![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
71 Cards in this Set
- Front
- Back
|
What are the three primary effects of thyroid hormone?
|
1: increase BMR
2. induce gluconeogenesis 3. coordinate normal growth and development |
|
|
How do thyroid hormones increase BMR?
|
generate futile cycles where triglycerides are being made and broken down at the same time
increase the expression of Beta adrenergic receptors |
|
|
What kind of a drug could you use to treat overproduction of thyroid hormones?
|
beta adrenergic antagonist
|
|
|
What disease state results if hypothyroidism is left untreated in the first weeks of birth?
|
Cretinism-irreversible mental retardation
|
|
|
Explain thyroid hormone control?
|
TRH-(+)->TSH(+)-->T3/T4(-)->TRH
|
|
|
Explain the purpose of using the Radioactive Iodine uptake test?
|
Because the thyroid is one of the few places where iodine is absorbed you can trace it to the follicles.
If the thyroid is enlarged (graves) you see a bigger dark shape a hot spot means one area is unresponsive to TSH and is constitituively active |
|
|
What will the size of the colloid be in a person with graves disease?
|
Very tiny follicles with tall columnar epithelium b/c it is awlays active
|
|
|
Explain the production of thyroid hormones
|
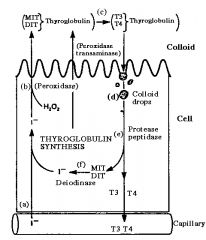
a) iodine from the diet is actively transported across the cell membrane
b) trapped iodine is transfered across the cell into the lumen where it is linked to tyrosine to form MIT and DIT (in thyroglobulin) c) MIT and DIT are convered to T3 and T4 with the aid of peroxidase and transaminase d) T4 and T3 are reabsorbed into the cell in the form of colloid droplets e) T4 and T3 are separated from thyroglobulin f) T4 and T3 are secreted into the circulation. Any uncoupled MIT and DIT are diodinated to release tyrosine and iodine |
|
|
What converts thyroxine to active T3 inside of cells?
|
5'-iodinase (3-4x more potent than T4)
|
|
|
What class of drug could prevent thyroid hormones from being produced?
|
A thyroid peroxidase blocker (makes the DIt and the MIT) eg propylthiouracil
|
|
|
In what form is most of the thyroid hormone stored?
|
Thyroxine (90% is T4)
|
|
|
Why does a patient with hypothyroidism or hyperthyroidism develop a goiter?
|
sustained high levels of TSH from lack of negative feedback from T4/t3 or from the trophic effects of TSI in graves disease cause hyperplasia of the thyroid
|
|
|
What is the mechanistic cause of Hashimoto's thyroiditis?
|
autoantibodies against thyroid peroxidase and antithyroglobulin
|
|
|
What is the mechanism of Graves disease?
|
thyroid stimulating immunoglobulin are produced by the immune system it is an analog of TSH
|
|
|
What are the 4 roles of parathyroid hormone?
|
1. Stimulates bone resorption
2. Decrease in renal calcium excretion 3. Increase in renal phosphate excretion 4. Final step in vitamin D synthesis in the kidney |
|
|
What 3 factors regulate the secretion of PTH?
|
1. Plasma free calcium levels (decrase = pth secretion-sensed through CaSR receptors in cheif cells)
2. Plasma [phosphate]-increase = increased PTH secretion 3. VItamin D-PTH stimulate vitamin D synthesis which exerts negative feedback on PTH |
|
|
What form is most phosphate in?
|
alkaline phosphate 4:1
|
|
|
What role does vitamin D play in the body?
|
regulates calcium/phosphate homeostasis
|
|
|
How is vitamin D made?
Which step is regulated? |
7 dihydrocholesterol is exposed to light to become cholecalciferol (or it comes from th ediet) which the liver makes into 25 hydroxycalciferol then the kidney makes it into 1,25 (calcitrol) the active form
hydroxylation in the kidney is the regulated step that is stimulated by PTH |
|
|
What controlsl Vitamin D production?
|
PTH
phosphate inhibits vitamin D synthesis even though it does increase PTH low calcium stimulate vitamin D synthesis |
|
|
What kind of hormones does the adrenal cortex secrete?
|
Steroid hormones
|
|
|
What kind of catecholamine predominates adrenal medullary secretions?
|
EPINEPHRINE; nor epi is for NEURons
|
|
|
How do adrenal cortex hormones have an effect on adrenal medulla secretions?
|
The adrenal medulla receives high concentrations of adrenal steroids b/c there is a portal venous blood supply.
