![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
90 Cards in this Set
- Front
- Back
|
Paracrine communication |
Use chemical signals to transfer information from cell to cell within a single tissue |
|
|
Endocrine communication |
hormones are released in the circulation by endocrine cells. The hormones alter the metabolic activities of many tissues and organs simultaneously by modifying the activities of target cells |
|
|
Direct communication |
Communication between adjacent cells of the same type which requires extensive physical contact and gap junctions. Ie. Coordination of the ciliary movement among epithelial cells, coordination of contractions of cardiac muscle cells, and propagation of action potentials from one neuron to the next at electrical synapses |
|
|
What are the four mechanisms of intercellular communication? |
Direct communication, paracrine communication, endocrine communication, and synaptic communication |
|
|
What are the three groups of hormones based on chemical structure |
Amino acid derivatives, Peptide hormones, and lipid derivatives |
|
|
What are amino acids derivative hormones |
Small molecules that are structurally related to amino acids. Synthesized from tyrosine, (includes thyroid hormones, epinephrine, norepinephrine, and dopamine) and tryptophan (melatonin) |
|
|
Catecholamines |
Amino acid derivatives hormones produced from tyrosine which include thyroid hormones, epinephrine, norepinephrine, and dopamine |
|
|
Peptide hormones |
Chains of amino acids. Most are synthesizes pro hormones and are converted to active hormones before after they are secreated. |
|
|
What are the two types of peptide hormones? |
Glycoproteins and short peptide/small proteins |
|
|
Lipid derivative hormones |
1. Eicosandoids - important paracrine factors which include leukotrienes and prostaglandins 2. Steroid hormones released by reproductive organs, adrenal glands, and the kidneys.
These hormones are bound to specific transport proteins in the plasma therefore they remain in circulation longer then do secreted peptide hormones |
|
|
How does G protein hormone interaction affect calcium levels |
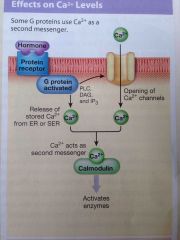
G protein activates the enzyme phospholipase C which triggers a receptor cascade that begins with the production of Diacylglycerol (DAG) and Inositol triphosphate (IP3)
IP3 triggers the release of calcium from intracellular reserves
DAG in intracellular calcium activates protein kinase C which leads to the phosphorylation an opening of calcium channel proteins.
Calcium ions then serve as messengers by binding calmodulin which can then Activate specific cytoplasmic enzymes
This chain is responsible for the excitatory effect of epinephrine and norepinephrine binding to alpha-1 receptors. |
|
|
How does hormone binding increase cyclic AMP in a cell |
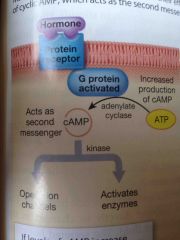
Activation of a G protein activates the enzyme adenylate cyclase which converts ATP to cyclic AMP. Typically cyclic AMP acts as a kinase which adds a high-energy phosphate group to another molecule
This generally has an excitatory effect on the cell |
|
|
How does hormone binding decrease cyclic AMP in the cell? |
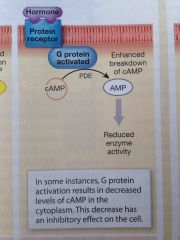
The activated G protein stimulates phosphodiesterase activity and inhibit adenylate cyclase activity. Levels of cAMP then decline which has an inhibitory effect on the cell
Occurs at alpha-2 receptors |
|
|
What are the three mechanisms of hypothalamus control over endocrine function? |

1. Production of antidiuretic hormone and Oxytocin 2. Secretion of regulatory hormones to control activity of the anterior lobe of the pituitary gland. 3. Control of sympathetic output to the adrenal Medullae |
|
|
What are the three mechanisms of hypothalamus control over endocrine function? |
