![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
describe the transition from estrogen to progesterone synthesis |
when the LH surge arrives at the ovary, it will change its synthesis from E to P (happens quickly)
at first, both are made, but true "reorganization that favors P synthesis" by about 24 hours after onset of LH surge |
|
|
what are the effects of increased progesterone synthesis? |
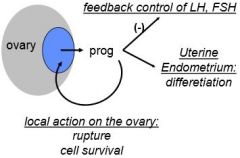
progesterone has feedback control at the hypothalamus endometrium and necessary for ovulation and the formation of the CL |
|
|
what drives follicle rupture? what else may play a role |
increased expression of many proteases, leads to degradation of the follicle wall
carefully coordinated series of events
the increased hydrostatic pressure from swelling of the follicle (with plasma) following LH surge may work in concert with the proteases to cause follicle rupture (but not sufficient alone) |
|
|
what causes meiosis in the oocyte to resume? |
LH surge causes meiosis to resume from prophase I, complete meiosis I and arrest in metaphase II |
|
|
describe the periovulatory changes to the oocyte. when is it fertilizable? |

fertilizable once it reaches metaphase II |
|
|
what drives the re-initiation of meiosis in the oocyte? |
when LH arrives, the loss of cAMP (cAMP locks the cell) so now the lock is gone
1) through desensitization of mural g.c. layer 2) uncoupling of transmural processes from cumulus layer to oocyte 3) activation of PDE3 (phosphodiesterase) which turns cAMP into AMP |
|
|
what's the effect of the LH surge on the cumulus layer? |
causes cumulus expansion, mediated by EGF family members and proteases |
|
|
what are the functions of the cumulus expansion? |
cumulus expansion allows extrusion of the oocyte (loosens it from the wall of the follicle)
hyaluronic acid in the cumulus matrix maintains dispersion of cumulus cells and facilitates sperm capacitation; cells contain ++ survival factors for the egg and sperm chemotactic factors |
|
|
where are the 2 places in the adult human body where angiogenesis occurs? |
1) the formation of the corpus luteum 2) the restructuring of the endometrium following menstruation |
|
|
what's a potential target for contraception besides endocrine disruption? |
targeting angiogenic process in the developing corpus luteum |
|
|
what are the primary hormone products of the corpus luteum? what are their functions? |
1) estrogen: endometrial proliferation during 1st half of the cycle, differentiation if fertilization, gonadotropin feedback, and "local actions ??" (not certain)
2) progesterone: endometrium, and in the event of fertilization, maintains pregnancy and CL |
|
|
progesterone has important ____ functions; there is ____-____ feedback |
progesterone has important local functions; there is autocrine-paracrine feedback |
|
|
what hormone maintains the corpus luteum in women? |
LH
GnRH and hence LH supports mid-luteal progesterone production vs. GnRH cessation and hence stopping LH would shut down progesterone production and cause pre-mature menstruation |
|
|
what makes up the bulk of the CL? why so important? |
vascular cells makes up about half the mass, so important to get progesterone out and into circulation efficiently
(critical for maintaining pregnancy) |
|
|
the CL is a very complicated gland. what are the main 4 cell types? |
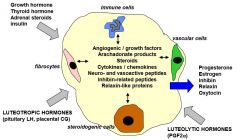
steroidogenic cells derived from g.c. and theca cells
number of immune cells increases
|
|
|
what defines the end of the menstrual cycle? |
"death" of the corpus luteum during a non-fertile cycle, the process is called luteolysis |
|
|
what's our best guess for how luteolysis works in a human? |
loss of trophic support probably represents a decline in sensitivity to LH
(just a hypothesis, we don't really know) |
|
|
what's corpus luteum rescue? |
the process during a fertile cycle by which the early embryo secretes hCG (chorionic gonadotropin) that has a high affinity on LH and CG receptors to keep progesterone alive and thus maintain the CL for about 7 weeks until the placenta takes over progesterone production |
|
|
what hormone prevents contraction of the uterus? |
progesterone maintains quiescence of the myometrium of the uterus
important to maintain early preganancy; its declining levels causes cramps around the time of menstruation |
|
|
the CL differentiates from the ____, specifically the ____ and ____ cells |
