![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
94 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
The posterior pituitary glands stores hormones produced by what?
|
The posterior pituitary glands stores hormones produced by what?
- Hypothalamus |
|
|
|
What glands are part of the endocrine system?
|
What glands are part of the endocrine system?
- pituitary gland - parathyroid gland - adrenal gland - thyroid gland - thymus gland - pancreas |
|
|
|
What does the blood stream have to do with target tissues and transport of the endocrine hormones?
|
What does the blood stream have to do with target tissues and transport of the endocrine hormones?
- they transport the hormone to the target tissues |
|
|
|
When releasing hormones, it is done by the...what?
|
When releasing hormones, it is done by the Anterior Pituitary Gland
|
|
|
|
The pituitary hormone ACTH acts on the adrenals, True or False?
|
The pituitary hormone ACTH acts on the adrenals, True or False?
- True |
|
|
|
What are adrenals?
|
What are adrenals?
-Small gland atop the kidneys, two parts: (inner) medulla and (outer) cortex -The medulla produces epinephrine (adrenaline) and norepinephrine (the flight or fight hormones (catecholamines)) -The cortex produces: mineralocorticoids (aldosterone), glucocorticoids (cortisol or hydrocortisone), and small amounts of androgens and estrogens |
|
|
|
What does ACTH stand for?
|
What does ACTH stand for?
-Adrenocorticotropic Hormone (ACTH) -ACTH (adreno corticotropic hormone) |
|
|
|
Prolactin, thyrotropin, and somatotropin are produced and secreted by what gland?
|
Prolactin, Thyrotropin, and Somatotropin are produced and secreted by what gland?
- Anterior Pituitary Gland |
|
|
|
True or False: The pancreas somatotropin hormone inhibits pancreatic secretion of glucagon and insulin?
|
True or False: The pancreas somatotropin hormone inhibits pancreatic secretion of glucagon and insulin?
- True |
|
|
|
Ovaries, testis, pancreas and thyroid glands are endocrine tissues that are affected by aging and reduce their weight?
|
Ovaries, testis, pancreas and thyroid glands are endocrine tissues that are affected by aging and reduce their weight?
-Tissues are getting old, overdone, everything slows down (but still are working) |
|
|
|
Abnormal anterior pituitary gland result in what disorders?
|
Abnormal anterior pituitary gland result in what disorders?
- Pituitary Dwarfism - Achondroplasia Dwarfism - Turner Syndrome - Primordial Dwarfism - Gigantism (marcosomia) - Acromegaly - Hyperpituitarism - Hypopituitarism |
|
|
|
What does pt with acromeglia look like?
|
What does pt with acromeglia look like?
- enlargement of hands, nose, mandible, feet, ears, supraorbital ridge - thickening of the tongue (dysphagia) - spade shaped hands |
|
|
|
what does GH stand for?
|
what does GH stand for?
- Growth Hormone |
|
|
|
Q1. Is acromegalia and gigantism a result of over produced growth hormone?
Q2. What is the difference between Acromeglia and Gigantism? |
Q1. Is acromegalia and gigantism a result of over produced growth hormone?
- yes Q2. What is the difference between Acromeglia and Gigantism? - gigantism happens in childhood and acromegalia happens in adulthood |
|
|
|
If pt doesn’t like fish, which helps maintain the endocrine system, what can they add to their diet instead?
|
If pt doesn’t like fish, which helps maintain the endocrine system, what can they add to their diet instead?
- Iodized salt (iodine is in fish and in the salt) |
|
|
|
What labs would be elevated as a result of overproduction of Growth Hormone?
|
What labs would be elevated as a result of overproduction of Growth Hormone?
- Glucose (Hyperglycemia) |
|
|
|
What is norm specific gravity?
|
What is norm specific gravity?
1.001-1.03 (up to 5) |
|
|
|
What does Hypophysectomy mean?
|
What does Hypophysectomy mean?
- surgical removal of the hypophysis (pituitary gland) - Transphenoidal (through the nose) hypophysectomy is the most commonly used surgical approach - most common treatment for hyperpituitarism |
|
|
|
What do you monitor after having a Hypophysectomy?
|
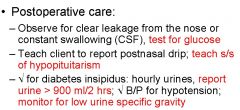
What do you monitor after having a Hypophysectomy?
|
- “Observe for clear leakage from the nose or constant swallowing (CSF), TEST for GLUCOSE”
(Cerebral Spinal Fluid (CSF) |
|
|
If your post op pt (who just had a hypophysectomy), has a specific gravity of less than 1.001 what are you going to do and why?
|
If your post op pt (who just had a hypophysectomy), has a specific gravity of less than 1.001 what are you going to do and why?
