![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
116 Cards in this Set
- Front
- Back
|
a) True or False: Epithelial ovarian cancer (EOC) is the leading cause of gynecologic cancer death in North America
b) What is the lifetime baseline risk of contracting EOC? |
a) True
b) 1.5% |
|
|
a) What percentage of ovarian cancer is EOC?
b) How many have Stage >= II disease? c) What is the average decade of diagnosis? |
a) 85-90%
b) 75% c) 60's |
|
|
a) List histologic types of EOC?
b) What is the most common? |
Serous (most common)
Mucinous Clear cell Endometrioid Brenner Neuroendocrine Sarcomatous |
|
|
List risk factors for EOC.
|
Estrogen
Nulliparity Early menarche Late menopause Infertility Age Hereditary syndrome BRCAI (40%) BRCAII (15-20%) Lynch II (10%) Geographic location (North America) Ethnicity (northern european, jew, icelandic, hungarian) Drugs Menopause HT (estrogen) Family history of ovarian cancer (RR 3.0) PCOS Endometriosis |
|
|
List protective factors against EOC
|
OCP use (RR 0.5)
Breast feeding BSO Tubal ligation |
|
|
a) Should CA125 be used to screen average-risk populations?
b) What percentage of women in the background population with no/benign disease have an elevated CA125? |
a) No.
b) 1% |
|
|
a) What other processes can cause an increase in CA125 level?
b) What is CA125? |
a)
Endometriosis Menstruation PID Fibroids Liver disease b) MUC16 gene product, binds mesothelin |
|
|
a) What percentage of women with early stage EOC have an elevated CA125?
b) Late stage EOC? |
a) 50%
b) 80% |
|
|
In asymptomatic post-menopausal women, does an elevated CA125 (>30U/ml) increase the risk of EOC?
|
Yes.
If CA125 > 30U/ml, RR 35 for EOC w/i one year If CA125 > 100U/ml, RR 200 for EOC w/i one year |
|
|
What percentage of women with invasive ovarian cancer will be BRCA I or II positive?
|
13%
|
|
|
a) What is the recommended screening strategy for ovarian cancer in women at average risk?
b) What is recommended for women on a yearly basis? |
a) None. Nothing has been shown to be effective. No North American expert groups recommend screening.
b) Pelvic exam |
|
|
a) What women are at highest risk of developing ovarian cancer?
b) Discuss screening of these women. |
a)
BRCA I BRCA II Lynch II b) Controversial. Consider risk reduction surgery. Consider OCP. Consider q6-12m CA125 and TVUS. No screening program has been shown to be effective. |
|
|
List the most common symptoms associated with EOC
|
Pelvic/Abdominal pain
Urinary frequency/urgency Early satiety Bloating/increased pant size |
|
|
What is Meigs' syndrome?
|
Pelvic Mass (benign ovarian fibroma)
Ascites Pleural effusion |
|
|
a) What % of ovarian cancers are borderline (LMP)
b) Histologically, what distinguishes borderline ovarian tumours (LMP) from ovarian cancer? c) Histologically, what distinguishes borderline tumours from benign ovarian cysts? |
a) 10-15%
b) no stromal invasion (10% may have areas of microinvasion <3mm, covering <5% of tumour) c) atypia cellular pleomorphism mitotic activity microscopic papilla stratified epithelium |
|
|
List 5 features of physical exam or imaging that might help distinguish a borderline ovarian tumour from EOC?
|
Fixed ovarian mass (exam)
Ascites (CT/US) Omental caking (CT) Mets (CT) Nodal status (PET) |
|
|
After fertility-sparing surgery, what is the risk of recurrence of ovarian LMP in the contralateral ovary?
|
15%
|
|
|
What is the 5 yr survival for ovarian LMP at stage:
I II III IV |
a) 99%
b) 98% c) 96% d) 80% |
|
|
How are patients with ovarian LMP staged?
|
Same as for EOC.
