![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
List 4 main Adrenal Disorders
|
Cushing’s syndrome
Adrenal insufficiency (Addison’s disease) Congenital adrenal hyperplasia Primary aldosteronism Pheochromocytoma |
|
|
What are the four main types of Congenital Adrenal Hyperplasia? What do do they cause? |
17 alpha-hydroxylase deficiency 21 alpha-hydroxylase deficiency 11 Beta1- hydroxyls deficiency 3 Beta Hydroxysteriod Dehydrogenase Deficiency |
|
|
How does a 17 alpha hydroxylase deficiency affect aldosterone levels? What are the associated symptoms? How does this affect Ang II? |
the levels of aldosterone will be decrease (this is due to the RAAS system)the increased level of 11 deoxycorticosterone and corticosterone cause symptoms of mineralocorticoid excess leading to HTN, Metabolic alkalosis and hypokalemiaHTN inhibits renin secretion leading to decrease Ang II and Aldosterone.Hypokalemia also inhibits aldosterone secretion directly |
|
|
How does a 17 alpha-hydroxylase deficiency affect steroid production. Describe the presentation.
|

Excessive production of mineralocorticoids by the adrenal also results in hypertension and hypokalemia
|
|
|
How does a 21 alpha-hydroxylase deficiency affects steroid production? Describe the presentation.
|

Hypotension, hyperkalemia, poor feeding, loss of weight, dehydration, loss of sodium in urine.
|
|
|
T or F: Aldosterone levels decrease due to 17 alpha-hydroxylase deficiency as a result of regulation by the RAAS system. |
False:
Levels of aldosterone INCREASE in this deficiency and do not decrease due to RAAS negative feedback.
This is because Mineralocorticoids due to increases amounts of 11 deoxycorticosterone. |
|
|
Complete the following table for a patient with 21-alpha-hydroxylase deficiency |
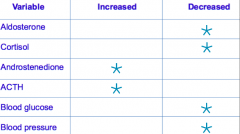
|
|
|
What is primary aldosteronism and what does it lead to? |
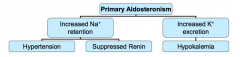
Autonomous aldosterone excess
Suppression of renin by negative feedback
Sodium retention (Hypertension)
Potassium secretion (Hypokalemia in some patients, Most patients are normokalemic)
|
|
|
What is Hyperaldosteronism? What is primary hyperaldosteronism and what causes it, and what is the most important clinical manifestation?
|
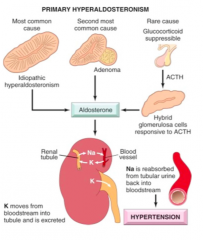
Hyperaldosteronism-a group of closely related conditions characterized by chronic excess aldosterone secretion.
• Hyperaldosteronism may be primary, or it may be secondary to an extra-adrenal cause. • Primary hyperaldosteronism stems from an autonomous overproduction of aldosterone, with resultant suppression of the renin-angiotensin system and decreased plasma renin activity. • Blood pressure elevation is the most common manifestation of primary hyperaldosteronism, which is caused by one of three mechanisms |
|
|
What is bilateral idiopathic hyperaldosteronism, is it a primary or secondary cause? Describe the typical patient and what is possibly mutated?
|
• Characterized by bilateral nodular hyperplasia of the adrenal glands
• The most common underlying cause of primary hyperaldosteronism • Patients tend to be older and to have less severe hypertension than those presenting with adrenal neoplasms. • The pathogenesis remains unclear, possible mutation in a potassium channel. |
|
|
Aldosterone Regulation
|
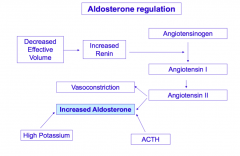
|
|
|
Describe the pathohistology presentation of bilateral idiopathic hyperaldosteronism. What must be excluded as a cause of hyperaldosteronism? |
bilateral idiopathic hyperplasia
Marked by diffuse and focal hyperplasia of cells resembling those of the normal zona glomerulosa.
• The hyperplasia is often wedge-shaped, extending from the periphery toward the center of the gland.
• The enlargement may be subtle and adrenocortical adenoma must be carefully excluded as the cause for hyperaldosteronism. |
|
|
What is Conn’s Syndrome? What is the typical age and sex presentation? |
A adrenocrotical neoplasia causing primary hyperaldosteronism is due to a solitary aldosterone secreting adenoma
This syndrome occurs most frequently in adult middle life and is more common in women than in men (2 : 1). |
|
|
Adrenocoritcal neoplasias are most commonly caused by ________ and rarely caused by____________.
|
Adrenocortical neoplasm: either an aldosterone producing adenoma (most common) or, rarely, an adrenocortical carcinoma Can have multiple adenomas
|
|
|
Describe the gross and microscopic appearance of aldosterone-producing adenomas (ie color, cell type, resemble). Are these tumors visible on imaging? |
These are almost always solitary, small (<2 cm in diameter), well-circumscribed lesions, more often found on the left than on the right.