- Diabetes Insipidus - “check for diabetes insipidus: hourly urines, report urine >900 ml/2 hours; check B/P for hypotension; monitor for low urine specific gravity”. - “check for diabetes insipidus: specific gravity <1.004; hormone replacement with vasopressin (ADH) may be needed to maintain fluid balance”. |
|
|
|
What is Diabetes Insipidus?
|
What is Diabetes Insipidus?
- “Diabetes Insipidus is characterized by excessive fluid intake and hypotonic (low specific gravity) polyuria”. - Diabetes insipidus (DI) is a condition characterized by excessive thirst and excretion of large amounts of severely diluted urine, with reduction of fluid intake having no effect on the latter. - pt will pee as fast as they drink water - Trauma to the pituitary gland (if you just had a Hypophysectomy) |
|
|
|
What are the classic symptoms of Diabetes Insipidus?
|
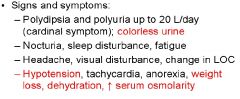
What are the classic symptoms of Diabetes Insipidus?
- Polyuria; Output is greater than intake - Polydipsia and polyuria up to 20 L/day (cardinal symptom); colorless urine - Nocturia, sleep disturbance, fatigue - Headache, visual disturbance, change in LOC - Hypotension, tachycardia, anorexia, weight loss, dehydration, increased serum osmolarity (the amount of chemicals dissolved in the liquid part (serum) of the blood). |
|
|
|
What does ADH mean?
|
What does ADH mean?
- antidiuretic hormone (aka vasopressin) |
|
|
|
Kidney are the target for vasopressin (ADH)? T or F
|
Kidney are the target for vasopressin (ADH)? T or F
True (it is squeezing it out) |
|
|
|
What are vasopressors?
|
What are vasopressors?
- ADH - causing constriction of blood vessels. - An agent that causes a rise in blood pressure. |
|
|
|
What does Diabetes Insipidus have to do with Hypophysectomy?
|
What does Diabetes Insipidus have to do with Hypophysectomy?
- removal of the pituitary gland, it has to do with the trauma - Diabetes insipidus can be primary or secondary (hypophysectomy, tumor, head injury) |
|
|
|
pts need to be taught if after a Hypophysectomy, if they should develop Hypopituitarism, what do they need to do?
|
pts need to be taught if after a Hypophysectomy, if they should develop Hypopituitarism, what do they need to do?
- go to the DR. (see a Endocrinologist) (check for diabetes insipidus) |
|
|
|
Kidney’s are the target for what?
|
Kidney’s are the target for what?
- vasopressin |
|
|
|
Diabetes Insipidus can be a result of a malfunctioning, what?
|
Diabetes Insipidus can be a result of a malfunctioning, what?
- Posterior pituitary or a head trama - Monitor for Low Specific Gravity which will tell you the ADH levels - Monitor for ADH deficiency (ADH is low in Diabetes Insipidus) - Inappropriate amount of ADH |
|
|
|
Secretion of ADH causes tubular reabsorption of what to increase?
|
Secretion of ADH causes tubular reabsorption of what to increase?
- Increase Sodium to increase water |
|
|
|
What is ADH ?
|
What is ADH = anti diuretic hormone
|
|
|
|
What sign is most indicative of Diabetes Insipidus?
|
What sign is most indicative of Diabetes Insipidus?
- Low urine specific gravity |
|
|
|
what would the urine look like for a pt with inadequate vasopressin (ADH) secretion due to Diabetes Insipidus?
|
what would the urine look like for a pt with inadequate vasopressin (ADH) secretion due to Diabetes Insipidus?
- Clear (will have NO waist products) (this is bad) |
|
|
|
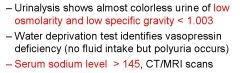
What does SIADH stand for?
|
What does SIADH stand for?
Syndrome of Inappropriate Antidiuretic Hormone (SIADH) |
|
|
|
What are the classic s/s of SIADH? (Syndrome of Inappropriate Antidiuretic Hormone)
|
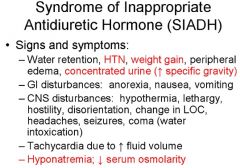
What are the classic s/s of SIADH? (Syndrome of Inappropriate Antidiuretic Hormone)
- water retention (peripheral edema) - hyponatremia - weight gain - concentrated Urine (increased Specific Gravity) - HTN - Tachycardia - decreased serum osmolarity |
|
|
|
What does metastatic breast cancer have to do with SIADH?
|
What does metastatic breast cancer have to do with SIADH?
