![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
162 Cards in this Set
- Front
- Back
|
where does endochondral ossification occur?
|
epiphysis
metaphyseal growth plate secondary centers of ossification |
|
|
What percentage of total collagen of the articular cartilage does type II collagen comprise?
|
90% of total
|
|
|
What are proteoglycans in articular cartilage?
|
the other major solid component of articular cartilage
consists of protein core covalently attached to GAG chains Aggrecan |
|
|
Pastern Joint Lesions
|
early lameness and DJD
lameness exam: positive flexion, IA block best predominantly SCC |
|
|
Coffin Joint SCC
|
Predominantly SCC
lameness exam: no swelling/effusion, digital flexion positive, IA anesthesia won't reach arthroscopically --- must access through hoof wall |
|
|
OCD lesions: treatment goal
|
removal of fragment and loose cartilage
debride parent bone to healthy bone with firm margins general success is good |
|
|
Subchondral Cystic Lesions: treatment goal
|
approach is to debride (enucleate) the cavity
-remove fibrous lining and sclerotic bony margin - don't drill the cavity generally arthroscopic results vary with joint |
|
|
Extensor Process OCD
|
confirm diagnosis as there are many separate centers of ossification and many extensor tendon calcifications
block the joint operate arthroscopically--- only site in coffin joint that you can see!!! |
|
|
Fetlock Joint OCD
|
multiple or all joints
lameness exam: lameness variable (can be complicated by multi. joints); fetlock effusion; IA block of one of the joints arthroscopic procedure (explore all joints with effusion) generally good prognosis (non-weightbearing surface) |
|
|
Fetlock Joint SCC
|
demonstrated earlier than OCD
lameness exam: effusion approx 50%, positive flexion medial condyle usually surgical outcome 80% in one report |
|
|
Carpus OCD/SCC
|
less commonly affected
distal radial SCC lameness exam |
|
|
Elbow joint SCC
|
less common
lameness exam: presents similar to shoulder; elongated heel probable -gen. SCC in medial proximal radial condyle not arthroscopically access. don't do very well exhaust conserv. therapy (intralesional DepoMed) |
|
|
Elbow Joint OCD
|
less common
lameness exam: present similar to shoulder; elongated heel probable gen. distal humeral condyle gen. not arthroscop. accessible exhaust conserv. therapy |
|
|
Shoulder Joint -Humeral OCD
|
Common
gen. do better than expected but not always (difficult to predict) lameness exam: elongated heel; flexion equivocal often radiographically obscure lesion arthroscopic procedure |
|
|
Shoulder Joint- Glenoid SCC
|
diagnosis same as OCD
may coexist difficult to access on concave glenoid |
|
|
Tibiotarsal Joint OCD
|
very common (uncommon SCC on trochlear ridges)
gen. present early b/c visible effusion lameness exam: minimal lameness; may req. flexion to see; obvious bog spavin gen. operate in athletes |
|
|
Tarsal sites of predilection of OCD
|
distal intermediate ridge of tibia
medial malleolus of tibia distal lateral trochlear ridge of tibialtarsal bone anywhere else..... always examine all views and explore entire joint |
|
|
Femoropatellar joints: OCD and SCC
|
OCD very common
SCC uncommon lameness exam: mild or severe ---worse in younger horses prominent effusion lateral trochlear ridge much more common |
|
|
three classifications of SCC (communication only)
|
type I: dome shape
type II: circular with narrow channel to joint surface type III: dimple |
|
|
femorotibial joints
|
SCC very common
OCD uncommon Lameness exam: IA anesthesia, 50% improvement usually medial FT joint |
|
|
Coxofemoral Joint
|
lameness exam: positive flexion, IA anesthesia
femoral head subchondral cystic lesions |
|
|
Immobilization of fractures
|
prevent closed fractures from opening!!!!!!!!!!!!!
