urovagina - conformation, weight loss. |
|
|
Contagious equine metritis
|
Taylorella equigenitalis. NOTIFIABLE. G-ve. Clitoral sinus. Causes severe endometritis, necrosis and shedding of uterus lining. Profuse watery mucopurulent, non-clumping discharge. Short cycle. Stallions carriers. Isolate from repro tract. Culture on chocolate agar with increased CO2. Approved labs only. Many recover spontaneously. Some don't recover even with treatment. Treatment - uterine infusion for 5-7 days with ceftiofur sodium or penicillin, chlorhexidine to wash clitoris and fossa only. Pack external genitals with nitrofurizone or chlorhexidine ointment.
|
|
|
Abortion
|
Viral - EHV1, EHV4 (rarely) - transmission via resptract. Between 5 months and term. Only a few in herd abort. Foals born - viraemia, weak, die shortly after birth. Pregnant kept separate from herd. Vaccinate 3, 5, 7,9 months.
EVA - Togavirus - Severe systemic illness in dam. Fever, lethargy, depression, cj, nd, urticarial rashes, oedema. Abortion. Respiratory or venereal route. Localises in accessory sex glands. Shedder stallions. Mares don't shed. Vaccine available. Bacterial Fungal - small and emaciated foetus. Can survive. Aspergillus. Twinning - 8-10 months. Placental insufficiency - endometrial fibrosis or scarring in older mares. Umbilical cord defects - torsion. Most common (40%) |
|
|
RFM
Sequelae if >8h |
EMERGENCY
More than 3 hours. Oxytocin iv or im every 15 mins. Anti-inflammatories, broad spectrum antibiotics, exercise. Allantochorionic space can be infused with 10-12 litres of saline/povidone iodine - tied shut then can trot mare. Should stimulate contractions. Passed within 30 mins. Laminitis, endometritis. |
|
|
Diagnosis of cryptorchidism
Large testes Small testes Large epididymis Blocked ampullae |
<3 - basal blood sample, give hCG, second blood sample after 30-60 minutes. Elevation of testosterone.
>4 - oestrone sulphate assay. Haematoma - hemicastration if massive and prophylactic antibiotics. Torsion - greater than 270o to stop blood flow. If only 180, developmental which doesn't affect fertility. Acute colic. Hot or cold. Orchitis - primary rare. Hot, swollen, tense, painful. Fever, oedema. Stiff hindlimbs. Ischaemic necrosis and abscess - adhesions. Abs, NSAIDs, hydrotherapy, hemicastration. Tumours. Hypoplasia (congenital), degeneration (subfertility, infertility, chronic inflam 2-6 weeks). May be reversible - takes a few months for sperm to return to normal. Epididimitis, sperm granuloma Spermiostasis - massage and ejaculation. Oxytocin. |
|
|
Penile abnormalities
Haematoma Paraphymosis Balanoposthitis Neoplasia |
Compression bandage and support. Reduce oedema with massage, hydrotherapy, NSAIDs.
Phenothiazine tranquillisers, trauma. Chronic grass sickness. Impairs venous and lymphatic drainage. Becomes oedematous. Cellulitis, necrosis, gangrene if left. Support penis and reduce oedema (hydrotherapy, NSAIDs, diuretics. Inflammation of glans penis and prepuce. - Coital exantema (EHV-3) - pox lesions, venereal, self-limiting, resolution in 3-5 weeks. Inapparent venereal pathogens - silent carrier. Sarcoids (surgical excision if single), SCC (eventually metastasise, cryo), fibropapilloma (regresses in 1-6 months) |
|
|
Loss of libido
Ejaculatory dysfunction Semen abnormalities Abnormal sperm |
Nutrition, systemic diseases, age, management (harsh handling, poor restraint, improper footing), psychic factors, musculoskeletal, hormonal (low LH, can give testosterone or GnRH).