|
|
|
risk factors for developing EOC
|
- nulliparity
- early menarche - late menopause - white race - increasing age - residence in North America and Northern Europe - family history * - personal Hx of breast cancer - ethnic background (European Jewish, Icelandic, Hungarian) |
|
|
factors that reduce risk of EOC
|
- child-bearing (plateaus after 5 births)
- breastfeeding - OCP use (50% decrease) - TL - hysterectomy - BSO (best evidence) - diet low in fat but high in fibre, carotene, and vitamins - HT, perineal talc increase risk |
|
|
% of inherited ovarian cancers BRCA1 and 2 account for
|
- > 90%
|
|
|
indications for BRCA testing
|
- recommended:
- personal Hx of both breast and ovarian cancer - personal Hx of ovarian cancer and a 1st, 2nd, or 3rd degree relative w/ breast cancer at =< age 50 or ovarian cancer at any age - personal Hx of ovarian cancer at any age - personal Hx of breast cancer at =< age 50 and a 1st, 2nd, or 3rd degree relative w/ ovarian or male breast cancer at any age - Ashkenazi Jew and personal Hx of breast cancer at =< age 40 - 1st or 2nd degree relative w/ known BRCA1 or 2 mutation - considered: - personal Hx of breast cancer at =< age 40 - bilateral breast cancer (esp. if first cancer at =< age 50) - breast cancer at =< age 50 and a 1st, 2nd, or 3rd degree relative w/ breast cancer at =< age 50 - Ashkenazi Jew w/ breast cancer at =< age 50 - breast or ovarian cancer at any age and >= 2 1st, 2nd, or 3rd degree relatives w/ breast cancer at any age |
|
|
locations of BRCA1 and 2
|
- BRCA1 on chromosome 17q21
- BRCA2 on chromosome 13q12 |
|
|
risks for developing ovarian cancer w/ BRCA1/2
|
- BRCA1: 39-46%
- BRCA2: 12-20% - cumulative lifetime risk of developing breast cancer w/ BRCA1/2: 65-74% - both genes are autosomal dominant w/ variable penetrance |
|
|
components of screening in women w/ BRCA1/2 mutation that do not wish prophylactic surgery
|
- thorough pelvic examination
- TVU/S - CA125 |
|
|
time to perform BSO in BRCA1/2
|
- upon completion of child-bearing or at age 35
- 90% effective in BRCA1/2 - ~100% effective in HNPCC |
|
|
What is the most reliable indicator of poor prognosis in borderline tumours?
|
- invasive peritoneal implants (as opposed to noninvasive implants)
|
|
|
From what structures in the ovarian stroma are most EOCs found to originate?
|
- cortical inclusion cysts
|
|
|
Common laboratory findings of women w/ EOC
|
- increased CA125
- thrombocytosis (> 400 x 10^9/L) - hyponatremia ~125-130 mEq/L (SIADH) - CA19-9/CEA may be elevated in mucinous |
|
|
conditions that can result in falsely elevated CA125
|
- PID
- endometriosis - leiomyoma - pregnancy - menstruation |
|
|
% of EOC w/ serous histology
|
- > half
- often will contain other cell types as a minor component (< 10%) |
|
|
What are psammoma bodies?
|
- extracellular round laminar dark eosinophilic collections of calcium
- pathognomonic for serous type |
|
|
2nd most common histologic type of EOC after serous
|
- endometrioid adenocarcinomas (15-20%)
- usually better differentiated and slightly better prognosis - 15-20% has coexisting endometrial adenocarcinoma (usually synchronous tumour) - often will have pelvic endometriosis |
|
|
% of EOC that are mucinous
|
- 5-10%
|
|
|
What is pseudomyxoma peritonei?
|
- clinical term used to describe the finding of abundant mucoid or gelatinous material in the pelvis and abdominal cavity, surrounded by thin fibrous capsules
- rarely primary ovarian mucinous carcinoma, usually metastases to ovary - should exclude appendiceal or other GI sites of origin |
|
|
With what benign condition is clear cell adenocarcinoma most frequently associated?