The adrenal cortex hormones (cortisol) stimulate release of the medulla catecholamines |
|
|
What substrate and enzyme is necessary for steroid production?
|
LDL cholesterol
Desmolase |
|
|
What enzyme is necessary for adolsterone creation and in what cell?
|
Glomerulosa cells have adlosterone synthase
|
|
|
What enzyme is necessary for cortisol creation and in what cell does this occur?
|
17 alpha hydroxylase in the fasciulata
|
|
|
Why is lack of cortisol potentially fatal?
|
Hypotension results due to lack of sympathetic stimulation
|
|
|
What enzyme is unique to the reticularis and the fasciculata that allows them to secrete cortisol?
|
17 alpha hydroxylase
|
|
|
What part of the renal cortex has aldosterone synthase?
|
Glomerulosa
|
|
|
What are 3 roles of cortisol?
|
mobilize glucose, amino acids, and fatty acids
resist inflammatory and immune responses increase blood glucose |
|
|
When are cortisol levels the highest?
|
highest in the morning and lower during late afternoon and prior to sleep.
|
|
|
What other hormone is created upon synthesis of adrenalcorticotrophic hormone?
|
Melanocyte stimulating hormone!!
|
|
|
In a case of ACTh insufficiency why would aldosterone continue to be produced?
|
B/c it is stimulated by angiotensin 2 and only weakly by ACTH
|
|
|
Why does excess ACTH cause hyperpigmentation?
|
B/c when cortisol is produced so is melanocyte stimulating hormone
|
|
|
What enzyme allows the precursors for both androgens and mineralcorticoids and glucocorticoids to become corticosteroids?
|
21 alpha hydroxylase.!! w/o this you get congenital adrenal hyperplasia
|
|
|
What is 11 beta hydroxysteroid dehydrogenase and what can inhibit it?
|
It deactivates cortisol and is expressed in addition to aldosterone which prevents cortisol from blocking aldosterone receptors.
Licorice blocks it.-results in hypertension etc why? |
|
|
Why does synthetic glucocorticoid therapy result in water retention?
|
It overwhelms the ability of 11 beta hydroxysteroid dehydrogenase which means that cortisol agonizes the receptors for the mineralcorticoids causing increased sodium and therefore water retention in the kidney.
|
|
|
What are the three stimuli for the release of renin?
|
1. reduced distension of the afferent arteriole
2. tubuloglomerular feedback 3. stimulation of renal sympathetic nerves (baroreceptor reflex) |
|
|
What is addison's disease?
|
primary failure of the entire adrenal cortex
symptoms are: hypoglycemia-cortisol hypotension-cortisol Weakness and fatigue-cortisol Hypovolemai-aldo increased pigmentation-too much ACTH = alpha melanocyte Reduced libido in FEMALES |
|
|
What is Cushing's syndrome? not to be confused with Cushing's disease.
|
Too much cortisol maybe from corticosteroids;
Hyperglycemia, muscle wasting, truncal obesity, hypertension -mineralcorticoids |
|
|
What is Conn's syndrome?
|
Hyperaldosteronism-hypertenion, hypokalemia, metabolic alkalosis
things that prevent blood flow to the kidney can cause 2ndary hypoaldosteronism. |
|
|
What is the rate limiting enzyme of making catecholamines?
|
Tyrosine hydroxylase
|
|
|
What does the final conversion from norepinephrin to epinephrine and *only* occurs in chromaffin cells?
|
Phenylethanolamine N methyltransferase
|
|
|
What controls release of catecholamines from the adrenal medulla?
|
CNS
|
|
|
What stimulates Phenyl N methyltransferase to convert nor epi to epi?
|
Cortisol!
|
|
|
Why would you want to give someone with tachycardia a epinephrine antagonist rather than a norepinephrine antagonist?
|
B/c epinephrine like Beta receptors more than norepinephrine
(closer in the alphabet) |
|
|
Name the major effectors of the following receptor subyptes:
alpha 1 beta 1 beta 2 |
alpha 1 -vasodilator
beta 1-heart contractile beta 2-relaxes smooth muscle of the lungs |
|
|
What can be measured in the urine to determine the amount of catecholamines being produced by the adrenal medulla?
