![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
100 Cards in this Set
- Front
- Back
|
Function: maintain homeostasis by producing and secreting hormones. Controls and regulates what?
|
Energy
Growth Fluid and electrolytes Balance Stress Sexual reproduction |
|
|
Endocrine Glands
|
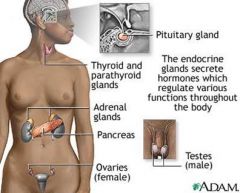
(see picture)
|
|
|
The CNS interacts with the endocrine system through
|
a hypothalmus-pituitary pathway
|
|
|
Stimulating hormones are believed to be synthesized in what gland?
|
hypothalamus
|
|
|
Chemical messengers that transmit information between body cells and organs Some hormones affect __________ Others affect ________, Many hormones are _______
|
all cells
target tissues cyclic |
|
|
Think in terms of (regarding secretion)
|
hyper-secretion and hypo-secretion
|
|
|
Everything in system is responsible for
|
maintaining a balance
|
|
|
Pharmacologic Treatment What are the 7 methods of treatment?
|
Hypothalmic and Pituitary Hormones
Corticosteroids come from adrenal glands Thyroid and Antithyroid Bone and Calcium regulation Antidiabetic Estrogen, progestin, contraceptive Androgen and anabolic steroids |
|
|
Corticosteroids (glucocorticoids or steroids) - Hormones produced by the adrenal gland Maintain _________ (state); Have profound effects both ________& ________; Act as an _________________
|
Maintain homeostasis
Have profound effects both therapeutic and adverse Act as an anti-inflammatory |
|
|
ADRENAL CORTEX - What are the 3S’s?
|
sugar, salt and sex
|
|
|
Gonadal hormones
|
lookup
|
|
|
Glucocorticoids and Mineralocorticoids - What are Cortisol and aldosterone together called?
|
Together called the corticosteroids
|
|
|
What are the primary functions of corticosteroids?
|
Carbohydrate, protein and fat metabolism
Electrolyte and water metabolism Cardiovascular functions Immune effects Effects are Widespread |
|
|
Why do you give PO meds with food?
|
to decrease GI upset
|
|
|
Why do you take daily doses of PO meds before 9AM
|
to match body’s circadian rhythms
|
|
|
Increase dose of PO meds during periods of _______________
|
stress (surgery)
|
|
|
Anticipate ulcer formation and start what PO medications?
|
antacids or H2 antagonists
|
|
|
Do not abruptly DC PO meds, instead__________
|
taper dose
|
|
|
Monitor blood sugars if diabetic – why do you notify the MD while taking steroids?
|
Notify MD for adjustment of diabetic meds while taking steroids
|
|
|
With PO meds, monitor for acute infection treat __________
|
treat quickly
|
|
|
With PO meds, increase activity to reduce bone __________________
|
reduce bone demineralization
|
|
|
Diabetes Mellitus is caused by insufficient secretion of ___________ from _______ cells. It primarily involves the body’s inability to metabolize ________________ due to diminished effectiveness of ___________.
|
Insufficient secretion of insulin from beta cells
Primarily involves the body’s inability to metabolize carbohydrates due to deficiency or diminished effectiveness of insulin |
|
|
Diabetes Mellitus Type 1 = ______________ (%?) Type 2=____________ (%) Third type? __________
|
Type 1: Insulin-Dependent (10-12%)
Type 2: Non-Insulin Dependent (85-90%) Secondary |
|
|
Type 1 Diabetes – Abrupt failure of the __________________, ________ cells disabled, Absolute insulin ____________________
|
Abrupt failure of the pancreas (autoimmune disease)
Beta cells disabled Absolute insulin dependency |
|
|
Type 2 – Resistance to ___________ action in target tissues, ____________ insulin secretion, Inappropriate hepatic ________________
|
Resistance to insulin action in target tissues
Abnormal insulin secretion Inappropriate hepatic gluconeogenesis |
|
|
Secondary: Caused by what?
|
Gestational
Stress Related - Use of adrenal corticosteroids, oral contraceptives, and other drugs that antagonize the effects of insulin |
|
|
Blood Sugar Ranges What is normal? When is a person diabetic according to ADA? (Fasting and Random levels) What determines the amount of medication? What is the most sensitive test?