|
- endometriosis
- 5-10% of EOC |
|
|
What are Brenner tumours?
|
- transitional cell tumours
- may be benign or malignant - resemble carcinomas arising from the urinary tract - characterized by having a dense, unusually abundant fibrous stroma w/ embedded nests of transitional epithelium |
|
|
definition of mixed carcinoma
|
- if >10% of an ovarian cancer exhibits a second cell type
- common combinations: mixed clear cell/endometrioid, serous/endometrioid |
|
|
main DDx for primary peritoneal carcinoma
|
- malignant mesothelioma
|
|
|
criteria for diagnosis of PPC when both ovaries present
|
- both ovaries must be normal in size or enlarged by a benign process
- involvement in the extraovarian sites must be greater than the involvement on the surface of either ovary - ovarian tumour involvement must be either non-existent, confined to the ovarian surface epithelium without stromal invasion, or involving the cortical stroma w/ tumor size less than 5x5mm |
|
|
What is the most frequent location of spread for EOC?
|
- omentum
|
|
|
When is it appropriate to follow w/ observation w/ no further Tx after surgery in EOC?
|
- stage IA or IB, grade 1 or 2 EOC (after complete staging procedure)
|
|
|
Are second-look surgeries routinely performed to assess residual disease?
|
- no
- no demonstrable survival benefit |
|
|
overall 5-year survival rate of EOC (all stages)
|
45%
- cf. uterine (84%) and cervical (73%) |
|
|
favourable prognostic factors for EOC
|
- younger age
- good performance status - cell type other than mucinous and clear cell - well-differentiated tumour - smaller disease volume prior to surgical debulking - absence of ascites - smaller residual tumour following primary cytoreductive surgery |
|
|
definition of "platinum-refractory" and "platinum-resistant" EOC
|
- platinum-refractory: progress during primary chemotherapy
- platinum-resistant: relapse w/in 6 months |
|
|
factors that make the best candidate for secondary cytoreductive surgery
|
1. platinum-sensitive disease
2. a prolonged disease-free interval 3. a solitary-site recurrence 4. no ascites |
|
|
What percentage of epithelial ovarian cancers are hereditary?
|
10
|
|
|
Which of the following is not a risk factor for ovarian cancer?
a. Nulliparity b. Late menopause c. Combination oral contraceptive pill use d. Hereditary nonpolyposis colon cancer (HNPCC) |
c. Combination oral contraceptive pill use
|
|
|
Which of the following genetic mutations is associated with the highest risk of developing ovarian cancer?
a. Phosphatase and tensin homolog (PTEN) b. Hereditary Breast Ovarian Cancer Syndrome 1 (BRCA1) c. Hereditary Breast Ovarian Cancer Syndrome 2 (BRCA2) d. MutL homolog 1, colon cancer, nonpolyposis type 2 (MLH1) |
b. Hereditary Breast Ovarian Cancer Syndrome 1 (BRCA1)
|
|
|
A 40-year-old woman with a BRCA1 mutation undergoes a MIS BSO for risk reduction. By what percentage is her breast cancer risk reduced by her BSO?
|
50%
|
|
|
A 55-year-old healthy woman undergoes exploration for a large pelvic mass. Frozen section analysis of her right ovary notes “mucinous low malignant potential, cannot exclude invasion.” There is no other obvious disease. What surgical procedures should be performed, in addition to total abdominal hysterectomy and bilateral salpingo-oophorectomy?
|
Pelvic washings, omentectomy, multiple peritoneal biopsies, bilateral pelvic and para-aortic lymph node dissection, appendectomy (mucinous!)
|
|
|
A 27-year-old nulligravida who desires future fertility underwent a MIS LSO for a 7-cm cyst. The cyst was removed intact, and washings were negative. Final pathology revealed a serous low malignant potential tumor. What is the most appropriate management?
|
Close observation
|
|
|
Which of the following is the worst prognostic feature associated with low malignant potential (LMP) tumors?