• They are often buried within the gland and do not produce visible enlargement, a point to be remembered in interpreting sonographic or scanning images.
• They are bright yellow on cut section and , are composed of lipid-laden cortical cells that resemble fasciculata cells than glomerulosa cells (the normal source of aldosterone).
• Cells tend to be uniform in size and shape. |
|
|
In what age and gender group do aldosterone secreting adenomas occur?
|
30s and 40s, in women more than men.
|
|
|
What is Glucocorticoid-remediable hyperaldosteronism? What genes and enzymes are affected, and how does this affect aldosterone? |
An uncommon cause of primary familial hyperaldosteronism.
Due rearrangement involving chromosome 8 that places CYP11B2 (the gene that encodes aldosterone synthase) under the control of the ACTH responsive CYP11B1 gene promoter.
ACTH stimulates the production of aldosterone synthase (required in the last step in aldosterone synthesis)
Aldosterone production is under the control of ACTH (suppressible by dexamethasone) |
|
|
What are the 5 clinical manifestations of primary aldosteronism ?
|
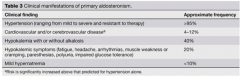
|
|
|
What is the most important consequence of hyperaldosteroneism? Describe the effects of renal mineralocorticoid receptors? What are the long term effects of this disease?
|
The most important clinical consequence of hyperaldosteronism is hypertension
• Through its effects on the renal mineralocorticoid receptor, aldosterone promotes sodium reabsorption, which secondarily increases the reabsorption of water, expanding the extracellular fluid volume and elevating cardiac output. • The long-term effects of hyperaldosteronism - induced hypertension are cardiovascular compromise and an increase in the prevalence of adverse events such as stroke and myocardial infarction. • Some normokalemic patients are now diagnosed |
|
|
What causes the hypokalemia in primary hyperaldosteroneism and how does it present? |
Hypokalemia results from renal potassium wasting and, when present, can cause a variety of neuromuscular manifestations, including weakness, paresthesias, visual disturbances, and occasionally frank tetany. |
|
|
Primary Aldosteronism Screening targets which patients? What other factors should be considered? |
Who to screen? Hypertensives and Hypokalemia Elevated ratio of Aldosterone/PRA (plasma renin activity) Interfering drugs
– Must discontinue (markedly affect the ratio) •Potassium-sparing diuretics (diuretics lower the circulating volume and raise rennin)
• Potassium-wasting diuretics
• Liquorice-root products (gum and tobacco)
– Consider withdrawing “if possible”
• Most other antihypertensive agents (and NSAIDs)
– Verapamil SR, hydralazine, and alpha-1 antagonists are OK • Many false-positive results due to ubiquity of low-renin essential hypertension |
|
|
Primary Aldosteronism Confirmation
|
Confirmation by “salt-loading”
Normal persons will suppress aldosterone if filled with salt
Most common protocols
Oral salt loading with measurement of urinary aldosterone IV Saline load with measurement of plasma aldosterone
|
|
|
How are Aldosterone-Producing Adrenal Adenomas managed?
|
Surgery
– Unilateral adrenalectomy • Usually laparoscopic surgery • Results of surgery – Resolution of hypokalemia – Improvement (> 95%) or resolution (30-65%) of HTN |
|
|
How is Bilateral Adrenal Hyperplasia managed?
|
Spironolactone
– Aldosterone receptor antagonist – Side effects: gynecomastia (men), hyperkalemia, If gynecomastia, try eplerenone instead (due to inhibition of adrogen receptors) Amiloride – Inhibits Na reabsorption in distal tubule and collecting duct (thereby reducing K secretion) – Not as effective as spironolactone – Side effect: hyperkalemia |
|
|
How is Glucocorticoid-Remediable Aldosteronism managed? |
– Give small dose of dexamethasone at bedtime
• Suppress AM surge of ACTH – With suppression of ACTH, normal renin-angiotensin system control of aldosterone resumes
– Side effects • Potential for HPA axis suppression and secondary adrenal insufficiency |
|
|
What is secondary hyperaldosteronism? Described the characteristic findings and which conditions it is caused by.
|
Aldosterone release occurs in response to activation of the renin-angiotensin system. It is characterized by increased levels of plasma renin and is encountered in conditions such as: Decreased renal perfusion (arteriolar nephrosclerosis, renal artery stenosis) Arterial hypovolemia and edema (congestive heart failure, cirrhosis, nephrotic syndrome) Pregnancy (due to estrogen-induced increases in plasma renin substrate)
|
|
|
What is Pheochromocytoma? Which cells cause this tumor and treatment can correct whatfinding? Describe the features
|
Pheochromocytomas are neoplasms composed of chromaffin cells, which synthesize and release catecholamines and in some instances peptide hormones. These tumors can surgically correct hypertension.