minimize cartilage damage with articular fractures (condylar fractures, P1 fractures) |
|
|
Make sure to immobilize the joint _______ and __________ to fracture
|
proximal and distal
--- may have to fudge in some cases |
|
|
Types of forces you must neutralize with field splints
|
torsion
shear bending |
|
|
What is a Kimsey Splint?
|
there is both the lower limb and the full limb
--- have it ready with the screws already in extension and bandages ready to apply |
|
|
suggestions for the contents of a splint box
|
bandage material - lots of cotton bandaging material
nonadherent dressings for bandaging open wounds two premade half limb splints sized for an adult horse and one full limb splint a saw to cut the splints to the appropriate length inelastic tape or casting tape fracture stabilization notes |
|
|
what is the best way to apply the padding for splinting?
|
thing layers in sequential layers works best at conforming
|
|
|
how long does complete bone healing take in adult horses? Foals?
|
adult horses - 4 months
foals - 2-3 months |
|
|
P2 fractures
|
rotational injury
racehorses shoes with toe grabs |
|
|
condylar fractures
|
lateral more common
--- usually lag well --- variable articular damage leading to OA medial condylar fractures usually course proximally and are comminuted |
|
|
Malposition of the deep flexor tendon causes what deformity?
|
varus deformity
----must be repositioned as early as possible |
|
|
what do you see with a central tarsal slab fracture?
|
characteristic wide gait
can be bilateral lag screw repair may require arthrodesis |
|
|
what is the treatment for adult horses with midshaft tibial fractures?
|
euthanasia
|
|
|
Early Lateral Trochlear Ridge OCD
|
weanling - yearling
present w/ femoropatellar effusion variable lameness but may be worse than usual w/ OCD min. to no radiographic changes medicate and recheck in a few weeks |
|
|
Cruciate Injury
|
variable outcome
can only debride frayed fibers if horse can walk and there is no DJD, give benefit of the doubt 1 year recovery continuous anti-inflamm. meds |
|
|
Fractures of the head
|
see most often in stallions and youngsters
generally do well --- self contained and good blood supply |
|
|
Fractures of the head: dx
|
misalighment/malocclusion (oral)
swelling pain salivation/hemorrhage odor with time beneath masseters can be more difficult *** |
|
|
standing repairs for fractures of the head
|
can do this for rostral fractures
xylazine/detomidine local not usu. required (mental or infraorbital nerves if necessary) |
|
|
for fixation of oral fractures the tension side is....
|
tension side is the oral side of the mandible or maxilla
|
|
|
_______________ is very effective for fractures back to cheek teeth.
|
Tension band wiring
|
|
|
______________ is effective for fractures along cheek teeth or caudal ramus.
|
Plating
|
|
|
what are postoperative considerations after oral fracture repair?
|
hay is usually best (b/c use only cheek teeth for grinding)
better to avoid grazing hardware removal --- remove wires, remove plates only if draining may need to address sequestra or tooth abscess |
|
|
cervical fractures: signalment
|
younger horses more commonly presented
older horses -- often catastrophic |
|
|
cervical fractures: therapy
|
unless neurological status - conservative
--neck brace or cast --can decompress fracture callus later --domino effect described |
|
|
fracture of the dens
|
often deteriorate and req. stabilization
pins dens removal and A-A arthrodesis (neck brace to support) lose some lateral range of motion |
|
|
fracture/subluxation of atlas and axis
|
can present minimal neuro deficit
need VD view to image completely often already in healing stage (w/ neuro deficit due to callus) laminectomy definitely worth surgery |
|
|
Atlanto-axial luxation presentation
|
usually present in chronic stage
may have no neuro effect no need to reduce (couldn't) |
|
|
Mid and caudal cervical fractures
|
avoid (acute) sx if possible
ventral plating (not tension side) - need radiogrpahic control - accompany interbody fusion - as long a plate as possible laminectomy after longer durations |
|
|
what are the two keys to good feet in a horse?
|
good conformation (selection)
conscientious foot care (farrier, nutrition, environment) |
|
|
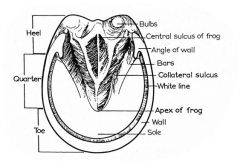
What 3 parts make up the hoof?