a. Advanced stage b. Invasive implants c. Mucinous histology d. Stromal microinvasion |
b. Invasive implants
|
|
|
Which of the following is FALSE regarding ovarian cancer symptoms?
a. Most women with ovarian cancer experience symptoms 20 to 30 days per month. b. Women with ovarian cancer do not have symptoms until the disease is very advanced. c. The most frequent symptoms associated with ovarian cancer include urinary urgency, pelvic pain, and bloating. d. None of the above |
b. Women with ovarian cancer do not have symptoms until the disease is very advanced.
|
|
|
What percentage of patients with stage I ovarian cancer have a normal cancer antigen 125 (CA125) level?
|
50%
|
|
|
Which of the following conditions can create an elevated CA125 level?
a. Leiomyomas b. Endometriosis c. Congestive heart failure d. All of the above |
d. All of the above
|
|
|
Which of the following radiologic tests is most helpful in a patient with suspected advanced ovarian cancer?
a. Transvaginal ultrasound b. Positron emission tomography (PET) scan c. Magnetic resonance (MR) imaging of the pelvis d. Computed tomography (CT) scan of the abdomen and pelvis |
d. Computed tomography (CT) scan of the abdomen and pelvis
|
|
|
Which one of the following women does not need referral to a gynecologic oncologist?
a. A 35-year-old with a complex 7-cm adnexal mass and a CA125 level of 75 b. A 60-year-old with a complex 7-cm adnexal mass and a CA125 level of 75 c. A 35-year-old with a complex 7-cm adnexal mass, ascites, and a CA125 level of 75 d. A 50-year-old with a complex 7-cm fixed adnexal mass and a CA125 level of 25 |
a. A 35-year-old with a complex 7-cm adnexal mass and a CA125 level of 75
|
|
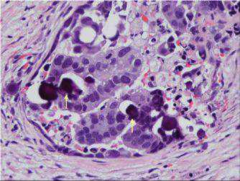
In the photomicrograph below, to what structures are the white arrows pointing? (Hint—this finding is pathognomonic for the most common histologic cell type of epithelial ovarian cancer.)
a. Signet rings b. Hobnail cells c. Keratin pearls d. Psammoma bodies |
d. Psammoma bodies
|
|
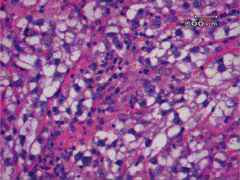
Shown here, what is the most common cell type of epithelial ovarian cancer associated with endometriosis?
a. Mucinous b. Clear cell c. Endometrioid d. Papillary serous |
b. Clear cell
|
|
|
A 27-year-old presents to the emergency department with a complaint of increasing abdominal distension, constipation, and weight loss. A CT scan reveals a 10-cm right adnexal mass and retroperitoneal lymphadenopathy. Her serum CA125 level is 45, β-hCG is less than 5, and AFP and LDH levels are normal. Her serum calcium level is 15. What is the most likely diagnosis?
a. Lymphoma b. Small cell ovarian cancer c. Primary hyperparathyroidism d. Malignant germ cell tumor of the ovary with bone metastasis |
b. Small cell ovarian cancer
|
|
|
Which of the following is NOT a characteristic of Krukenberg tumors?
a. They are bilateral. b. They usually arise from primary gastric tumors. c. They are usually the only site of metastatic disease. d. They are comprised of mucinous and signet ring cells. |
c. They are usually the only site of metastatic disease.
|
|
|
What is the most common method of ovarian cancer spread?
a. Lymphatic b. Hematogenous c. Direct extension d. Tumor exfoliation |
d. Tumor exfoliation
|
|
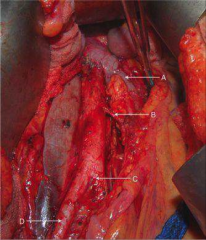
Which of the following correctly indicates the cephalad border of the para-aortic lymph node dissection for ovarian cancer clinically confined to the ovary?
|
A
|
|
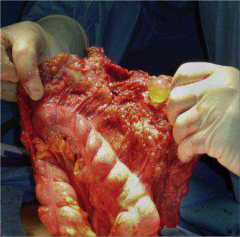
A 40-year-old woman with a right-sided pleural effusion undergoes exploratory laparotomy for a pelvic mass and elevated CA125 level.