- It’s a risk factor - Breast Cancer metastasizes to the brain (where the posterior pituitary (secretes ADH) gland is located). - Risk factors: Metastatic Malignancies, Brain Tumors. |
|
|
|
What is the drug of choice for SIADH?
|
What is the drug of choice for SIADH?
- lithium (it is a salt; sodium) (excreted as a salt) |
|
|
|
what lab would you expect to see decreased in SIADH?
|
what lab would you expect to see decreased in SIADH?
- Hyponatremia; Decreased Serum Osmolarity |
|
|
|
Thyroid hormone production depends on sufficient iodine intake, True or False?
|
Thyroid hormone production depends on sufficient iodine intake, True or False?
- True |
|
|
|
What type of IV fluid would a SIADH pt receive and why?
|
What type of IV fluid would a SIADH pt receive and why?
- Hypertonic Saline (2-3%) |
|
|
|
Why is restriction of fluid a nursing priority in pt with SIADH?
|
Why is restriction of fluid a nursing priority in pt with SIADH?
- Because u want to preserve sodium and all the other electrolytes that you will be peeing out - “Strict fluid restriction because further fluid intake dilutes plasma sodium levels.” |
|
|
|
An increased thyroid hormone and enlarged thyroid indicates which disorder?
|
An increased thyroid hormone and enlarged thyroid indicates which disorder?
- hyperthyroidism (thyrotoxicosis) |
|
|
|
What is a thyroid storm?
|
Q1. What is a thyroid storm?
- A surge of thyroid hormones - “Also known as thyrotoxic crisis, thyroid storm results from a sudden surge of large amounts of thyroid hormones into the bloodstream, causing greater increase in body metabolism.” |
|
|
|
What are the classic symptoms of a thyroid storm?
|
Q2. What are the classic symptoms of a thyroid storm?
- Hyperthermia (up to 106 degrees F) - Hypertension - Tachydysrhythmias - Hyperglycemia - Delirium - Vomiting - Abdominal Pain |
|
|
|
What is another name for “eyes protruding out of my head” in graves disease?
|
What is another name for “eyes protruding out of my head” in graves disease?
- Exophthalmos (also called exophthalmia or proptosis) is a bulging of the eye anteriorly out of the orbit. - Hyperthyroidism is the condition - Exophthalmos (bulging eyes, characteristic, but absent in many clients with hyperthyroidism) |
|
|
|
What can u do to keep protruding eyes from drying out (especially at night)?
|
What can u do to keep protruding eyes from drying out (especially at night)?
- Lubricant, non allergenic tape - Provide eye protection: patches, lubricant, taping eyelids closed |
|
|
|
What is Graves’ Disease?
|
What is Graves’ Disease?
- The most common form of hyperthyroidism, an autoimmune disorder that increases T4 production, enlarges the thyroid gland, and causes multiple system changes. |
|
|
|
Why do u monitor cardiac status on pt who have Graves’ disease (Hyperthyroidism) with a temp over 103?
|
Why do u monitor cardiac status on pt who have Graves’ disease (Hyperthyroidism) with a temp over 103?
- monitor cardiac status because the pt is burning up (Tachycardia, HTN, Palpitations, Heat Intolerance) |
|
|
|
What S/S would you expect to find in a pt who has hyperthyroidism?
|
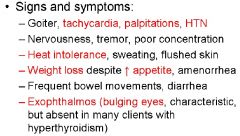
What S/S would you expect to find in a pt who has hyperthyroidism?
- Tachycardia - Goiters - Palpitations - HTN - Heat Intolerance - Frequent Bowel Movements - Bulging eyes (Exophthalmos - Hot, sweating, flushed skin - Increased Appetite - Weight Loss - Nervousness, Tremor, Poor Concentration |
|
|
|
What is Myxedema?
|
*What is Myxedema?
- Hypothyroidism (Myxedema) - not producing T3 or T4 (Increased Thyroid Stimulating Hormone (TSH)) - A life threatening condition that occurs when hypothyroidism is untreated or when a stressor such as infection affects an individual with hypothyroidism. |
|
|
|
What are the S/S of hypothyroidism?
|
What are the S/S of hypothyroidism?