|
hoof wall
sole frog |
|
|
the hoof wall is thickest at _______ and becomes thinner and more elastic _________.
|
thickest at the toe and becomes thinner and more elastic toward the heel
|
|
|
the __________ hoof wall is usually straighter (less curved) and more upright (steeper) than __________ hoof wall.
|
inside hoof wall is straighter and more upright than the outside hoof wall
|
|
Label this picture
|
|
|
|
what are some important structure found within the hoof
|
corium (dermis)
coffin bone coffin joint navicular bone and bursa deep digital flexor tendon |
|
|
what is the anatomy and function of the corium/dermis?
|
sensitive (contains nerve endings), blood rich tissue that lines the inside of the hoof
produces and nourishes the hoof and also serves to attach the coffin bone to the hoof |
|
|
what ar ethe projections from the corium/dermis and the inner hoof wall that form a strong and flexible bond
|
the projections are the lamellae and the region is the lamina
--- the lamellae also have secondary projections which are the secondary lamellae |
|
|
the coffin bone (and therefore the weight of the horse) is suspended within the hoof by ____________.
|
the laminar attachment
|
|
|
What is laminitis
|
inflammation of the lamellae
--- damage to the lamellar bond may lead to separation of the coffin bone from the hoof wall |
|
|
the hoof wall grows from the coronary band downward at a rate of __________ per month
|
6-10 mm (1/3 in.)
|
|
|
What are some shoeing problems caused by horses with slow hoof growth rates?
|
the farrier will have to alter the paths of his nails in order to avoid old nail holes
this ay alter the tightness of the shoes |
|
|
What is the appropriate foot confirmation of a horse?
|
---the hooves should be of sufficient size for the body weight
---hoof wall should be thick enough to allow adequate base of support ---should be wider at the ground surface than at the coronary band to allow normal movement/expansion ---inside and outside walls should bear weight evenly ---sole should be slightly concave and not bear weight |
|
|
the angle of the hoof is considered correct when ________________. This is referred to as ______________.
|
the hoof and pastern are in alignment -- the slope of the front of the hoof wall should match the slope of the pastern
this is a matched hoof-pastern axis |
|
|
the normal angle of front hooves averages ______
the normal angle of hind hooves averages _____ |
front hooves --- 54 degrees
hind hooves --- 56 degrees |
|
|
What problems do low hoof angles cause?
|
low hoof angles increase the weight supported by the heel region (navicular region) and makes breakover more difficult
|
|
|
What does a raised hoof angle cause?
|
the coffin joint becomes more flexed and the pastern segment becomes more sloped (and the fetlock drops)
|
|
|
what is the main reason we shoe horses' feet?
|
to protect the hooves from excessive wear which would result in lameness
|
|
|
what are some other reasons for shoeing horses?
|
protect hooves
provide traction correct or influence the stance and/or gait correct or improve abnormal or pathological conditions of the feet and legs |
|
|
shoes should be set _________ and ________ to provide support and allow for hoof growth
|
full and long
|
|
|
what is the "ideal" point of breakover?
|
approximately 1.5 inches in front of the apex of the frog
|
|
|
What is white line disease?
|
the breakdown of hoof wall
--- can be caused by the combination of urine and manure which provides a perfect medium for the growth of bacteria and fungi |
|
|
What are basal cells
|
they are a part of the epidermis
contain matrix metalloproteinases (MMPs) - anchoring filaments are substrates for MMP activity -precise MMP activity allows the growing hoof wall to move past the stationary distal phalanx |
|
|
____________ is the only connection between the dermis and the epidermis of the foot.
|
the basement membrane
|
|
|
What is indicated by a convex or dropped sole?
|
that the horse has laminitis
|
|
|
What is broken backwards?
|
the pastern angle is steeper than the angle of the hoof
--- will see tendon, ligament, joint problems --- will be predisposed to osteoarthritis |
|
|
What is broken forward?