1. Production of antidiuretic hormone and Oxytocin 2. Secretion of regulatory hormones to control activity of the anterior lobe of the pituitary gland. 3. Control of sympathetic output to the adrenal Medullae |
|
|
Describe the anatomy and organization of the pituitary gland |

Back (Definition) |
|
|
Describe the hypophyseal portal system in the pituitary gland |

The superior hypophyseal artery delivers blood to the capillary network of the median eminence. The portal vessels then deliver blood containing regulatory factors to the capillary network within the anterior lobe of the pituitary gland. The inferior hypophyseal artery delivers blood to the posterior lobe of the pituitary gland and hypophyseal veins carry blood containing the pituitary hormones to the cardiovascular system. |
|
|
How many hormones and what kind are released from the pituitary gland |
The pituitary gland releases 9 peptide hormones which bind to membrane receptors and use cAMP as a 2nd messenger. |
|
|
Thyroid stimulating hormone |
TSH, targets the thyroid gland and triggers the release of thyroid hormone. Released in response to thyrotropin releasing hormone from the hypothalamus |
|
|
Adrenocorticotropic hormone |
ACTH, stimulates the release of steroid hormones by the adrenal cortex, specifically target cells that produce glucocorticoids. Occurs understimulation of corticotropin releasing hormone from the hypothalamus. As glucocorticoid levels increase the rates of corticotropin releasing hormone release and subsequent adrenocorticotropic hormone released decline |
|
|
Gonadotropins |
Regulate activity of gonads. Gonadotropin releasing hormone from the hypothalamus stimulates production. There are two types of gonadotropin, follicle-stimulating hormone and luteinizing hormone |
|
|
Follicle-stimulating hormone |
Promotes follicle development in females and in combination with Luteinizing hormone stimulates the secretion of estrogens by ovarian cells.
In males, stimulates nurse cells which promote physical maturation of developing sperm.
Follicle-stimulating hormone production is inhibited by inhibin, a peptide hormone released by cells of the testes and ovaries |
|
|
Follicle-stimulating hormone and Luteinizing hormone |
(FSH). Stimulates follicle development and estrogen secretion and females and sperm production in males.
(LH). Causes ovulation and progesterone production in females, and androgen production in males.
Release of both FSH and LH is promoted by Ganadotropin releasing hormone from the hypothalamus. |
|
|
Prolactin |
(PRL). From the pituitary, together with other hormones, stimulates the development of the memory glands and milk production. |
|
|
How is growth hormone regulated |
By growth hormone releasing hormone and growth hormone inhibiting hormone which are produced in the hypothalamus. Insulin like growth factors inhibit growth hormone releasing hormone and stimulate growth hormone inhibiting hormone |
|
|
Melanocyte stimulating hormone |
Secreted by the pars intermedia. Stimulates the melanocytes of the skin. Dopamine inhibits the release of melanocyte stimulating hormone. Most active during fetal development, in very young children, and in pregnant women. |
|
|
Which nuclei manufacture antidiuretic hormone and oxytocin |
The supraoptic and paraventricular nuclei respectively. |
|
|
What is secreted from the posterior lobe of the pituitary gland |
Antidiuretic hormone and oxytocin |
|
|
What is the function of antidiuretic hormone and how is it stimulated |
ADH acts on the kidneys to retain water and decrease urination. results in elevation of blood volume and pressure.
Is released in response to rise in the solute concentration of blood or fall in blood volume or pressure. Rise in solute concentration is detected by specialized neurons called Osmoreceptors |
|
|
What is the function of oxytocin |
Labor contractions, milk ejection. Also produces contractions of ductus deferens and prostate gland.