Cytologic analysis of the pleural fluid reveals no malignant cells. Upon exploration, the finding below is seen. Which FIGO stage is she? |
IIIC
|
|
|
What percentage of women with ovarian cancer clinically confined to the ovaries will be upstaged by surgery?
|
33%
|
|
|
Which of the following patients does not need adjuvant chemotherapy following surgery for epithelial ovarian cancer?
a. A 65-year-old following TAH BSO, omentectomy, multiple peritoneal biopsies, and pelvic and para-aortic lymph node dissection for a stage IC clear cell ovarian cancer. b. A 45-year-old following TAH BSO, omentectomy, multiple peritoneal biopsies, and pelvic lymph node dissection for a stage IA grade 1 endometrioid adenocarcinoma of the ovary. c. A 55-year-old followingTAH BSO, omentectomy, multiple peritoneal biopsies, and pelvic and para-aortic lymph node dissection for a stage IB grade 1 papillary serous carcinoma of the ovary. d. A 70-year-old following TAH BSO, omentectomy, multiple peritoneal biopsies, and pelvic and para-aortic lymph node dissection for a stage IC grade 1 papillary serous carcinoma of the ovary. |
c. A 55-year-old followingTAH BSO, omentectomy, multiple peritoneal biopsies, and pelvic and para-aortic lymph node dissection for a stage IB grade 1 papillary serous carcinoma of the ovary.
|
|
|
What is the goal of cytoreductive surgery for advanced ovarian cancer?
a. Remove all tumors larger than 1 cm b. Remove all tumors larger than 2 cm c. Remove all tumors larger than 0.5 cm d. Remove all gross disease |
d. Remove all gross disease
|
|
|
Which of the following chemotherapy regimens is associated with the longest overall survival for women with optimally debulked (less than 1 cm residual disease) stage III epithelial ovarian cancer?
a. Single agent carboplatin b. Intravenous (IV) carboplatin and paclitaxel c. Intraperitoneal (IP) cisplatin and paclitaxel d. Intravenous (IV) carboplatin, paclitaxel, and bevacizumab |
c. Intraperitoneal (IP) cisplatin and paclitaxel
|
|
|
A woman with a history of stage IIIC ovarian cancer who underwent optimal cytoreductive surgery followed by six cycles of intraperitoneal (IP) cisplatin and paclitaxel recurs 4 months after completion of chemotherapy. She complains of bloating and decreased appetite. Which of the following is the most appropriate treatment?
a. Tamoxifen b. Intravenous (IV) carboplatin c. IV carboplatin and paclitaxel d. Pegylated liposomal doxorubicin |
d. Pegylated liposomal doxorubicin
|
|
|
Which of the following chemotherapy regimens is appropriate treatment of a patient with recurrent platinum-sensitive ovarian cancer?