- weight gain - sensitivity to cold - constipation - cold, dry, flaky, and coarse skin - puffy hands, face, and feet - weakness, fatigue, forgetfulness - Decreased mental stability - Periorbital (Head) edema - Bradycardia, decreased heart output (the lights are on, but nobody is home) |
- weight gain
- sensitivity to cold - constipation - cold, dry, flaky, and coarse skin - puffy hands, face, and feet - weakness, fatigue, forgetfulness - Decreased mental stability - Periorbital (Head) edema - Bradycardia, decreased heart output (the lights are on, but nobody is home) |
|
|
What environmental changes may a pt make in the home to make it confortable if they have hypothyroidism?
|
What environmental changes may a pt make in the home to make it confortable if they have hypothyroidism?
Increase the heat – increase the thermostat (Turn on the AC if the pt is hyperthyroidism) |
|
|
|
What lab test would indicate primary hypothyroidism?
|
What lab test would indicate primary hypothyroidism?
- TSH-up - T3-down - T4-down (hyperthyroidism would be the opposite) |
|
|
|
What is thyroidectomy?
|
What is thyroidectomy?
- Removal of the thyroid |
|
|
|
What is a possible complication of a thyroidectomy that would cause tingling around mouth and muscles twitching?
|
What is a possible complication of a thyroidectomy that would cause tingling around mouth and muscles twitching?
- Lacking in Calcium. Hypocalcemia. - Possible parathyroid gland injury (hypocalcemia and tetany) |
|
|
|
What keep at bedside of a post op pt that just had a thyroidectomy?
|
What keep at bedside of a post op pt that just had a thyroidectomy?
- emergency tracheostomy - 1-3 Liters of O2 - Keep a crash cart with Calcium Gluconate. - Calcium gluconate or calcium chloride for IV use should be available; tracheostomy kit |
|
|
|
Why are we monitoring a pt respiratory status post op thyroidectomy?
|
Why are we monitoring a pt respiratory status post op thyroidectomy?
- ABC and safety - Surgery on the neck - Can result from swelling, tetany, or damage to the laryngeal nerve, causing spasms |
|
|
|
What is possibility of accidentally damaging or removing the parathyroid during thyroidectomy?
|
What is possibility of accidentally damaging or removing the parathyroid during thyroidectomy?
- Possibility is high because parathyroid glands are small, next to one another, and attached to the thyroid gland. |
|
|
|
Due to accidently removing the parathyroid, what would you monitor the pt for?
|
Due to accidently removing the parathyroid, what would you monitor the pt for?
- Tetany (Trousseau (fingers) and Chvostek (cheeks)) (fingers cramp up because calcium is missing) Muscles will not contract without calcium (calcium flushes nerves so muscles can contract) - Ask client hourly about tingling around the mouth, toes, or fingers; assess for muscle twitching; assess Trousseau and Chvostek |
|
|
|
What is the S/S of tetany?
|
What is the S/S of tetany?
- continuous muscle twitching |
|
|
|
Which hormone responds to low blood calcium levels by increasing the breakdown of bone and reabsorption?
|
Which hormone responds to low blood calcium levels by increasing the breakdown of bone and reabsorption.
- Parathyroid hormone (PTH) - Parathyroid glands are located on the Thyroid Gland. |
|
|
|
Which hormone responds to an increase of blood calcium level (hyperparathyroidism) by decreasing the bone breakdown and reabsorption?
|
Which hormone responds to an increase of blood calcium level (hyperparathyroidism) by decreasing the bone breakdown and reabsorption?
- Calcitonin - Calcitonin pulls calcium out of the blood and puts it into bones |
|
|
|
Why are we so concerned about a CNA pulling a pt up by his shoulders who has hyperparathyroidism?
|
Why are we so concerned about a CNA pulling a pt up by his shoulders who has hyperparathyroidism?
- At risk for breaking bones because the calcium is out of the bones. - Handle gently to prevent fractures |
|
|
|
*Why do we make sure that pt with primary hyperparathyroidism drink large amounts of fluids?
|
*Why do we make sure that pt with primary hyperparathyroidism drink large amounts of fluids?
- To flush the calcium out of blood. - Monitor the I & O. - Forcing fluids to decrease serum calcium levels; limit dietary intake of calcium |
|
|
|
What is a complication of hyperparathyroidism that makes you at risk for falls?
|
What is a complication of hyperparathyroidism that makes you at risk for falls?
- Lack of calcium in the bones. They are now brittle & soft because of lack of calcium in the bones- |
|
|
|
What type of foods should Hypoparathyroid pt consume?
|
What type of foods should Hypoparathyroid pt consume?