Levels peek at orgasm in both sexes |
|
|
Identify the two lobes of the pituitary gland |
The anterior and posterior lobe |
|
|
If a person where dehydrated how would the amount of ADH released by the posterior pituitary lobe change |
The amount of ADH released by the posterior pituitary lobe would increase |
|
|
What are follicle cells in the thyroid and what is their function |
Follicle cells surround the follicle cavity in the thyroid gland. They synthesize a globular proteins called thyroglobulin, which contains the amino acid tyrosine, and secrete it into the colloid of the thyroid follicles. |
|
|
What are the steps involved with the formation of thyroid hormones? |
1. Iodide molecules from the diet are actively transported into the cytoplasm of follicle cells 2. Iodide ions diffuse to the apical surface of each cell where they are converted to iodine by the enzyme thyroid peroxidase 3. Tyrosine molecules with attached iodine atoms become linked by covalent bonds forming molecules of thyroid hormones that remain incorporated into thyroglobulin. The hormone thyroxine is known as T4 and a related hormone is T3 4. Under the influence of thyroid stimulating hormone, follicle cells removed thyroglobulin from the follicles by endocytosis. 5. Enzymes in the cytoplasm breakdown thyroglobulin and the released T3 and T4 molecules diffuse across the basement membrane to enter the bloodstream. 6. In the bloodstream most thyroid hormones are bound by thyroid binding globulin's which form a substantial reserve. |
|
|
What are the two types of cells in the parathyroid gland |
Parathyroid cells, which produce parathyroid hormone, and oxyphils. |
|
|
What are the effects of thyroid hormones on peripheral tissues |
1. Elevates rates of O2 consumption and energy consumption, and in children may cause a rise in body temperature known as the calorigenic effect. 2. Increases heart rate and force of contraction which generally results in increased blood pressure. 3. Increases sensitivity to sympathetic stimulation. 4. Maintains normal sensitivity of respiratory centers to changes in oxygen and carbon dioxide concentrations. 5. Stimulates red blood cell formation and that's enhances oxygen delivery 6. Stimulates activity and other endocrine tissues. 7. Accelerates turnover of minerals in bones |
|
|
What is amplification |
When a small number of hormone molecules bind to a membrane receptor, thousands of second messengers may appear in a cell |
|
|
What are C cells and what is their function? |
Parafollicular cells sandwiched between the cuboidal follicle cells and their basement membrane. Parafollicular cells produce the hormone calcitonin. |
|
|
Aldosterone |
A mineralocorticoid secreted from the zona glomerulosa of the adrenal cortex. Aldosterone targets the kidneys to increase renal reabsorbtion of sodium and water and accelerate urinary loss of potassium. It is stimulated by angiotension two, elevated blood potassium, or fall in blood sodium. Inhibited by ANP and BNP |
|
|
Parathyroid glands |
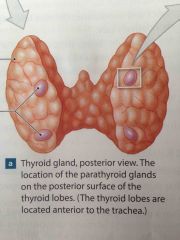
Two pairs of glands located in the posterior aspect of the thyroid gland. |
|
|
Glucocorticoids |
Increased rates of glucose and glycogen formation by the liver, release amino acids from skeletal muscles, and lipids from adipose tissue. Glucocorticoids also have anti-inflammatory effects. Most importantly cortisole |
|
|
Zona reticularis |
Inner layer of adrenal cortex. Under Stimulation by ACTH produces small quantities of androgens. Not important in adult men but in adult women they promote muscle mass and blood cell formation and support the sex drive |
|
|
Describe the homeostatic regulation of calcium ion concentrations |

Back (Definition) |
|
|
What is the function of calcitonin |
Calcitonin inhibits osteoclast activity which slows the rate of calcium release from bone, and stimulates calcium excretion by the kidneys |
|
|
Parathyroid glands |
Two pairs of glands located in the posterior aspect of the thyroid gland. |
|
|
What are the two cell populations of the parathyroid glands? |