a. Carboplatin with paclitaxel b. Carboplatin with gemcitabine c. Carboplatin with pegylated liposomal doxorubicin d. All of the above |
d. All of the above
|
|
|
3 kinds of cystic ovarian tumors
|
functional
neoplastic endometrioma |
|
|
T/F: functional cysts can be malignant
T/F: neoplastic cysts can be malignant T/F: endometriosis cysts can be malignant T/F: solid tumors cysts can be malignant |
F
T F T |
|
|
3 kinds of functional ovarian cysts
|
follicular
corpus luteum theca lutein |
|
|
functional cysts are common/rare
they are related to ___ |
common
ovulation |
|
|
follicular cysts are lined by ___ cells
|
granulosa
|
|
|
usual follicular cyst outcome
|
spontaneous resolution within 2 weeks
|
|
|
___ is one kind of corpus luteum cyst
|
hemorrhagic corpus luteum
|
|
|
menstrual abnormality associated with corpus luteum cyst
this can cause confusion with ___ |
delay of menses
ectopic pregnancy |
|
|
usual outcome of corpus luteum cyst in the absence of pregnancy
usual outcome of corpus luteum cyst in the presence of pregnancy |
resolution within 8 weeks
resolution at development of yolk sac |
|
|
corpus luteum cysts present with ___
they are more common on L/R |
sudden pain
R |
|
|
compared with follicular cysts, CL cysts are ___
|
more likely to cause pain
larger |
|
|
theca lutein cysts and ___ are caused by ___, e.g. from ___ (2)
|
luteoma of preganancy
hCG molar pregnancy chorioca |
|
|
___ is a benign germ cell tumor
|
dermoid cyst
|
|
|
dermoid cysts are aka ___
|
benign cystic teratoma
|
|
|
3 benign epithelial tumors
|
serous cystadenoma
mucinous cystadenoma brenner tumor |
|
|
benign tumor of sex cord stroma
|
fibroma
|
|
|
serous/mucinous cystadenoma is more common
serous/mucinous cystadenoma is bigger serous/mucinous cystadenoma is associated with psammoma bodies |
serous
mucinous serous |
|
|
___ is a complication of mucinous cystadenoma
|
pseudomyxoma peritonei
|
|
|
u/s parameters distinguishing benign from malignant ovarian tumors
|
size
laterality (bilateral worse) structure (septated, complex) ascites vascualrity solid/cystic components |
|
|
benign tumors are usually uni/bilateral
|
uni
|
|
|
structure of benign tumors (3)
|
cystic
unilocular thin septations |
|
|
structure of malignant tumors (3)
|
solid elements present
multilocular thick septations |
|
|
7 indications for surgery on ovarian cyst
|
>5 cm and lasting>6 w
>10 cm solid lesion papillary vegetation present ascites palpable and present in premenarchal/postmenopausal torsion/rupture suspected |
|
|
5 protective factors for ovarian ca
|
OCP use
multiparity breastfeeding tubal ligation hysterectomy |
|
|
tx for stage 1a or 1b epithelial ovarian ca (5)
|
TAH
BSO omentectomy peritoneal washings LN dissection |
|
|
tx for stage 2/3/4 epithelial ovarian ca
|
debulking surgery
chemo |
|
|
chemo for advanced epithelial ovarian ca (2)
|
carboplatin
taxol |
|
|
primordial germ cells become ___ (2 tumors)
|
dysgerminoma
embryonal ca |
|
|
markers for dysgerminoma
|
LDH
|
|
|
markers for embryonal ca
embryonal cells become ___ (2) cells |
AFP
hCG embryonic extraembryonic |
|
|
embryonic cells give rise to ___ tumors
|
immature teratoma
|
|
|
marker for immature teratoma
|
nothing!
|
|
|
2 cell types with extraembryonic differentiation
|
trophoblast
yolk sac |
|
|
trophoblast cells give rise to ___
|
choriocarcinoma
|
|
|
marker for choriocarcinoma
|
hCG
|
|
|
marker for yolk sac tumor
|
AFP
|
|
|
in contrast to epithelial tumors, germ cell tumors ___ (2)
|
grow quickly
present early |
|
|
surgical tx for malignant germ cell tumors:
if bilateral disease, ___ if unilateral disease, ___ |
TAH + BSO
unilateral SO |
|
|
in addition to surgery, give ___ for malignant germ cell tumor
|
BEP chemo
|
|
|
BEP means ___
|
bleomycin
etoposide cisplatin |
|
|
tx for sex cord stromal tumors
|
USO
|
|
|
Prognostic factors for EOC
|
Younger age
Good performance status Cell type other than mucinous and clear cell Well-differentiated tumor Smaller disease volume prior to surgical debulking Absence of ascites Smaller residual tumor following primary cytoreductive surgery |
|
|
the best candidates for secondary cytoreductive surgery have?
|
(1) platinum-sensitive disease,
(2) a prolonged disease-free interval, (3) a solitary-site recurrence, and (4) no ascites |