|
Normal is 90’s-120’s
According to the American Diabetes Association a person is diabetic if: Fasting blood glucose >126 mg/dl Random blood glucose > 200 mg/dl Serum glucose levels determine amount of medication Most sensitive test is glycated or glycosylated hemoglobin (Hgb A1c) |
|
|
Polyuria (↑peeing) is an example of
|
Hyperglycemia
|
|
|
Seizures is an example of
|
Hypoglycemia
|
|
|
Coma is an example of
|
Hypoglycemia
|
|
|
Polydipsia (↑thirst) is an example of
|
Hyperglycemia
|
|
|
Polyphagia(↑ hunger) is an example of
|
Hyperglycemia
|
|
|
Nausea is an example of
|
Hypoglycemia
|
|
|
Numbness is an example of
|
Hypoglycemia
|
|
|
Tingling of lips/tongue is an example of
|
Hypoglycemia
|
|
|
Weight loss is an example of
|
Hyperglycemia
|
|
|
Fatigue is an example of
|
Hyperglycemia
|
|
|
Hunger is an example of
|
Hypoglycemia
|
|
|
Weakness is an example of
|
Hyperglycemia
|
|
|
Vision changes is an example of
|
Hyperglycemia
|
|
|
Irritability is an example of
|
Hypoglycemia
|
|
|
Tremors is an example of
|
Hypoglycemia
|
|
|
Frequent skin infections is an example of
|
Hyperglycemia
|
|
|
Confusion is an example of
|
Hypoglycemia
|
|
|
Vaginal discomfort is an example of
|
Hyperglycemia
|
|
|
Dry, itchy skin is an example of
|
Hyperglycemia
|
|
|
Cold & clammy skin is an example of
|
Hypoglycemia
|
|
|
Hot & sweaty skin is an example of
|
Hyperglycemia
|
|
|
What are the Oral Hypoglycemics?
|
Sulfonylureas (PO)
Alpha-Glucosidase Inhibitors (PO) Biguanide (PO) Glitazones (PO) Meglitinides (PO) |
|
|
Short Acting insulin Starts how fast? Peaks when? Gone after how long? Given by what route? What are the types?
|
Start ½ to 1 hr
Peak 2-3 hrs Gone 5-7 hrs The only insulin given IV Types - Regular, Humulin R, Novolin R |
|
|
Intermediate Acting insulin Starts how fast? Peaks when? Gone after how long? What visually indicates Intermediate Acting insulin? What are the types?
|
Start 1-2 hrs
Peak 8-12 hrs Gone 18-24 hrs Cloudy Types - NPH, Humulin N, Novolin N |
|
|
Long Acting insulin Starts how fast? Peaks when? Gone after how long? What is the type?
|
Start 4-8
Peak 10-30 Gone 36 plus Type – Ultralente |
|
|
What are some other situations when insulin may be beneficial?
|
May also be required during times of stress such as illness, infection or surgery
Used to control diabetes induced by pancreatitis, hormones, drugs and pregnancy Also used to treat hyperglycemia related to IV parenteral nutrition or Hyperkalemia |
|
|
What is Hyperkalemia?
|
Insulin and dextrose causes potassium to move from blood into the cells
|
|
|
Insulin – Absorption
|
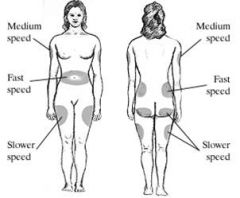
(see picture)
|
|
|
Insulin Administration – Keep at what temp? How is it administered? Do you massage the site? Which insulin do you draw up first?
|
Kept at room temp
Given SQ in units using an insulin syringe and needle Do not massage site Mixing Insulin: Draw up regular insulin first; NPH next |
|
|
Nursing Considerations
|
Assess for ketoacidosis
Assess for hypoglycemic reaction -Treat with OJ, hard candy, glucose 10-20g po or SL or buccal mucosa; follow with milk, bread, crackers, or meal -THINK, THINK, THINK---if giving NPH, when might you expect to see a hypoglycemic reaction? When it peaks Teach when they should take it. Medic-Alert bracelet Adverse effects: -Hypoglycemia, weight gain, allergic reactions |
|
|
What is notable about Insulin Pen Injectors?
|
Prefilled and reusable
Examples: Humulin 70/30 and Humalog 75/25, Lantus |
|
|
What is different about Insulin Pumps? What kind of insulin can be used in a pump?
|
Implantable (abd) and portable
Can be d/c for bathing, swimming for 1-2 hrs Rapid acting only (Regular or Humalog) Not NPH or Lente – unpredictable results |
|
|
PO Anti-Diabetic Drugs
|
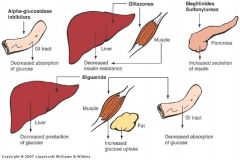
(see pic)
|
|
|
Sulfonylureas
Action |
Lowers blood glucose by increasing insulin secretion
Requires functioning beta cells Contraindicated in hypersensitivity to sulfa drugs, severe renal or hepatic impairment, pregnancy. |
|
|
Sulfonylureas Drugs:
|
1st Generation: rarely used
2nd Generation: stronger duration of action; less s/e than 1st Generation - Glipizide (Glucotrol, Glucotrol XL) Glyburide (DiaBeta, Glynase, PresTab,) - Glimepiride (Amaryl) |
|
|
Sulfonylureas: Side Effects?
|
Hypersensitivity
Hypoglycemia NV Metallic taste (like tin can) Blood dyscrasias (a lysing of blood cells) |
|
|
Sulfonylureas: Administration
|
Take 30 min before breakfast or BID (or r/o hypoG.)