- Provide diet high in calcium, low in phosphorous - Dairy - Administer calcium and vitamin D as prescribed |
|
|
|
Why do we not give Calcitonin to pt who is Hypoparathyroid?
|
Why do we not give Calcitonin to pt who is Hypoparathyroid?
- Too low calcium levels in the blood. Need calcium in the blood. (Calcitonin will take the calcium out of the blood and put it into the bone) - Calcitonin will exacerbate the problem. |
|
|
|
What does CRH stand for?
|
What does CRH stand for?
- Corticotropin-Releasing Hormone (CRH) - Produced in the Hypothalamus. - Stimulates release of Adrenocorticotropic hormone (ACTH) by the anterior pituitary. |
|
|
|
*When cortisol is above normal, what hormone is directly suppressed?
|
*When cortisol is above normal, what hormone is directly suppressed?
- Corticotropin-releasing hormone (CRH) |
|
|
|
The adrenal glands (the cortex portion) secretes androgens in men and women?
|
The adrenal glands (the cortex portion) secretes androgens in men and women?
- true |
|
|
|
What is Cushing’s Syndrome (Hypercortisolism)?
|
What is Cushing’s Syndrome (Hypercortisolism)?
- A cluster of clinical abnormalities caused by excessive adrenocortical hormones (particularly cortisol) or related corticosteroids and, to a lesser extent, androgens and aldosterone |
|
|
|
What does a pt with Cushing's syndrome look like?
|
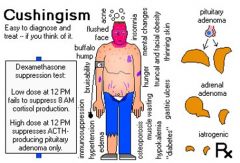
What does a pt with Cushing's syndrome look like?
- Fat trunk (obesity) - Abdominal obesity - Buffalo hump - Small (thin) extremities - Bleeding and Ecchymosis - Hypernatremia (HTN, Edema - Hypokalemia - Supraclavicular Fat pad - Mood Changes - Hyperglycemia |
|
|
|
What is the major function of the adrenal cortex hormone?
|
What is the major function of the adrenal cortex hormone?
- Balancing Glucose - Salt and Water - Adrenal fluids - Situated along the perimeter of the adrenal gland, the adrenal cortex mediates the stress response through the production of mineralocorticoids and glucocorticoids, including aldosterone and cortisol respectively. It is also a secondary site of androgen synthesis. |
|
|
|
What is common cause of Cushing's syndrome?
|
What is common cause of Cushing's syndrome?
- Hyperplasia of the adrenal cortex (above the Kidneys) (Hyperplasia is increased cell production in a normal tissue or organ.) |
|
|
|
In large amounts, does cortisol cause Hyperglycemia?
|
In large amounts, does cortisol cause Hyperglycemia?
- Yes. Causes Hyperglycemia - Large amounts of cortisol does not cause Hypoglycemia (Cortisol levels are decreased which caused Hypoglycemia). |
|
|
|
How is Cushing's syndrome causing personality problems?
|
How is Cushing's syndrome causing personality problems?
- They are moody (bipolar) because sugars are all over the place - Increased cortisol levels cause Mood changes (lability), depression, psychosis, cataracts |
|
|
|
If Cushing's syndrome pt have excessive amount of Glucocorticoids (GC) or Mineralocorticoids what levels would be up?
|
If Cushing's syndrome pt have excessive amount of Glucocorticoids (GC) or Mineralocorticoids what levels would be up?
- the blood sugars (glucose) would be up. Hyperglycemia |
|
|
|
When a pt have increase cortisol levels, what else is up?
|
When a pt have increase cortisol levels, what else is up?
- Hypernatremia is a greater than normal concentration of sodium in the blood. |
|
|
|
What does ACTH stand for?
|
What does ACTH stand for?
- Adrenocorticotropic hormone (ACTH) - ACTH is released by the Anterior Pituitary Gland - ACTH – Stimulates Adrenal Cortex to produce cortical hormones |
|
|
|
Why do we give pt who is scheduled for a bilateral adrenalectomy, steroids?
|
Why do we give pt who is scheduled for a bilateral adrenalectomy, steroids?
- To prevent an adrenal crisis. To compensate for the lack of adrenal hormones. - Administer glucocorticoid preparations before an Adrenalectomy surgery to prevent Adrenal Crisis. |
|
|
|
Why monitor for hypotension in pt who just had a adrenalectomy (besides hemorrhage)?
|
Why monitor for hypotension in pt who just had a adrenalectomy (besides hemorrhage)?