the CL differentiates from the follicle, specifically the granulosa and theca cells |
|
|
the lifespan of the CL depends solely on the fate of the ____ |
the lifespan of the CL depends solely on the fate of the oocyte
(2 weeks in non-fertile cycle vs. 7 weeks in fertile cycle) |
|
|
steroid and peptide products have ____ and ____ effects to regulate cycle length |
steroid and peptide products have local and central effects to regulate cycle length |
|
|
______ of the CL is essential for the next cycle of follicular growth vs. ____ of the CL is essential for pregnancy |
regression of the CL is essential for the next cycle of follicular growth (through loss of P relieving negative feedback on FSH) vs. rescue of the CL is essential for pregnancy |
|
|
what vasculature is lost with menstruation? then what happens? |
spiral arteries
then re-formed under the influence of estrogen in the first half of the cycle, the site of angiogenesis every cycle *potential cycle target |
|
|
other than the spiral arteries, what other part of the endometrium is lost and re-formed every cycle? |
the straight necks of the glands |
|
|
what's causes the very dense layer at the apical surface of the endometrium and what do you call it? |
the zona compacta, forms under the influence of progesterone |
|
|
describe the changes of the glands and stroma caused before ovulation. caused by ____ |

estrogen |
|
|
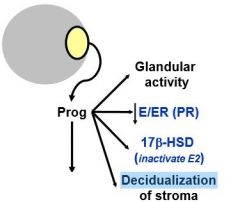
describe the changes of the glands and stroma caused after ovulation. caused by ____ |

estrogen and progesterone |
|
|
what hormone is involved in "pre-decidualization"? and what is it? |
progesterone --> pre-decidualization of the luminal epithelial cells causes increased gland production and changes in luminal morphology (cells become rounded and store glycogen) |
|
|
what's estrogen's primary role on the endometrium in the first half of the cycle? what are the intermediaries? |
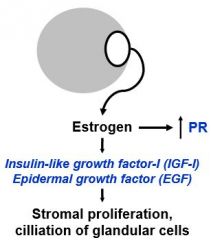
stromal proliferation and increases the expression of the progesterone receptor (PR); preparing the endometrium to respond once P is present |
|
|
what are 4 major effects of progesterone during the second phase of the cycle? |
|
|
|
summarize what happens when progesterone levels decline |
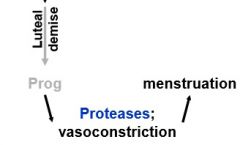
P withdrawal via luteolysis --> protease release** |
|
|
what's behind the loss of blood during menstruation? |
as spiral arteries in the functionalis constrict, there is extravasation of blood into the stroma (the uterine lumen) |
|
|
what's the main theme of this lecture? |
that chemical messengers, in the form of steroids, especially estrogen and progesterone are integrating the female reproductive system in time and space
so that the hypothalamus, pituitary, ovaries, and uterus can all work in concert with one another |
|
|
where does fertilization occur? |
at the junction between the ampulla and the oviduct |
|
|
what is a fertilized egg called when it enters the uterus and implants? |
a blastocyst |
|
|
what stops most of the sperm from reaching the oocyte? |
the cervix, cervical mucus, only about 100k of 250 to 500 million reach the uterine cavity; fewer than 100 reach the distal end of the oviduct |
|
|
where do sperm mature? |
in the epididymis |
|
|
how long can the cervix store sperm? |
up to 72 hours |
|
|
_____ occurs during the passage of sperm through the cervical ____. what 3 things does this process involve? |
capacitation occurs during the passage of sperm through the cervical mucus this imparts: 1) the ability to undergo the acrosomal rxn 2) hypermotility and 3) ability to bind to the zona pellucida |
|
|
what allows the sperm to get through the cumulus matrix? |
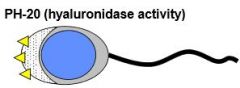
hyaluronidase activity expressed by the head of the sperm |
|
|
what are the 4 steps of fertilization starting with the sperm arriving at the zona pellucida? |
1) the sperm arrives at the zona pellucida, where 2) contact and binding initiates the acrosomal reaction i.e. the breakdown of the acrosome and the release of enzymes that 3) degrade the ZP and 4) an acrosome process that is an actin filament will form and make contact with the oocyte's plasma membrane |
|
|
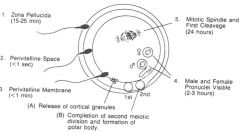
what are the consequences of the actin filament of the sperm making contact with oocyte's plasma membrane |