Psychogenic, organic (damage to dorsal nerve of penis, malfunction of ANS, blocked ducts, retrograde ejaculation into bladder). Urospermia - train to urinate before. Haemospermia - Secondary to penile/urethral/ accessory gland lesion. Detached heads - rough handling, long sexual rest. Looped tails - cold shock Coiled tails Immature - Cytoplasmic droplet - excessive sexual use Head abnormalities important as chromosomes here. |
|
|
Manipulation of oestrus
AI Cooled semen Frozen semen |
Progestogens - oestrus occurs 4-5 days after 12-15 day treatment.
Prostaglandin F2 - Cl between 6- 14 days to respond. Heat in 2-5 days. Ovulation 3-10 days. Progesterone/oestradiol hCG - can hasten ovulation of mature follicle GnRH - Twice daily during oestrus to hasten ovulation. Cooled - day before ovulation Frozen within 6 h of ovulation. |
|
|
What conditions cause paresis and weakness?
Key historical features What conditions cause spasticity and hypertonia? Key historical features |
Rhabdomyolysis, botulism, equine motor neurone disease, hyperkalaemic periodic paralysis, hypocalcaemia, myasthenia gravis
Fasciculation/muscle twitching, narrow based stance, increased periods of recumbency, low head carriage, reluctant to bear weight, sudden rapid recumbency, dysphagia. Rhabdomyolysis, tetanus, hypocalcaemia, shivering and stiff horse syndrome Fasciculation, trismus, stiff and stilted gait, other bizarre gait abnormalities, dysphagia. |
|
|
Botulism - weakness
Aetiology CS Clinical pathology Treatment Prevention |
Clostridium botulinum, G+ve, anaerobic, spores. Horses susceptible to toxin types B and C. Toxin blocks ACh release. Peripheral sensory nerves and CNS unaffected. Decaying vegetable matter (silage) and animal carcasses. Ingestion of preformed toxin, growth of agent in GI system, contamination of wounds.
Acute - dyspnoea, severe diffuse paresis, rapid progression to recumbency. Slower over few days. Weakness and trembling. Can't retract tongue. Dysphagia and drooling. Flaccidity of tail. Gradual onset - better prognosis. Fatal - quiet death. Non-fatal recovery weeks to months. Foals - toxicoinfectious botulism/shaker foal. Initially alert. Progression to paresis, stilted gait, muscle tremors. Ptosis and decreased tail tone. Dysphagia. Slow PLR, ileus, constipation, urine retention. Death by respiratory paralysis or pneumonia. Mortality >90%. Toxin in serum, GI content or food. Symptomatic. Antitoxin (in US). Prevent - Vermin control, disposal of carcasses, no spoiled |
|
|
Tetanus - Spasticity/hypertonia
Causal organism Pathophysiology CS Diagnosis Treatment Vaccination |
Clostridium tetani G+ve bacillus. Soil , commensal of GI tract. Spores can persist for many years. Needs anaerobic conditions.
Exotoxin. Spastic contractions of striated muscles. Acts on CNS. Prevents release of inhibitory neurotransmitters. Tetanolysin - necrosis and exudation. Stilted gait, difficulty eating, generalised spastic muscle contrations. May worsen quickly over 24 hours or take several days. Square on four limbs, tail erect, neck extended. Ears erect. Seating, tachycardia. Drooling. Progression to recumbency and death CS, not vaccinated, CPK levels Each case consider prognosis and welfare. Recumbent - euth. Best cases mild clinical signs over several days and if can still eat and drink. Quiet dark stable, soft bedding, elevate food and water, soft moist food, quiet gentle handling. ACP, procine pen, anti toxin, hydrogen peroxide around wound. 2, 4-6 weeks apart then booster one year later. Mares one month prior to foaling. Foals unvac dam - antitoxin. |
|
|
Acute rhabdomyolysis
History and clinical signs Diagnosis Pathological finding |
Working horses and ponies.