|
the hoof angle is steeper than the angle of the pastern
--- most of the load stress is going through the suspensory tendon coming around the back |
|
|
What are underrun heels?
|
when the heel angle is 5 degrees (or more) less than the toe angle
puts the heels further under the foot than ideal and results in increased concussion to palmar structures of foot (see probs w/ navicular disease, heel bruises, quarter cracks) |
|
|
What is a club foot?
|
one that has a hoof angle of 60 degrees or more
usu. the result of a flexure deformity of the distal interphalangeal joint |
|
|
What is wry foot?
|
term for a distorted foot which is no longer centered under the limb
the medial hoof wall usually rolls under (narrower at ground surface than at coronary band) while the lateral hoof wall flares |
|
|
what are sheared heels?
|
descriptive term for the structural breakdown that occurs between the heel bulbs with the disproportionate use of one heel
--- may result in chronic heel soreness and hoof cracks (quarter cracks) *****DP radiograph of foot is critical to guide trimming |
|
|
What are contracted heels?
|
the hoof wall at the heels is closer than normal and the frog is atrophied
--- really a sign of another problem - the horse isn't loading his foot appropriately |
|
|
What are flat feet?
|
the flat foot lacks the natural (normal) concavity of the sole
-- predisposes to sole bruising and subsequent lameness |
|
|
What is the problem with thin walls and sole?
|
-predisposes horse to many probs and difficult to keep sound
---bruising ---shoeing problems --- difficult to drive good nails without penetrating or coming close to the sensitive tissue |
|
|
___________ rings or lines around the circumference of the hoof wall are considered normal. ____________ rings are abnormal.
|
parallel rings or lines -- normal
divergent rings (wider at heel than the toe) --- abnormal |
|
|
What is the cause of divergent rings on the hoof?
|
result of laminitis -- systemic or mechanical
the hoof wall is growing quicker at the heel than the toe |
|
|
What causes parallel rings?
|
stress, nutritional, climatic or body temp changes, irritating substances on the coronary band
|
|
|
Corns refer specifically to what?
|
bruises occuring between the bars and the wall of the foot
|
|
|
When will you see discolored areas that are evidence of bruising?
|
may not see at initial exam
depends on duration of the problem (typically see if chronic problem) |
|
|
What do you need to differentiate bruises from?
|
subsolar abscesses and coffin bone fractures
|
|
|
What is the most common cause of lameness in horses?
|
subsolar abscesses
|
|
|
what is thrush?
|
degenerative condition of the frog due to bacterial infection
the infection may penetrate the cornified tissues and involve sensitive structures |
|
|
Thrush: clinical signs and dx
|
degeneration of the frog
+/- pain with hoof testers -- lameness depending on involvement of sensitive tissues must determine whether a primary or secondary problem (navicular disease) |
|
|
What is canker?
|
a chronic hypertrophy of the horn producing tissues of the foot
-- uncommon condition |
|
|
What is the etiology of canker?
|
unhygienic stabling
poor hoof care presumably a gram-negative coccobacillary microbial infection in the stratum germinativum layer of the frog or sole infection causes dyskeratosis |
|
|
what are the clinical signs and diagnosis for canker?
|
moist exudative dermatitis affecting the frog and/or the sole
germinal layers of the foot produce an abnormal hypertrophic horn with a copious foul-smelling exudate |
|
|
What is the treatment for canker?
|
adequate stabling and foot care
radical debridement of affected tissues daily soaking in epsom salt solution followed by bandaging in an antiseptic dressing very difficult to treat |
|
|
What is a keratoma?
|
uncommon disorder of the hoof wall and is best described as a tumor of the keratin producing cells of the hoof wall
the tumor is interposed between the hoof wall and the underlying third phalanx ----recurrent abscesses are a big key to keratomas -- they are always in the same spot |
|
|
How do you treat a keratoma?
|
the tumor must be removed in its entirety or it will regrow
hoof wall overlying the keratoma is resected, the keratoma is removed and abnormal appearing lamina and bone debrided the hoof defect is treated as a hoof wall avulsion prognosis - good with complete resection |
|
|
How are hoof cracks described?