this initiates a wave of calcium within the oocyte; this results in: 1) fusion of the sperm plasma membrane with that of the oocyte --> allows the release of nuclear, genetic material from the sperm into the egg 2)the second is the cortical reaction |
|
|
explain the initiation of the "cortical reaction" |
as part of the calcium wave initiated by the acrosomal reaction, there is the fusion and release of vesicles called cortical granules that line the oocyte and contain very important enzymes this is called a block to polyspermy (i.e. fertilization by more than one sperm) |
|
|
how does the cortical reaction block polyspermy? |
the calcium wave initiates fusion of these cortical granules and release of their enzymes into the space between the egg and the ZP; they break down the ZP proteins into very specific fragments, which fuse together and form an impenetrable barrier to additional sperm; the primary block to polyspermy in humans (occurs within a couple of minutes) |
|
|
what 3 things happen as far as meiosis in response to the sperm binding? |
in response to sperm binding, there is 1) the completion of the second meiotic division and 2) the extrusion/formation of the second polar body, so 3) within 2-3 hours after the arrival of the sperm, you can see the male and female pronuclei (under light microscopy); |
|
|
describe the pronuclei and zygote in terms of haploid and diploid. |
each haploid genome in the pronucleus fuse together to form one complete diploid genome and within about 24 hours, there will be the first division |
|
|
what happens to the zygote before implantation? |
several rounds of cell division occur before implantation, while the zygote and ultimately the early embryo transits the oviduct and enters the lumen of the uterus |
|
|
what's a zygote? |
a zygote is a fertilized egg prior to first division (you can see the pronuclei) |
|
|
what is still intact at the 2-cell stage of the early embryo? why is it important? |
2-cell stage, ZP is still intact, very important because it prevents the early embryo from adhering to the wall/the endometrium and implanting these cells divide again and again to form a morula (a solid mass of cells) and develops into a blastocyst (i.e. a morula that has developed a cavity |
|
|
what critical step allows the blastocyst to contact the cells of the endometrium and implant? |
the blastocyst hatches from the ZP, which is very very important because the cells of the blastocyst are then able to contact the cells of the endometrium directly |
|
|
describe the events right after fertilization: where does fertilization occur? when does cell division occur? what are the next two phases? |
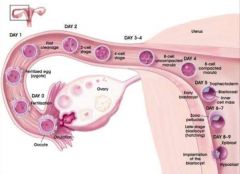
*fertilization occurs at the delay in the junction of the ampulla and the isthmus, *cell division begins within a couple of days, *by day 4-5 you have a blastocyst and *by the end of day 7 or 8, you have adherence and implantation into the endometrium |
|
|
what essential hormone does the early embryo produce? why so important? |
even at these early stages of development, even especially (day 4, morula), cells of the early embryo begin to produce hCG and rescue the CL, so an early pregnancy test would show positive even if you haven't missed your period yet |
|
|
what is compaction? |
compaction: the physical constraint of the growth of the early embryo; the ZP constrains the volume in which the early embryo has to develop, so as these cells divide, they have increasingly smaller space in which to divide |
|
|
what does compaction cause? |
compaction forces polarization of these cells early on in division due to limited states, which results in division in a basal vs. apical manner, the differentiation of cells of the inner cell mass as they divide across this axis into the pluriblast and the trophoblast |
|
|
what does the pluriblast become? what does the trophoblast become? |
pluriblast becomes the embryo
trophoblast becomes the placenta and extraembryonic membranes |
|
|
simply put, what 2 steps follow sperm penetration of the ZP? |
sperm penetration of the ZP --> initiates acrosome reaction --> initates calcium wave |
|
|
what 2 things does the calcium wave allow? |
1) allows fusion of sperm and egg, and 2) the cortical reaction, a block to polypsermy by the "hardening of the ZP" |
|
|
when does cell division begin? |
cell division begins within about a day after the pronuclei fuse |
|

describe the timeline of fertilization |
|