Slight change in gait to unable to move. Recumbency and death in some. During or following exercise. Sometimes not associated with exercise. Hindlimbs. and lumbar muscles. Stiff, painful hard and swollen. Distressed, sweating, pyrexic. May become recumbent. Shivering, muscle atrophy, can't lift limbs properly. Red brown urine myoglobin. In order that appear: CK (most specific for skeletal muscle, rises first and disappears first peaks 2-12 hours, disappears 24-36 hours), LDH (peaks at 15 hours), AST (peaks at 24 hours, remains for 3 weeks). Myoglobin in urine. Pale discolouration of affected muscles. Degeneration and swelling of muscle fibres. |
|
|
Treatment of acute tying up
|
Rest, analgesia (NSAIDs - flunixin meglumine), fluids, sedatives (ACP) - aleviates anxiety and muscle spasm, may also promote peripheral vasodilation. CS - short acting but laminitis. Calcium carbonate and calcium gluconate.
|
|
|
Chronic tying up
Investigation Treatment |
Recurrent exertional rhabdomyolysis (TB fillies), idiopathic chronic exertional, glycogen storage disorders (polysaccharide storage myopathy - QH, glycogen branching enzyme deficiency, equine polysaccharide storage myopathy).
Exercise - blood samples prior and 2-6 hours after. No more than doubling of CK, no more than 50% increase in AST. No signs of stiffness. Muscle biopsy. Fractional electrolyte excretion test. Diet - reduce CHO, exercise - no breaks in routine, stress avoidance, drugs (ACP, dantrolene), salt, vitamin E and selenium. |
|
|
Collapse
|
Neuro - seizure, cervical vertebral stenosis, narcolepsy, inappropriate sleep, botulism
Cardiovascular - Arrhythmias, haemorrhage, heart failure, aorto-iliac thrombosis, neurocardiogenic collapse. Metabolic and nutritional - Hypocalcaemia, hypoglycaemia Toxic - Monensin toxicosis Miscellaneous - Systemic anaphylaxis, air emboli, musculoskeletal abnormalities, severe myopathy. |
|
|
Foals
History Immune disorders |
Mother, parturition, foal conditions, abnormal post-partum behaviour, premature/dysmature.
Failure of passive transfer - Fail to suck. Measure neonatal serum IgG from 8h - 24h onwards. Can't do >2 weeks. Tx - <24h - 1-2 L colostrum, lasts in freezer 12 months, can use cow. >24 hours - intestinal absorption of IgG stopped so give 1-2 L plasma iv. Neonatal isoerythrolysis - immune-mediated haemolytic anaemia. Destruction of foal's RBCs by colostral antibodies directed against foal's RBC membrane alloantigens. Don't get it in first partum mares. Normal at birth, signs at 6-48 hours - anaemia, weakness, icterus, haemoglobinuria, depression, anorexia, collapse and death. Prevent further absorption of mare's colostral Ig. Alternative milk until >24 hours. Blood transfusion if PCV <10%. Don't mate Aa or Qa -ve mares with Aa or Qa +ve stallions. |
|
|
Neonatal septicaemia
|
Guarded prognosis. GIT, lung, umbilicus, iatrogenic entry. Rare in utero. Signs 48-96 h. Environmental bacteria mostly G-ve. Lungs, bones, GIT sites of sepsis. Non-specific signs, reduced appetite, decreased sucking, dull, recumbency, pyrexia. Multisystemic - including meningitis, diarrhoea, lameness, scleral injection. Blood culture. Band and toxic neutrophils. Fibrinogen. IgG low. Hypoglycaemia, low PaO2, metabolic acidosis. Treatment - broad spec antibiotics (penicillin and gentamicin. C+S. Treat >1-2 weeks after signs resolved. Local therapy e.g. joint lavage. IgGs.
|
|
|
Foal diarrhoea
|
Foal heat diarrhoea - 6-14 days, adapt from milk to grass diet and start coprophagy. Self-curing.