|
VMA-vanillymlmandelic acid -is created by MAO using epinephrine
|
|
|
What is a pheochromocytoma?
|
a secretory tumor of the adrenal medulla
|
|
|
When is GH secretion the highest?
|
during the first 2 hours of sleep
|
|
|
What factors results in increased GH secretion?
|
Acute stress
hypoglycemia through ghrelin starvation |
|
|
What are the 2 functions of growth hormone?
|
Stimulates lineal growth through IGF (somatomedin)
Metabolic effects that oppose insulin |
|
|
What is the largest source of plasma IGf1
|
Liver also secreted in many tissue
|
|
|
What controls the secretion of GH?
|
IGF-1
|
|
|
What is the advantage of having plasma proteins bound to IGF1 even though it is a peptide hormone?
|
It allows for a more stable amount of IGF1 to circulate.
|
|
|
Explain feedback in GH IGF axis?
|
GH inhibits its own secretion
IGF-1 inhibits GH secretion directly at somatotropes IGF-1 inhibits hypothalamic GHRH IGF1 stimulates hypothalamic somatostatin |
|
|
What is the main regulator of glucagon levels and why?
|
Insulin, it has to flow from the center toward the periphery and suppresses glucagon secretion as it goes into the blood.
|
|
|
What is the first screening method for diabetes?
|
microalbuminuria
|
|
|
What mediates the effects of insulin in a cell?
|
Receptor tyrosine kinases (number of receptors is important for determining response-obesity lowers the number of receptors)
|
|
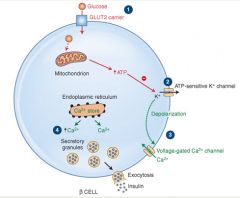
Explain the mechanism of insulin secretion:
|
Glucose is taken up by glut 2 to produce Atp
Inhibits atp sensitive potassium channel which depolarizes the membrane Depolarization activates voltage sensitive calcium channels causing and influx of calcium Calcium induced calcium release triggers exocytosis of secretory granules continaing insulin. |
|
|
What is an incretin? Name one example?
|
GIP GLP1 (glucagon like peptide)-
incretins are GI peptide hormones that stimulate insulin secretion that are secreted in response to eating allows an increase in plasma insulin levels ONLY when in conjunction with high blood glucose levels |
|
|
What is the Wolff Chaikoff effect?
|
Too much iodine actually causes hypothyroidism
|
|
|
What is the main function of glucagon?
|
Makes the liver perform gluconeogenesis and make ketone bodies (beta hydroxybutyrate and acetoacetic acid) from acetyl coA
increase lipolysis and proteolysis |
|
|
What is the effect on glucagon and insulin of eating a protein rich meal?
|
It increases both glucagon and insulin secretion, minimizing the change in the concentrations and preventing the development of hypoglycemia
|
|
|
What is the short term reaction to hypoglycemia, what is the long term reaction to starvation?
|
Short term-glucagon/catecholamines
Long term-cortisol and GH |
|
|
DIagnose the following glucose levels:
70-99 100-125 126+ |
Normal
prediabetes diabetic nonfasting over 200 is diagnostic if they have the 3 Ps |
|
|
What is one major difference in the symptoms between Type 1 and Type 2 diabetes?
|
Type 2 does not produce ketoacidosis b/c there is still enough hepatic resposne to insulin to prevent ketogenesis
|
|
|
Primary hyperparathyroidism
|
Stones, bones, groans, psychiatric overtones
|
|
|
What is metabolic syndrome?
|
Increased risk of both cardiovascular disease and type 2 diabetes
|
|
|
What causes the following forms of dwarfism?
Achondroplasia- Pituitary Dwarfism Laron Dwarfism Cretinism- |
Achondroplasia-gene defect for cartilage FGF receptor
Pituitary dwarfism-GRH, GH, IGF1 deficiency Laron dwarfism-unresponsive GH receptors Cretinism: hypothyroidism in children-thyroid hormones are permissive for action of GH |
|
|
What hormone results in pubic hair development in women?
|
DHEA (weak adrogens)
|