- Because they were given steroids, monitor the BP for fluctuation - Monitor I&O, daily weights, B/P (hypotension), and serum electrolyte levels, prevent injury |
|
|
|
What are we checking for in a pt who is doing a ACTH stimulation test?
|
What are we checking for in a pt who is doing a ACTH stimulation test?
- Checking to see if the Adrenals are working (functioning) - The ACTH stimulation test is a medical test usually ordered and interpreted by endocrinologists to assess the functioning of the adrenal glands stress response by measuring the adrenal response to adrenocorticotropic hormone (ACTH). - The ACTH stimulation test is used to diagnose or exclude primary and secondary adrenal insufficiency, Addison's disease and related conditions |
|
|
|
What S/E would you expect to see if pt sudden stop high dose of steroid therapy?
|
What S/E would you expect to see if pt sudden stop high dose of steroid therapy?
- Hypopituitarism |
|
|
|
What are risk factors for secondary (glucocorticoid deficiency) Adrenal Hypofunction
|
What are risk factors for secondary (glucocorticoid deficiency) Adrenal Hypofunction
- Hypopituitarism, abrupt withdrawal of corticosteroids, removal of ACTH secreting tumor, pituitary injury. |
|
|
|
What is Addison's Disease?
|
What is Addison's Disease?
- Primary Adrenal Hypofunction - Addison’s disease is characterized by the decreased secretion of mineralocorticoids, glucocorticoids, and androgens - Addison’s disease is defined as destruction of 90% of both adrenal glands and is usually caused by an autoimmune process - Addison’s disease is relatively uncommon and can occur at any age and in both sexes |
|
|
|
Why do we watch Addison's disease pt for S/S of infection due to what disturbed body mechanism?
|
Why do we watch Addison's disease pt for S/S of infection due to what disturbed body mechanism?
- Due to stress response (because when we are super stressed, we get sick) - Report all illness – Decreased immune response (stress response) due to decrease in cortisol |
|
|
|
Addison’s disease pt has hypotension due to what disturbance in what hormone?
|
Addison’s disease pt has hypotension due to what disturbance in what hormone?
-Mineralocorticoid |
|
|
|
What interventions are necessary in Addison’s Crisis pt who is receiving steroid therapy?
|
What interventions are necessary in Addison’s Crisis pt who is receiving steroid therapy?
- fluid replacement, IV norm saline - IV hydrocortisone - Urine specific gravity - Vassopressors - glucose monitor hourly - watching glucose, have insulin on hand - Administer steroids as ordered; monitor glucose levels (Increased due to steroids); administer Insulin as needed. - Diet is high in protein and sodium and low in potassium (Hyponatremia and Hyperkalemia) |
|
|
|
What is pheochromocytoma?
|
What is pheochromocytoma?
- A tumor in the Adrenal (Medulla portion) glands (A pheochromocytoma is a rare catecholamine (epinephrine and norepinephrine) secreting tumor derived from chromaffin cells in the Adrenal Medulla.) |
|
|
|
Is a Pheochromocytomas a catecholamine producing tumors?
|
Is a Pheochromocytomas a catecholamine producing tumors?
- Yes. (Pheochromocytomas are catecholamine (Epinephrine and Norepinephrine producing tumors of chromaffin cells in the Adrenal Medulla, that can occur sporadically or as part of a familial syndrome) |
|
|
|
What VS do we diligently watch for in pt’s with pheochromocytoma?
|
What VS do we diligently watch for in pt’s with pheochromocytoma?
- B/P because they have severe HTN |
|
|
|
What is the VMA test for?
|
What is the VMA test for? (and what is does VMA stand for)
- vanillylmandelic acid (VMA) - Tests for the Pheochromocytoma - 24 hour urine test - in 1 container - 24-hour urine collection shows increased catecholamines, metanephrines, and VMA (vanillylmandelic Acid) |
|
|
|
Why tell pt with Pheochromocytoma not to smoke or drink coffee?
|
Why tell pt with Pheochromocytoma not to smoke or drink coffee?
- Because it Increases the B/P (we already have a problem with Severe B/P) - Avoid Smoking, Caffeine, Alcohol |
|
|
|
Why is palpating a pt with Pheochromocytoma contraindicated?
|
Why is palpating a pt with Pheochromocytoma contraindicated?
- Because it releases catecholamine (there is an adrenal crisis now) - Do not palpate abdomen, causes release of catecholamines and HTN -Provide diet increased in calories, vitamins, and minerals, provide calm, restful environment for pts with pheochromocytoma |
|