Nutritional diarrhoea - overingestion of milk Rotavirus - main cause. Adults sources. <1 months die. >1 month mild enteritis. Profuse watery diarrhoea, depression. Stunting of villi. Antisera or fluids. Avoid overstocking. Vaccinate mare in 8th, 9th and 10th monthgestation. Salmonellosis - Mare source. Mild enteritis. MAy cause severe septicaemia. Foetid diarrhoea or colic. Clostridium perfringens types A, B and C - foetid necrotising haemorrhagic enteritis in 1-2 day old foals. Death in 48 hours. Septicaemia - diarrhoea is common presenting sign. |
|
|
Management of diarrhoeic foals
|
Fluids, antibiotics if bacterial, adsorbents - bismuth subsalicylate. NSAIDs reduce endotoxaemia. Codeine only if severe and profuse. Plasma if FPT, probiotics, anti-ulcer, nutrition - keep on mare's milk if mild or electrolyte solutions, hygiene, nursing.
|
|
|
Foal with abdominal pain
|
Gastroduodenal ulceration - Stress, NSAIDs, infections. Symptomatic - from day 1 onwards - anorexia, salivation, colic after sucking, regurgitation, perforation rare. CS, response to therapy - omeprazole (PPI).
Meconium retention - Voided within few hours. Mainly in males. 6-24h - restless, lift tail, roll, lie on back, try to urinate, straining reopens urachus. Careful digital rectal exam. Warm soapy water enema with soft tube 10-12 inches. If non-responsive, liquid paraffin or dioctyl by stomach tube. Surgical intervention - rare. Tyzzer's disease - Uncommon in UK. Infectious necrotic hepatitis caused by Clostridium piliformis. Foals 1-6 weeks old. Sudden death or acute abdo pain, depression. Penicillin but most die. Uroperitoneum - Ruptured bladder, patent urachus. Dorsal midline rupture. 3-7 do. Abdo distension, lethargy, tachyp, tachyc, cairculatory failure, mild abdo pain. Azotaemia, hyperk, hypon and c, metabolic acidosis. Drain, iv saline and dextrose, AB. Sx. |
|
|
Neurological conditions of foal
|
Perinatal asphyxia syndrome - barker foals. Peripartum hypoxia/ischaemia. Normal several hours to 1 day before seizures, ataxia, disorientation, recumbency, coma. Seconfary FPT, dehydration, hypoglycaemia, metabolic and respiratory acidosis. Steroids or DMSO? Control seizures with diazepam. Nursing - nutrition, heat, fluids, ABs, IgG, intranasal oxygen. Many stabilise 2-3 days, several weeks for full recovery. Poor prognosis if no improvement in 48h.
Septic meningoencephalitis - 75% of septic foals. Depression, coma, seizures, stiff neck, weak, tetraplegia. CSF protein and neutrophil count. Hypoglycaemia - CNS signs with fasting, stress, hypothermia, sepsis, sick. Weak, lethargic, depression, reduced sucking, recumbent, hypothermia, coma/seizures. 5-10% glucose iv. |
|
|
What parameters cause haematology parameters to vary between horses?
What causes changes in sodium levels? Changes in serum potassium Changes in serum chloride Calcium - ionised |
Age - neonates and adults.
Different labs Hot-blooded (athletic) and cold-blooded (ponies and draft breeds) Sample collection and handling. Changes in water balance Affected by factors that alter internal balance (distribution of K between ECF and ICF). Hypokalaemia: Altered external balance - depleted K stores - diarrhoea, 3rd space losses, deficiency. Altered internal balance - ECF to ICF - metabolic alkalosis, bicarbonate administration. Hyperkalaemia: False - in vitro haemolysis, altered external balance - hypovolaemia, altered internal balance - metabolic acidosis. Mostly associated with changes in Na. When not - inversely to bicarbonate. Increase compared to Na - metabolic acidosis or compensation for respiratory alkalosis. Decreases - metabolic alkalosis or compensation for resp acidosis. Hypo - ARF, exhaustive disease, transit, lactation Hyper - CRF, hypervitaminosis D, hyperPT, pseudohyperPT (PNpS) |
|
|
Acid base
Metabolic acidosis Metabolic alkalosis Respiratory acidosis Respiratory alkalosis - rare |
Hypovolaemia, acute colitis, bowel strangulation, exercise above anaerobic threshold. Decreased pH, increased H+. Primary - decreased HCO3-
Gastric reflux (H+, Cl- loss), excessive sweating (disproportionate NaCl loss), prolonged salivary losses (Cl- loss). Increased pH, decreased H+. Primary - increased HCO3- Primary upper/lower airway disease, decreased alveolar ventilation. Decreased pH, increased H+, increased PCO2 Hyperventilation, increased pH, decreased H+, primary - decreased PCO2. |
|
|
Anion gap
Decreased Increased |
[Na + K] - [Cl + HCO3]
Normally 12-16 Approximation of unmeasured anions - proteins, sulphate, phosphate, lactate. Hypoproteinaemia, hyperchloaemia metabolic acidosis Lactic acidosis (anaerobic exercise, grain overload, hypovolaemia) |
|
|
Serum enzymes
GLDH GGT AST AP CK |
Hepatocellular. Liver specific. Short half life.