|
location (toe, quarter, heel)
depth (superficial or deep) origin (ground surface of the coronary band) length (complete or incomplete) |
|
|
What is pedal osteitis?
|
implies inflammation or inflammatory changes of the third phalanx
these changes are prob. related to concussion, causing chronic bruising and inflamm. of the sole and third phalanx |
|
|
What are the clinical signs seen with pedal osteitis and how is it dx?
|
CS/Dx:
mild forelimb lameness short choppy gait worse on hard surfaces +/- hoof tester sensitivity diagnostic anesthesia nuclear bone scan - most accurate way to confirm radiographs |
|
|
What are sidebones?
|
lay term for describing the ossification of the collateral cartilages
common in draft horses -- assoc. w/ lameness is debated normal aging process to some degree |
|
|
Sidebones may accompany other lameness such as ____________ and may be mistaken for the cause.
|
navicular disease
|
|
|
What is quittor?
|
lay term referring to chronic infection and necrosis of a collateral cartilage of the third phalanx
|
|
|
What is the etiology of quittor?
|
direct injury and subsequent infection from puncture wounds or lacerations
secondary to penetrating wounds through the solar surface of the foot |
|
|
What are the clinical signs/dx for quittor?
|
draining tract over the collateral cartilage just above the coronary band
failure to respond to conservative treatment Hx may indicate healing followed by recurrence of a draining tract radiographs using a probe or contrast media |
|
|
How is quittor treated?
|
surgical excision of the necrotic cartilage ( be careful of entering the coffin joint )
total cure may be difficult |
|
|
What is an angular limb deformity?
|
lateral or medial deviation to the long axis of the bone in the frontal plane
|
|
|
What is valgus?
|
lateral deviation distal to the point of angulation (pivot point)
- often accompanied by outward rotational deformity |
|
|
What is varus?
|
medial deviation distal to the point of angulation (pivot point)
- often accompanied by inward rotational deformity |
|
|
___________ rotational deformity often corrects with time as the chest widens with growth.
|
Outward rotational deformity
|
|
|
What are the risk factors for angular limb deformities?
|
age (foals of all ages but usu. young)
breed (all breeds and partic. in rapidly growing foals) sex (both sexes, but slightly higher in colts) limb (most often front limbs - uni or bilateral) site - carpus, fetlock, metacarpophalangeal/metatarsophalangeal, and tarsus |
|
|
What is the most commonly seen ALD?
|
carpal valgus > fetlock varus > tarsal deformities
|
|
|
What are some causes of ALD?
|
- asynchronous longitudinal growth of physis
- ligamentous joint laxity.. not growth abn - defects in endochondral ossification of the cuboidal bones and/or small MC/MT bones - traumatic luxation or fracture of the physis, epiphysis, or carpal/tarsal bones |
|
|
What are some causes of alterations of endochondral ossification?
|
rapid growth
trauma to endochondral ossification centers genetic predisposition nutritional imbalance (energy excess, protein excess or deficiency, calcium:phosphorus excess or deficiency, trace minerals - cu def., zn excess, Manganese def.) |
|
|
Congenital ALD
|
will be present at birth
most correct w/out treatment causes: intrauterine malposition overnutrition of mare joint laxity hypoplasia of cuboidal bones incomplete devt. of MT/MC II and IV if severe >15 degrees or not improving w/in 5-7 days of life, do further dx + intervention |
|
|
three causes of hypoplasia of cuboidal bones
|
premature/dysmature
hypothyroidism osteochondrosis |
|
|
Causes of acquired ALD
|
excessive exercise
excessive weight bearing secondary to contralateral limb lameness over-nutrition improper trimming poor conformation congenital ALD that became worse |
|
|
What questions do you ask during dx or ALD?
|
is a deformity present
has it changed over time define the defotmity (valgus, varus, rotational) what joint(s) involved act now or "wait and see" |
|
|
What do you palpate the limbs for in your physical exam for ALD?
