![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
56 Cards in this Set
- Front
- Back
|
Def: Gastroenteritis
- most common cause? - symptoms? |
inflammation of the lining of the intestines caused by a virus, bacteria, or parasites
most common cause is Norovirus infection symptoms include: diarrhea, abdominal pain, vomiting, headache, fever, & chills |
|
|
Def: Gastritis
Causes? |
inflammation, irritation, or erosion of the lining of the stomach
causes: excessive alcohol use, chronic vomiting, stress, certain medications, H. pylori, pernicious anemia, bile reflux, infection |
|
|
Def: Enteritis
causes? |
inflammation of the small intestine
causes: usually bacteria or virus sometimes by autoimmune (i,e, Crohn's), certain drugs, radiation damage |
|
|
Def: Colitis
Causes? |
inflammation of the large intestine
causes: infections, inflammatory disorders (colitis, Crohn's), ischemia, radiation |
|
|
Def: Cholecystitis
Causes? |
inflammation of the gall bladder
causes: gallstones, infection, injury |
|
|
Def: Dysentery
|
diarrhea with pus and blood in the feces
causes: microbial deep invasion and/or cytotoxin destruction of colon |
|
|
Def: Enteric fever
|
a systemic infection starting in the GI tract
e.g. typhoid - an infection that causes diarrhea and rash - usually caused by Salmonella typhi |
|
|
Def: tenesmus
|
feeling of incomplete defecation
|
|
|
Def: enterotoxin
|
a harmful substance produced by certain bacteria that damages the GI tract causing cramps, N&V, diarrhea
|
|
|
Def: cytotoxin
|
a substance that is toxic to cells
|
|
|
Def: exotoxin
|
a toxin secreted by bacteria
|
|
|
Def: Intoxication
|
poisoning by a drug or toxic substance
|
|
|
Def: Oral rehydration therapy
|
the use of modest amounts of sugar and salt added to water to prevent or treat dehydration
|
|
|
Def: Bile
|
fluid made by the liver, stored in gall bladder that aids in digestion of lipids
|
|
|
Following the GI tract from the mouth to the anus, what rough density of microbes
(sparse, heavy, etc.) do you find in each site? |

|
|
|
What are the host defenses of the GI tract?
|
1. Epithelium, mucus secretions
2. Peristalsis 3. Stomach acid 4. Bile 5. Secretory IgA, IgG 6. Phagocytes 7. GALT - gut associated lymphoid tissue 8. Normal flora |
|
|
What are the four class examples of obligate human pathogens?
|
1. Salmonella typhi
2. Shigella 3. Helicobacter pylori 4. Entamoea histolytica |
|
|
What are the three zoonotic pathogens presented in class?
What is the unexpected source? |
1. E. coli
2. non-typhoid salmonella 3. Campylobacter Humans can be the source of infection, via fecal/oral transmission |
|
|
What is the relationship between acid tolerance of a microbe and minimum inoculum required for infection?
What is the result of reduced gastric acidity? |
inversely proportional
high acid tolerance = low infectious inoculum (most inoculum make it through the stomach) low acid tolerance = high infectious inoculum (small % make it through the stomach) Reduced gastric acidity increases susceptibility to GI pathogens |
|
|
What is the typical site, clinical features, and examples for infection via INTOXICATION mechanism?
|
site: small intestine
cf: severe N&V and/or diarrhea ex: Staphylococcus aureus, Bacillus cereus |
|
|
What is the typical site, clinical features, and examples for infection via SECRETORY TOXIN mechanism?
|
site: small bowel
cf: profuse watery diarrhea, possibly pain &/or fever ex: ETEC, Vibrio cholerae, rotavirus |
|
|
What is the typical site, clinical features, and examples for infection via CYTOTOXIN mechanism?
|
site: large bowel
cf: bloody diarrhea, painful cramps, fever ex: EHEC, Shigella |
|
|
What is the typical site, clinical features, and examples for infection via MUCOSAL COLONIZATION & DESTRUCTION mechanism?
|
site: small bowel
cf: diarrhea, fever, N&V ex: EPEC, Salmonella, Campylobacter (early), rotavirus |
|
|
What is the typical site, clinical features, and examples for infection via DEEP INVASION mechanism?
|
site: large bowel
cf: purulent bloody dysentery, painful cramps, fever ex: EIEC, Shigella, Campylobacter (late), Entamoeba histolytica |
|
|
What is the typical site, clinical features, and examples for infection via SYSTEMIC DISSEMINATION mechanism?
|
site: GI to blood to liver to GI
cf: systemic signs and symptoms (enteric fever) ex: Salmonella typhi |
|
|
How does Staphylococcus manifest as food poisoning?
|
enterotoxins stimulate T lymphocytes in the gut
- a common skin microbiota, contamination is common in many foods, but not all strains are toxigenic |
|
|
How does Bacillus cereus manifest as food poisoning?
|
2 types of toxins:
Emetic toxin pre-formed in food causes vomiting 1-6 hr pc Diarrhetic toxin formed in intestinal lumen causes diarrhea 8-16 hr pc - a strain may produce one or both types, or neither |
|
|
What are the four most common causes of bacterial enteric disease in the US?