Hepatobiliary disorders and cholestasis. Pancreas, renal tubular cells, periportal liver. Longer half life. Skeletal and cardiac muscle, liver, kidney, erythrocytes. Long half life. Intra or extra hepatic obstruction of biliary system. Bone, intestine, neutrophils. Liver and biliary stasis. Specific to skeletal muscle. Exertional rhabdomyolysis, recumbency, intramuscular injections. Short half life. With AST and LDH for muscle damage. |
|
|
Bilirubin
2 types Elevations Glucose Hypo Hyper |
Unconjugated (albumin bound), conjugated (liver)
Haemolysis - unconjugated, liver disease (C + UC), if >25% total conjugated suggests biliary obstruction. Anorexia (unconjugated). Fasting, septicaemia, endotoxaemia, hyperlipaemia Stress, excited, endotoxaemia (initially), Cushing's |
|
|
Creatinine (and BUN)
Elevations Serum proteins Hyper Hypo |
From skeletal muscle. Excreted by kidneys.
Prerenal azotaemia, renal azotaemia, post renal. Normal foals. Panhyperproteinaemia -Dehydration. Hyperglobulinaemia (chronic antigenic stimulation) Pan - Acute protein losing colitis, acute blood loss Hypoalbuminaemia - Decreased production in liver disease, increased breakdown (metabolism, antigenic stimulation), increased loss - GI/renal |
|
|
Erythron
Anaemia Mean cell volume Mean cell Hb MCHC (Hbx100/PCV) - mean cell haemoglobin concentration Polycythaemia |
Decreased PCV and RBCC - blood loss, increased RBC destruction, inadequate RBC production
Increase - regenerative Decrease - iron deficiency Increase - haemolysis Decrease - iron deficiency Increase - haemolysis Decrease - iron deficiency Increase in PCV, RBC count, haemoglobin Absolute - Increased erythropoeitin - appropriate (chronic hypoxia high altitude) or inappropriate (renal/hepatic neoplasia). Relative - dehydration, splenic contraction. |
|
|
Leucogram
Physiological leucocytosis Neutrophilia Neutropenia Lymphocytosis Lymphopaenia Monocytosis Eosinophilia |
Adrenaline (stress/excitement - neutrophilia, lymphocytosis), corticosteroid (neutrophilia, lymphopaenia)
Inflam, bac, left shift - regenerative Decreased production, increased consumption (large surface area of inflam), endotoxaemia, left shift (immature excede mature), some viral disease (EHV1, equine influenza) Rare - chronic viral, autoimmune, leukaemia Acute viral disease, endotoxaemia Chronic inflammation Uncommon even with parasitism |
|
|
Urinalysis
SG pH Protein Glucose Blood Cells Casts Crystals Bacteria |
Normal 1.020-1.050. Failure to concentrate - primary renal disease, DI, medullary washout.