Parathyroid cells, which produce parathyroid hormone. And Oxyphils. |
|
|
What are the three effects of parathyroid hormone? |
1. Increases osteoclast activity through stimulation of osteoblasts which secrete a growth factor known as RANKL 2. Enhances resorption of calcium by the kidneys reducing urinary losses 3. Stimulates the formation and secretion of calcitriol by the kidneys, which in turn enhances calcium and potassium absorption by the digestive tract |
|
|
What is the adrenal gland and where is it found? |
Highly vascularized glands near the level of the 12th rib on the superior border of each kidney. |
|
|
What is the adrenal cortex and what is its function? |
The outer layer of the adrenal gland which produces steroid hormones known as corticosteroids. The adrenal cortex consist of an outer zona glomerulosa, middle zona fasiculata and inner zona reticularis. |
|
|
Zona glomerulosa |
Outer region of the adrenal cortex which produces mineralocorticoids. |
|
|
Mineralocorticoids |
Steroid hormones that affect the electrolyte composition of body fluid. |
|
|
What are C cells and what is their function? |
Parafollicular cells sandwiched between the cuboidal follicle cells and their basement membrane. Parafollicular cells produce the hormone calcitonin. |
|
|
Aldosterone |
A mineralocorticoid secreted from the zona glomerulosa of the adrenal cortex. Aldosterone targets the kidneys to increase renal reabsorbtion of sodium and water and accelerate urinary loss of potassium. It is stimulated by angiotension two, elevated blood potassium, or fall in blood sodium. Inhibited by ANP and BNP |
|
|
Parathyroid glands |
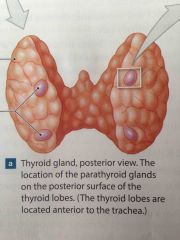
Two pairs of glands located in the posterior aspect of the thyroid gland. |
|
|
Glucocorticoids |
Increased rates of glucose and glycogen formation by the liver, release amino acids from skeletal muscles, and lipids from adipose tissue. Glucocorticoids also have anti-inflammatory effects. Most importantly cortisole |
|
|
Zona reticularis |
Inner layer of adrenal cortex. Under Stimulation by ACTH produces small quantities of androgens. Not important in adult men but in adult women they promote muscle mass and blood cell formation and support the sex drive |
|
|
Describe the homeostatic regulation of calcium ion concentrations |

Back (Definition) |
|
|
What is the effect of stimulation of alpha-1 and beta-1 receptors |
Accelerates the use of cellular energy and mobilization of energy reserves |
|
|
What is the function of calcitonin |
Calcitonin inhibits osteoclast activity which slows the rate of calcium release from bone, and stimulates calcium excretion by the kidneys |
|
|
Parathyroid glands |
Two pairs of glands located in the posterior aspect of the thyroid gland. |
|
|
What are the two cell populations of the parathyroid glands? |
Parathyroid cells, which produce parathyroid hormone. And Oxyphils. |
|
|
What are the three effects of parathyroid hormone? |
1. Increases osteoclast activity through stimulation of osteoblasts which secrete a growth factor known as RANKL 2. Enhances resorption of calcium by the kidneys reducing urinary losses 3. Stimulates the formation and secretion of calcitriol by the kidneys, which in turn enhances calcium and potassium absorption by the digestive tract |
|
|
What is the adrenal gland and where is it found? |
Highly vascularized glands near the level of the 12th rib on the superior border of each kidney. |
|
|
What is the adrenal cortex and what is its function? |
The outer layer of the adrenal gland which produces steroid hormones known as corticosteroids. The adrenal cortex consist of an outer zona glomerulosa, middle zona fasiculata and inner zona reticularis. |
|
|
Zona glomerulosa |
Outer region of the adrenal cortex which produces mineralocorticoids. |
|
|
Mineralocorticoids |
Steroid hormones that affect the electrolyte composition of body fluid. |
|
|
What is the pineal gland and where is it found? |
Part of the epithalamus, which Lies in the posterior portion of the roof of the third ventricle.