|
1. Campylobacter
2. Salmonella 3. Shigella 4. E. coli |
|
|
Does Heliobacter cause enteritis?
|
NO, it causes gastritis
|
|
|
ETEC
|
Enterotoxigenic E. coli
"traveler's diarrhea" secretory toxin |
|
|
EPEC
|
enteropathogenic E. coli
"infantile diarrhea" mucosal colonization and destruction similar to non-typhoid Salmonella |
|
|
EIEC
|
Enteroinvasive E. coli
bacillary dysentery - deep invasion similar to Shigella |
|
|
EHEC
|
enterohemorrhagic E. coli
hemorrhagic colitis, HUS cytotoxin - zoonosis from cow intestines or infected humans |
|
|
HUS - Hemolytic uremia syndrome
cause? associated with what pathogens? clinical features Who at risk? |
caused by cytotoxin
associated with EHEC, some Shigella strains, other enteropathogens cf: thrombotic microangiopathy hemolytic anemia throbocytopenia w/ renal lesions renal failure Children & elderly are at increased risk of this rare disease |
|
|
How does Salmonella manifest as Gastroenteritis?
|
from mucosal colonization and destruction (EPEC)
- non-typhoid Salmonella - "rotton egg" odor of stool - relative resistance to bile salts |
|
|
how does Salmonella manifest as Enteric Fever?
|
from systemic dissemination
- mainly S. typhi - blood culture likely before stool - reservoir sites (gall bladder) lead to carrier state |
|
|
What are the four causes of Enteric fever presented in class?
|
1. Salmonella typhi
2. other Salmonella species 3. Yersinia enterocolitica 4. Campylobacter jejuni Note: colonization of gallbladder can lead to continuous fecal shedding by asymptomatic carrier |
|
|
What is the timing of positive fecal, blood, and urine cultures for Typhoid?
|

|
|
|
Shigella
|
obligate human pathogen; fecal/oral
small inoculum required Can cause Bacillary dysentery via deep invasion Some strains make cytotoxin |
|
|
Campylobacter
|
most common bacterial enteric infection in US
fecal/oral, contaminated food & animals gastroenteritis from mucosal colonization and destruction rare enteric fever from systemic dissemination |
|
|
Yersinia
|
fecal/oral, animal transmission
gastroenteritis, diarrhea, occasional pseudoappendicitis |
|
|
Y. pestis
|
human-human transmission via fleas or respiratory droplets
plague: bubonic, pneumonic, septicemic |
|
|
Vibrio cholerae
|
fecal/oral
large inoculum required Cholera, voluminous watery diarrhea |
|
|
Vibrio parahemolyticus
|
salt water, shellfish, sushi
gastroenteritis, rare enteric fever |
|
|
Vibrio vulnificus
|
salt water, shellfish, skin abrasions
wound infection, septicemia NOT gastroenteritis - especially in immunocompromised & alcoholics |
|
|
Listeria monocytogenes
|
dairy & meat, direct animal contact, transplacental, perinatal
gram + rod; resistant to freezing, drying, heat gastroenterits |
|
|
What are the symptoms of viral gastroenteritis?
|
- watery diarrhea, N&V
- viral shedding for weeks after symptoms end - prolonged full recovery time |
|
|
Rotavirus
|
major viral agent in infants & young children
- vaccine since 2006 reducing prevelance gastroenteritis via secretory toxin, mucosal colonization & destruction diagnosed by stool ELISA |
|
|
Norovirus
|
very contagious; outbreaks
gastroenteritis |
|
|
What condition do Adenovirus and astrovirus cause?
|
gastroenteritis
|
|
|
What are the three parasitic agents of enteric infection discussed in class?
|
Entamoeba histolytica
Giardia lamblia Cryptosporidium parvum |
|
|
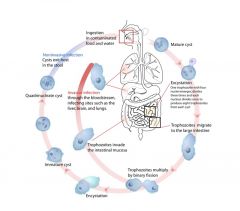
What is the process of Entamoeba histolytica infection?
|
|
|
|
Helicobacter pylori
|
fecal/oral transmission
ulcers, gastitis, development of cancer - microbe avoids/survives acid environment |
|
|
What medications can be used to treat enteric infections?
|
1. maintain hydration and electrolytes
2. bismuth subsalicylate may have some antimicrobial activity 3. GI motility reducing agents (do NOT use if blood or pus in stool) 4. probiotic therapy - antibiotics often not indicated |
|
|
Why are antibiotics generally not indicated for enteric infecions?
|
1. infection is often self-limiting
2. duration of infection < time to achieve therapeutic antibiotic level 3. vomiting & diarrhea expel oral antibiotics 4. antibiotics may worsen situation by altering normal microbiota 5. no effective antibiotics for viral agents |
|
|
What are the special cases when antibiotics might be used to treat enteric infections?
|
1. at-risk patients
2. protracted and/or severe infections - often fluoroquinolones (ciprofloxacin) for bacteria; metronidazole for Entamoeba |