7-9, foals slightly acidic Not normally in urine. Glomerular loss or UTI. Not present unless blood glucose exceeds threshold. Cushings, glucocorticoids, adrenaline. Glucosuria without hyperglycaemia - renal tubule damage. Myoglobin, haemoglobin, haematuria. Up to 5 red or white cells per HPF normal. Increased RBCs - neoplasia, trauma, inflam, coagulopathy. Leukocytes - inflam. Protein and cellular material - tubular damage. Not seen in stored/non-refrigerated as fragile. Calcium carbonate - abundant in horse urine Significant amounts if infection |
|
|
Most likely bacteria in the following infections:
Traumatic wounds, respiratory, septic foals Antimicrobials available in Equine medicine Factors contributing to antimicrobial failure Prophylaxis Antifungals Hospital acquired infections |
Skin and faecal flora, streptococcus, E.coli and other enteric G-ve
Penicillin, cephalosporins, aminoglycosides (gentamicin - often in combinations with penicillin for example), potentiated sulphonamides, FQs, oxytet, metronidazole, macrolides, rifampin Depressed immune system, poor owner compliance, FB/abscess, pharmacokinetics, incorrect dose, wrong diagnosis, incorrect choice, resistance. Use cidal - TMPS, penicillins. Strangles - penicillins for in contact horses with no signs. Enilconazole - dermatophytosis. Or natamycin. Both can be used for guttural pouch mycosis. Enteric - Salmonellosis, Clostridium difficile. Both associated with antibiotic use. Surgical sites - MRSA - nasal carriage Respiratory - Influenza, EHV, EVA, EIA, Strangles Skin - Dermatophytosis, pediculosis, mange |
|
|
Vaccination
Equine influenza Tetanus EHV EVA Rotavirus Strangles Equine plasma |
2 primary vaccinations, 6 month then yearly booster.
First vaccination from 6 months old then 21-92 days later, then 150-215 days. Booster must be within 365 days. If over, must re-start. Antitoxin if not already vaccinated and horse obtains injury. Administer at remote site to vaccination. Fisrt day of life for foals espec if mare not vaccinated. Toxoid - 2 vaccinations a month appart then boosters every 2-3 years. booster mare 6 weeks before birth. EHV1 and 4 - young performance horses. Primary course 2 vaccines 4 weeks apart. Boosters every 6 months. EHV1 for breeding mares - 5, 7 and 9 months pregnancy. (Maybe 3 months too). Establish negative first. 2 vaccinations then yearly booster. Pregnant mares 4-6 weeks then booster every 6 months. Musocal injection. Live-modified. FPT. |
|
|
Parasite control
Available drugs Dosing strategies Ascarid infections Tapeworm Gastrophilus (bots) Strongyloides westeri |
Macrocyclic lactones - Ivermectin,moxidectin; FBZ, Praziquantel, Pyrantel
New horses - 5 d FBZ and/or moxidection/ivermectin. Interval dosing - specific drug at regular time intervals during high risk summer grazing. Strategic dosing - Specific times of year to disrupt seasonal cycle transmission. Dose at turn-out, mid grazing and autumn. Care with abnormal weather. Problem if heavy burden horses introduced. Targeted strategic dosing - FWEC - 80% worms in 20% horses. >200 eggs per gram - treat. Include larvicidal dosing for young susceptible as mucosal larvae not picked up by FWEC. Tapeworm ELISA every 1-2 years. FWEC won't detect high burden of encysted cyathostomes. Pregnant mares 1 month before foaling FBZ/ivermectin then 10 d after foaling. Foals at 6 weeks then 1 month until 6 m, every 6 weeks after. Impaction in foals if high. Spasmodic colic, impactions. ELISA. Anti-cestode yearly (Ps) Treat after first frost winter - McL Via milk - diarrh, tx 1- 2 wo |
|
|
Nutritional support of sick animal
|
Increase energy density with vegetable oil, add protein - alfalfa, soybean meal.
Enteral feeding, parenteral Foals - mare's milk, milk replacer, goat's milk. Hourly initially. Gain 1kg/d. Orphan - foster mare. 20% bwt every 20-30 minutes. Bottle then bucket. |
|
|
Emerging equine diseases
African horse sickness West nile virus Equine infectious anaemia |
Orbivirus, Culicoides. Multiplies in LN, epithelium of target organs. Effusions and oedema. Pulmonary - dyspnoea, death hours. Cardiac - sc oedema of head and neck, death days. Mixed - progresses to other - 50% mortality. Horse sickness fever - low mort, pyr, anor. ELISA, PCR. Notifiable. Euth affected, destroy carcases. Vacc of uninfected. Perimeter vacc to limit spread. No vacc in UK.