Verify admin w/ NPO status Avoid ETOH (sugar from yeast) |
|
|
Biguanide Action:
|
Increases the use of glucose by muscle and fat
Decreases hepatic (liver) glucose production Decreases intestinal absorption of glucose |
|
|
Biguanide Drugs
|
Metformin (Glucophage)
Drug of choice in obese clients with new onset type 2 |
|
|
Biguanide Side Effects:
|
Weight loss
Anorexia Flatulence Nausea Stomach pain Vomiting Lactic acidosis |
|
|
Biguanide Contraindications
|
Diabetes with fever or infections
Trauma or surgery Pregnancy Hepatic or Renal impairment Cardiac or respiratory insufficiency Lactic acidosis |
|
|
Biguanide Administration:
|
Given 2-3 times qd w/ meals
Does not cause hypoglycemia Excreted unchanged by the kidneys. Do not give with liver/renal disease. Avoid ETOH. |
|
|
Alpha-Glucosidase Inhibitors & PTU ACTION:
|
Delay digestion of complex CHI into glucose
|
|
|
Alpha-Glucosidase Inhibitors & PTU DRUGS:
|
Acarbose (Precose)
Glitazones |
|
|
New Diabetic Agents
|
Pramlintide (Symlin)
Exenatide (Byetta) Sitagliptin (Januvia) |
|
|
Pramlintide (Symlin) Is a synthetic version of _________________? Action? Side Effects? Administer with what therapy?
|
Synthetic version of human amylin
Slows gastric emptying of food Can decrease appetite, potentially resulting in weight loss Use with insulin therapy |
|
|
Exenatide (Byetta) 2 Actions?
|
Increases glucose sensitive insulin secretion from beta-cells
Slows gastric emptying of food |
|
|
General Nursing Considerations
|
Teaching
Nutrition and exercise Medic alert bracelet Maintain good foot and skin care Neuropathy (can’t feel them) No sticking, trimming nails, etc. Teach client and family the sx, prevention, and tx of hypoglycemia (elderly especially) and hyperglycemia. Watch for liver toxicity Jaundice, pale stools, dark urine Best Practices—careful medication management watch for “opathys” |
|
|
What is the Thyroid ?
|
The thyroid is a small, butterfly-shaped gland in the mid-lower neck.
It’s primary function is to control the body’s metabolism. |
|
|
What does the Thyroid secrete? What has to be present in order to produce?
|
Secretes T3 andT4 (thyroxine) and Calcitonin
Production of T3 and T4 is dependent on the presence of iodine Probably all cells have receptors for thyroid hormones Regulates metabolism Stimulates protein and fat catabolism Insulin antagonist Necessary for growth and development (esp brain and skeletal) |
|
|
Hypothyroidism – What are the 4 types?
|
Primary
Secondary Congenital Adult |
|
|
Primary Hypothyroidism (it’s in the gland)
|
Chronic (Hashimoto’s) thyroiditis
Autoimmune disorder Treatment of Hyperthyroidism (radiation or surgery) |
|
|
Secondary Hypothyroidism (from pituitary gland)
|
Decreased TSH from the pituitary or hypothalamus
|
|
|
Congenital Hypothyroidism (cretinism)
|
Child is born without a thyroid gland or with a poorly functioning gland
|
|
|
Adult Hypothyroidism (myexedema)
|
Myxedema coma: severe, life-threatening hypothyroidism
|
|
|
Myxedema (see pics)
|
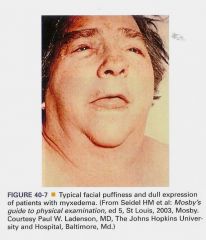
Flattens ridge of nose, tongue swollen
|
|
|
Signs and Symptoms of Hypothyroidism (everything slow, cold & shut down)
|
Decreased BP
Decreased HR Slowed drug metabolism Use caution with opioids and sedatives Lethargy, fatigue Weight gain Cold intolerance Constipation Dry skin Dry and thinned hair Thick, hard nails Prolonged menstrual periods Increased susceptibility to infection |
|
|
Drugs to Treat Hypothyroidism (These drugs provide an exogenous source of thyroid hormone)
|
Levothyroxine (Sythroid, Levothroid)
Liothyronine (Cytomel, Triostat) Liotrix (Thyrolar) |
|
|
Liothyronine (Cytomel, Triostat)
|
Synthetic T3
Rapid onset and shorter duration of action More pronounced CV side effects |
|
|
Liotrix (Thyrolar)
|
contains levothyroxine and liothyronine
|
|
|
Levothyroxine (Sythroid, Levothroid) Action and Use?