|
heat
pain swelling crepitus |
|
|
Radiographic exam for ALD
|
AP and lateral views (weight bearing)
use long plates if available determine pivot point degree of angulation - measure above angle |
|
|
How do you determine the pivot point for ALD?
|
bisect the long bones above and below joint, and note the area of intersection
|
|
|
Mild ALD = < ____ degrees
severe ALD = > _____ degrees |
Mild ALD = < 5 degrees
Severe ALD = > 15 degrees |
|
|
Radiographic changes seen with ALD
|
metaphysis - flaring and sclerosis
growth plate - indistinct physis, irregular width (convex side) Epiphysis- wedge- shaped +/- flaring Cuboidal bone - abnormal shape, hypoplastic, collapsed, subluxated MT/MC II or IV - shorter or wider joint space bone cortex - diaphyseal remodeling |
|
|
Treatment goals for ALD
|
improve conformation
prevent secondary changes (DJD) improve athletic performance ** the older the foal, the more intervention required and the more severe the angulation, the more intervention required |
|
|
what are the two methods that are popularly used for growth retardation of bone?
|
placement of screws on either side of the physis with a cerclage wire applying tension across the growth plate (ie. the screw and wire)
placing a single screw across one side of the growth plate |
|
|
Angulation within the diaphysis can be treated with....?
|
wedge osteotomy or other sx procedures we didn't talk about
|
|
|
Use ________ extensions to help correct valgus deviations.
|
medial
|
|
|
use __________ extensions to help correct varus deviations.
|
lateral
|
|
|
Use tube casts or splints in cases of ___________ or _____________.
|
severe laxity or hypoplastic cuboidal bones (prevent cuboidal bone fracture)
|
|
|
What is periosteal transection and elevation used for?
|
growth acceleration occurs on the concave side (side it is performed)
perform laterally for valgus deformity ----remove ulnar remnant from distal radial physis ---use periosteal elevator to sepate the periosteum fro the bone and the corners are placed back against the bone to minimize scarring |
|
|
What is transphyseal bridging used for?
|
growth retardation on convex side (side it is performed)
perform medially for valgus deformity --- use two screws with cerclage wire across the physis ----single position screw across one side of the physis -- plating, stapling |
|
|
important things about transphyseal bridging
|
very effective if enough growth can occur
***monitoring of the foal is critical restricted exercise to prevent implant fatigue second sx to remove implants implants can become infected local inflammation and scarring possible bilateral or multiple TPBs may need to be removed at different times overcorrection is possible with this technique ***** |
|
|
what is the prognosis for ALD?
|
the more distal the pivot point, the poorer the px
the older the foal, the longer the implant needs to stay in and the less straightening potential 83% carpal valgus corrected carpal and tarsal bone collapse/crush more guarded MCP/MTP (fetlock) deformities less likely to get corrected b/c short time frame |
|
|
Tendon and ligament laxity
|
primarily congenital but can be acquired
hindlimbs > forelimbs , can be all four etiology: musculotendinous weakness (idiopathic, lack of exercise, systemic illness, bandaging/casting) |
|
|
Clinical signs of tendon and ligament laxity
|
clinical signs - no weight on toe, walks on heel bulbs
|
|
|
Tendon and ligament laxity: Treatment
|
heel extensions
controlled exercise no splinting or bandaging (light bandages only if palmar/plantar fetlock is abraded) |
|
|
Using shoes on foals
|
glue on shoes
limits normal hoof wall growth so do 10 days on, 10 days off second set if needed NO THIRD SET hoof nipper, rasp off (don't pull off) |
|
|
Flexural Deformity (aka contracted tendons)
|
describes physical appearance as well
incorrect term b/c primary lesion is not contracture of the tendinous units primary*** lesion is probably ***length disparity between tendons and bones |