Traditionally, the features of pheochromocytomas have been summarized by the “rule of 10s”.
• Ten percent of pheochromocytomas are extra-adrenal. • Ten percent of sporadic adrenal pheochromocytomas are bilateral. • Ten percent of adrenal pheochromocytomas are biologically malignant. • Ten percent of adrenal pheochromocytomas are not associated with hypertension. |
|
|
What factors contribute to the pheochromocytoma presentation
|
Hereditary
Bilateral Extra-adrenal Malignant |
|
|
Describe causes of Multiple endocrine neoplasia (MEN) type 2.
|
Type 2A: Medullary thyroid CA
– Pheochromocytoma – Hyperparathyroidism Type 2B: Medullary thyroid CA – Pheochromocytoma – Multiple neuromas – Marfanoid habitus 50% of MEN2 patients develop pheo |
|
|
What is the classic triad for of signs and symptoms in Phaeochromocytoma? What is the affect of catecholamines? How does Blood pressure present?
|
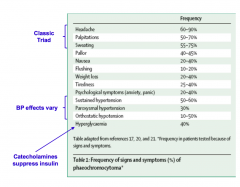
catecholamines are released in paroxysms from adrenal tumors, so there are spells of these triads.
Lack of these indicate less posibility of pheo |
|
|
What are the signs signs and symptoms pheo?
|
Classically occur in “spells” (paroxysms)
– Typically last minutes to hours – Can be elicited by variety of stimuli • Food • Exercise • Drugs • Anesthesia • Tumor manipulation |
|
|
What are some differentials for pheochromocytoma?
|
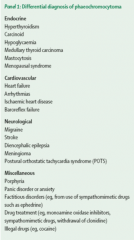
The Great Mimic
|
|
|
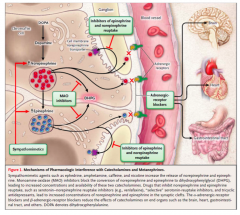
Pheochromocytoma can be detected in urine? How? What enzymes are involved? What metabolic product is commonly present?
|
Pheochromocytomas are associated with the urinary excretion of catecholamines or their metabolic breakdown products.
These catecholamines are broken down by two enzymes, catecholamine orthomethyltransferase (COMT) and monoamine oxidase (MAO), into: homovanillic acid, normetanephrine, metanephrine, or vanillylmandelic acid (VMA). Any of these metabolic products may be found in the urine of patients with pheochromocytomas; however, VMA is most common. The best screening tests are 24-h urinary metanephrine and VMA levels. |
|
|
Who should get tested for pheochromocytoma and how is it performed?
|
Who?
– Resistant hypertension – Paroxysms suggestive of phew – Genetic predisposition – Adrenal incidentaloma How? – Plasma catecholamines or metabolites – Urine catecholamines or metabolites |
|
|
Biochemical testing for pheo relies on plasma_________. Why? |
Current screening: plasma metanephrines (MN)
– Metanephrines are continuously released from pheo
– Very high sensitivity • Picks up nearly all pheos • Negative test excludes pheo nearly all the time
– Conveniently performed
– Problem: Lot of false-positive results • Confirm (or refute) positive screening plasma MN with 24 hour urine collection for catecholamines and MN
– Problem: Lots of drugs interfere with the tests |
|
|
Pharmacological Interference with Catecholamines and Metanphrines
|
|
|
|
What is dynamic testing for pheochromocytoma?
|
Clonidine suppression test
– Clonidine suppresses catecholamine release from normal sympathetic activation – Failuretosuppressafterclonidine->Pheo Glucagon stimulation test – In pheo, glucagon causes NE levels to rise 3X – Not recommended: Test can be fatal! |
|
|
What diagnostic tests are used to confirm hyperaldosteronism?
|
The diagnosis of primary hyperaldosteronism is confirmed by elevated ratios of plasma aldosterone concentration to plasma renin activity; if this screening test is positive, a confirmatory aldosterone suppression test must be performed, because many unrelated causes can alter the plasma aldosterone and renin ratios.
|
|
|
How is hyperaldosteronism treated (primary, secondary, and adenomas) ?
|
Adenomas are amenable to surgical excision.
Surgical intervention is not very beneficial in patients with primary hyperaldosteronism due to bilateral hyperplasia, which often occurs in children and young adults. These patients are best managed medically with an aldosterone antagonist such as spironolactone. The treatment of secondary hyperaldosteronism rests on correcting the underlying cause stimulating the renin-angiotensin system. |