|
ACTION: Synthetic form of T4
USE: Drug of choice for long-term treatment of hypothyroidism May take several months to reach peak effect |
|
|
Levothyroxine SIDE EFFECTS:
|
Adverse effects include signs and symptoms of hyperthyroidism
Watch for chest pain, heart palpitation, nervousness, or insomnia |
|
|
Levothyroxine NURSING CONSIDERATIONS:
|
Take every morning on an empty stomach
Iron, antacids, cholestyramine, sucralfate (these decrease absorption) Check pulse before taking—hold and notify MD if >100 Do not stop taking drug abruptly can lead to life-threatening illness Brand names differ; do not switch drugs Monitor T4 and TSH |
|
|
Hyperthyroidism is caused by what? What disease falls under this category and what is the treatment?
|
Usually associated with excessive number of thyroid cells and excessive secretion of thyroid hormone
|
|
|
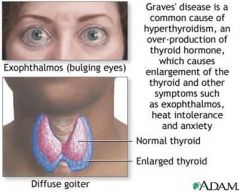
Graves Disease (See Pic) - Treatment is:
|
drugs to block thyroxine
Radiation to destroy the gland Subtotal thyroidectomy |
|
|
Hyperthyroidism carries a risk of _________storm or ____________ crisis
|
thyroid storm or thyrotoxic crisis
Going to explode, have a stroke right there |
|
|
Symptoms of Hyperthyroidism:
|
Rapid pulse
Palpitations Tremors Heat intolerance Irritability Exophthalmos Weight loss Excessive perspiration Nervousness Increased appetite |
|
|
Drugs for Hyperthyroidism
|
Methimazole (MMI) [P]
Propylthiouracil (PTU) Potassium Iodide (Lugol’s Solution, SSKI) Sodium Iodide (Radioactive Iodine) Propranolol (Inderal) |
|
|
Methimazole (MMI)– Prototype Action, Use and Adverse effects:
|
ACTION:
Inhibits production of thyroid hormones therefore new T4 and T3 are not produced Does not interfere with release of previously produced hormone So therapeutic effects may not occur for several days or weeks---not good in thyroid storm USE: Suppress hyperthyroidism and Graves disease ADVERSE EFFECTS: s/s of hypothyroidism, blood disorders, rash, headache, N/V/D, hepatitis. |
|
|
Potassium Iodide - Lugol’s Solution and SSKI (strong iodine solution and saturated solution of potassium iodide) Action, Use and Nursing Consideration?
|
ACTION:
Inhibit secretion of thyroid hormones USE: Iodine preparation used in short-term treatment of hyperthyroidism Used to treat thyroid storm and decrease size of thyroid gland before thyroidectomy NURSING CONSIDERATION: Do not give PTU, methimazole, or radiactive iodine after giving this drug |
|
|
Sodium Iodide (Radioactive Iodine) Action, Use, Side Effects?
|
ACTION:
Is converted to protein-bound iodine by the thyroid gland for use when needed Contraindicated in pregnancy and lactation USE: In small amounts can be used in diagnostic tests of thyroid function In large amounts used to treat thyroid cancer SIDE EFFECTS: May cause cancer and chromosomal damage in children In children should only be used for hyperthyroidism that cannot be controlled by other drugs or surgery May lead to hypothyroidism, necessitating lifelong hormone replacement Bone marrow depression |
|
|
Hyperthyroidism: Patient Teaching Guidelines for Medications - Nursing Considerations:
|
Take at regular intervals around the clock
Avoid foods high in iodine (soy, tofu, seafood, salt) May need to be taken for up to 1year or longer in order to decrease thyroid hormone levels to normal DO NOT stop abruptly! Tests of thyroid function and dosage adjustments may be needed (TSH, T3 and T4) |
|
|
Propranolol (Inderal) is NOT an antithyroid, what is it? When is it used?
|
Antiadrenergic---NOT antithyroid
Used in thyroid storm and to control symptoms while waiting for response to anti-thyroids |