Flavivirus. Birds, culex mosquitoes. Horses and humans dead-end. Dead birds precede. Behaviour, CN deficits, ataxia, muscle fasciculations, can progress to paralysis of one or more limbs - euth or die. May recover. Serology, PCR, ImHC. Notifiable. Hyperimmune plasma, IFNa, supportive. Vacc. Reduce mosquito exposure. Lentivirus. Flies, blood, equipment, vertical transmission, low risk - secretions. Recurrent pyrexia, depression, WL, ventral oedema, anaemia, thrombocytopenia, can be fatal, all carriers. Coggins test, ELISA, notifiable. No cure, no vacc. Euth. Movement and vector control, hygiene. |
|
|
Toxicity
|
Ragwort - 2o photosensitisation
Yew - alkaloids - collapse, sudden death. Foxglove - digitalis - altered cardiac conduction. Oak - colic, tenesmus, haem d, tachyc, tachyp, sudden de. Supportive tx. Selenium - Acute (oversupplementation) - weak, colic, d, arrythmias, dyspnoea. Chronic poisoning - loss of mane and tail, laminitis. Remove source, feed high protein. Aflatoxicosis - Aspergillus - CHOs. Liver disease, colic, can be fatal. Ryegrass staggers - Symbiotic endophyte. Neurotoxic alkaloids. Diffuse vestibulocerebellar syndrome, ataxia, tremors, proprioceptive deficits, can recover when food source removed. Zootoxins - blister beetle - inflam and necrosis of GIT. Severe colic, hypocal. Can be fatal. Lead - weak, WL, dysphagia, tremors, laryngeal paralysis. Anticholinesterase insecticides - Salivation, colic, CNS depression or stimulation, death maybe. Atropine. Warfarin - haem. Vit K tx Vit K tox - CRF Monensin - Hypovol, ataxia, death |
|
|
Treatment of periocular sarcoids
Ulcerative/destructive SCC Conjunctivits Melting ulcers Viral ulcers |
(Fibroblastic common in this site) - surgical excision, BCG, radiation.
Non-pigmented eyelids and third eyelid. Malignant - spread to local lymph nodes. Surgical excision, cryo and irradiation with strontium. Opportunistic bacteria related to flies or part of URT viruses. Broad spectrum antibiotics 5 days, fly control. Tendency to form these. Treat aggressively every 2 hours until melting stops with FQ. Gentamicin second choice. Atropine to treat uveitis. Anti-collagenase agents including saline in EDTA vacutainer or patient's serum. Early referral. Very painful. Punctate or linear. Anti-viral therapy works well. Apply frequently for first 48 hours then 4-6 times daily. Self limiting. |
|
|
Nerve blocks for eye examination
|
Palpebral nerve block - palpable over zygomatic arch. 2ml mepivicaine. Proxymetacaine squirted onto eye will provide anaesthetic of surface of eye. Tropicamide/atropine mydriatic.
|
|
|
Equine recurrent uveitis
CS Tx |
Leptospira. Acute nongranulomatous inflammation of uveal tract, auto-aggressive T-cell mediated disease. Acute, unilateral. Further attacks common in same eye. Other one can become effected too. May be associated to systemic infectious disease.
Pain (sedate), chemosis and lid oedema, marked miosis, iris looks dull and swollen, aqueous flare and hypopyon. Intra-ocular pressure reduced. Posterior segment may be involved. Complications - atrophy of granulae iridicae, posterior senechiae, iris rests, alterations in pigmentation, cataract formation. Glaucoma may develop. Can fail horse on prepurchase exam if signs of previous uveitis. Box rest in dark, lavage system. Systemic anti-inflammatory - flunixin meglumine top end of dose range for 5 days initially. 2 weeks, taper off 2 weeks after resolution of signs. Omeprazole. Systemic CS if severe - beware laminitis. Mydriatics - atropine. Topical CS gradually reducing - not in ulcerated. Cyclosporine implant (specialist). |
|
|
Post-inflammatory lesions of the eye
|
Butterfly lesions or bullet hole lesions. EHV? Insignificant as small.
|