Pinealocytes synthesize melatonin which may protect against damage by free radicals, may play a role in human sexual maturation and may influence circadian rhythms. |
|
|
Where is the pancreas found and what does it secrete |
A mostly retroperitoneal organ lying in the loop between the inferior border of the stomach and the proximal portion of the small intestine. Secretes glucagon, insulin, a peptide hormone identical to growth hormone inhibiting hormone, and pancreatic polypeptide. |
|
|
Where is the pancreas found and what does it secrete |
A mostly retroperitoneal organ lying in the loop between the inferior border of the stomach and the proximal portion of the small intestine. Secretes glucagon, insulin, a peptide hormone identical to growth hormone inhibiting hormone, and pancreatic polypeptide. |
|
|
What are the four cell types found in the islets of Langerhans |
Alpha cells - glucagon Beta cells – insulin Delta cells – peptide hormone identical to growth hormone inhibiting hormone F cells - pancreatic polypeptide |
|
|
What is the function of insulin |
Accelerates glucose uptake, accelerates glucose utilization, stimulates glycogen formation, stimulates triglyceride formation in adipose tissue |
|
|
What is the function of insulin |
Accelerates glucose uptake, accelerates glucose utilization, stimulates glycogen formation, stimulates triglyceride formation in adipose tissue |
|
|
What is the function of glucagon |
Stimulates the breakdown of glycogen in skeletal muscle and liver cells, stimulates the breakdown of triglycerides in adipose tissue, stimulates the production release of glucose by the liver |
|
|
How is blood glucose concentration regulated? |

Back (Definition) |
|
|
What is diabetes mellitus |
When glucose concentrations are high enough to overwhelm the reason absorption capabilities of the kidneys |
|
|
Type 1 diabetes |
Inadequate insulin production.
People with type one diabetes require insulin and usually require multiple injections daily or continuous infusion through an insulin pump |
|
|
Galactorrhea |
A milky discharge from the nipple not related to normal breast-feeding |
|
|
Hashimoto's disease |
A disorder in which the immune system attacks the thyroid gland. The most common cause of hypothyroidism in the United States |
|
|
Hirsutism |
Excessive growth of facial or body hair in a woman. A sign of hyperandrogenism. May also be a sign for polycystic ovarian syndrome, congenital adrenal hyperplasia, or androgen secreting tumors. |
|
|
Hypercalcemic tetany |
Muscle spasms affecting face and upper extremities caused by low calcium concentration body fluid. |
|
|
Type 2 diabetes |
The most common form of diabetes mellitus. Tissues do not respond properly to insulin in a condition known as insulin resistance. Diet and exercise can be an effective treatment. |
|
|
Describe the renin – angiotensin – aldosterone system |

Back (Definition) |
|
|
Erythropoietin |
A peptide hormone released by the kidneys in response to low oxygen levels. EPO stimulates red bone marrow to produce red blood cells |
|
|
Renin |
Released by juxtaglomerular cells in the kidney in response to sympathetic stimulation or decline in renal bloodflow.
Renin converts angiotensinogen to angiotensin 1.
In the capillaries of the lungs angiotensin-converting enzyme modifies angiotensin 1 to the hormone angiotensin 2.
Angiotensin II stimulates the secretion of aldosterone by the adrenal cortex and ADH from the posterior lobe of the pituitary gland
The result is retained salt and water as well as elevated blood pressure. |
|
|
What hormones are secreted by the heart and how is secretion stimulated |
The heart secretes natriuretic peptides if the volume of the blood becomes too great and the endocrine cells of the atria and ventricles are stretched
Natriuretic peptides promote the loss of sodium and water by the kidneys and inhibit running release and the secretion of ADH and aldosterone.
The net effect is a reduction in both blood volume and blood pressure |
|
|
Describe the renin – angiotensin – aldosterone system |
Back (Definition) |
|
|
What is leptin |
A peptide hormone released from adipose tissue which is part of the negative feedback control of appetite |
|
|
What are the three phases of the stress response? |
1. Alarm phase – activation of the sympathetic nervous system mobilizes energy reserves, increases mental alertness etc. 2. Resistance phase – if the stress lasts longer than a few hours. Glucocorticoids dominant, epinephrine, growth hormone and thyroid hormones are also involved. Lipids are mobilized and used in the peripheral tissues while the liver synthesize glucose from other carbohydrates, amino acids, and lipids. 3. Exhaustion phase - The resistance phase results in a conservation of sodium at the expense of potassium. As potassium content decreases cells begin to malfunction. If not corrected almost immediately organ systems will begin to fail |
|
|
Exophthalmos |
Abnormal protrusion of the eyeballs |
|
|
What are the nine hormone secreted by the pituitary gland? |
Thyroid stimulating hormone Adrenocorticotropic hormone Follicle-stimulating hormone Luteinizing hormone Prolactin Growth hormone Melanocyte stimulating hormone Antidiuretic hormone Oxytocin |