|
|
Flexural Deformity: Px
|
duration of signs inversely related to outcome
if can't straighten manually at surgery ---poor px - carpus px generally poor |
|
|
Possible structures involved in flexural deformity -- need to determine which ones
|
SDFT, DDFT, ulnaris lateralis, joint capsule, combination
|
|
|
Congenital FD
|
developmental
usu. fetlock (metacarpophalangeal) carpus |
|
|
Acquired FD
|
age 4-16 weeks; 1 year
more commonly: fetlock (metacarpophalangeal) coffin joint (distal interphalangeal) |
|
|
FD: pathogenesis -- congenital
|
uterine malpositioning
genetic influences teratogens dz of the mare (influenza) locoweed ingestion by mare sudan grass ingestion by mare (similar to arthrogryposis) |
|
|
FD: pathogenesis -- acquired
|
pain - flexion withdrawl reflex
--physitis --OCD --septic arthritis --wounds --hoof pain --contralateral limb overload Nutritional (high energy, imbalanced rations) |
|
|
characteristics of Distal interphalangeal FD
|
walking on toe
unable to place heel fully on ground "club foot" - upright foot with similar toe and heel hoof wall length excessive toe wear |
|
|
DIP FD staging: stage I
|
dorsal hoof wall angle < 90 degrees
good prognosis |
|
|
DIP FD staging: stage II
|
dorsal hoof wall angle >= 90 degrees
poor prognosis |
|
|
Fetlock contracture involves which tendon/ligament?
|
superficial digital flexor tendon and superior (proximal) check ligament
|
|
|
Distal Interphalangeal Joint Flexural Deformity (coffin joint contracture) involves which tendon/ligament?
|
deep digital flexor tendon and distal check ligament
|
|
|
What are the characteristics of MCP FD?
|
fetlock angle when viewed from the side is upright or knuckled over
DJD may be present in severe cases reducible vs non-reducible flexural deformities slow vs rapid onset |
|
|
Knuckling over indicates that it is a __________ joint problem.
|
Fetlock joint
|
|
|
Carpal FD characteristics
|
buckling at the carpus
severe cases may be recumbent if manual reduction is possible --> good px if manual reduction not possible --> poor prognosis radiographs should be taken ---> incomplete cuboidal bone ossification |
|
|
Congenital FD: Tx
|
assist to nurse
increase exercise NSAIDS and anti-ulcer meds Oxytetracycline (Ca ion chelation, musculotendinous unit relax., results rapid and dramatic) Toe extension shoes (protect toe, stretch tendons) splints/casts if can't stand sx |
|
|
FD treatment: Hoof trimming
|
lower heel to encourage tendon stretch
avoid trimming weakened toe |
|
|
FD: treatment -- Sx
|
usually not required
--- severe carpal flexural deformity may req. ulnaris lateralis + flexor carpi ulnaris transection recumbent cases = grave px |
|
|
__________ commonly occurs in sales yearlings being "pushed" with high energy rations
|
MCP FD
|
|
|
When will you do sx intervention with FD?
|
conservative treatment not effective
severe or rapidly worsening deformities |
|
|
What are the sx interventions for FD?
|
DIP joint - distal check ligament desmotomy
MCP joint- proximal check ligament desmotomy Carpal joint - ulnaris lateralis, flexor carpi ulnaris transection |
|
|
What is the aftercare required for Proximal check ligament desmotomy?
|
pressure bandaging for 3 weeks
NSAIDs for 10-14 days stall rest 10-14 days hand walking beginning at 2 weeks splints req. in most cases |
|
|
What is the aftercare required for Distal check ligament desmotomy?
|
NSAIDs
bandaging 10-14 days (change every 2-3 days) hoof care: lowered heel, toe extension hand walking beginning at 10 days turnout allowed at 3-6 weeks |
|
|
Distal Check Ligament Desmotomy Complications
|
cosmetic blemish
infection (rare; more common in SCL desmotomy) carpal sheath breach unsuccessful procedure |
|
|
Prevention/Minimization of FD
|
discussion w/ owners
good/consistent monitoring proper feeding (avoid overnutrition) pay attention to mare/stallion conformation good and consistent foot trimming watch for lameness in young foals |

