![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
56 Cards in this Set
- Front
- Back
|
***EXAM***
An elderly black female was admitted to the hospital from a nursing home because of progressive weakness. Her labs revealed a serum total calcium level of 8.2 mg/dL (normal 9.0-11.0 mg/dL), serum phosphorus of 2.6 mg/dL (normal 3.0-4.5 mg/dL) 25- hydroxyvitamin D level was 4 pg/dL (normal: 10-55 pg/dL), and her iPTH level was 161 pg/dL (normal: 14-72 pg/dL). What will you use to treat her? (select all that apply) A. Calcium B. Vitamin D C. Calcitonin D. Parathyroid hormone |
Calcium
Vitamin D (Calcitonin decreases Ca+, PTH is too high) |
|
|
What are some causes of hypercalcemia?
(select all that apply) A. PT gland tumor makes too much PTH B. Tumor interferes with PTH production C. Malignant tumor produces PTH-related protein (PTHrP) D. Chronic kidney disease E. Too much vitamin D F. Vitamin D deficiency G. Cancer that metastasizes to bone, stimulates osteoclast formation and activation, and causes bone resorption |
A. PT gland tumor makes toomuch PTH
C. Malignant tumor produces PTH-related protein (PTHrP) E. Too much vitamin D G. Cancer that metastasizes to bone, stimulates osteoclast formation and activation, and causes bone resorption |
|
|
What causes more symptoms? An acute increase in serum Ca+ or a slow, chronic increase in Ca+
|
Acute Increase in Ca+
|
|
|
Hypercalcemia decreases the concentrating ability of the kidneys. What is the mechanism?
What symptoms would you see? |
Hypercalcemia
↓ Down regulate aquaporin-2 channels ↓ Decreases concentrating ability of kidneys **Symptoms** -Polyuria -Polydipsia (thirst) -DEHYDRATION |
|
|
How does hypercalcemia affect the GI system?
|
Decreases GI smooth muscle contractility
↓ CONSTIPATION, nausea, anorexia |
|
|
How can you approach treating
hypercalcemia? |
↑ Ca+ excretion
↓ absorption of Ca+ ↓ osteoclast activity (inhibit bone resorption) |
|
|
A 63-year-old female has lost her appetite with weight loss, and is constipated. She has been urinating a lot and complains of thirst. Her blood pressure is 110/70 mm Hg, heart rate is 80 bpm.
Her mucus membranes are somewhat dry and sticky. Serum creatinine is 2.1 mg/dL (normal 0.6- 1.2 mg/dL), with normal electrolytes and glucose levels, but serum calcium is 14.1 mg/dL (normal 9.0-11.0 mg/dL). What would be the best treatment? |
IV normal saline
**restores volume status** **dilutes serum Ca+** **Facilitates urinary Ca+ excretion** |
|
|
What diuretic will increase Ca+ excreted by the kidney?
|
Loop Diuretic
|
|
|
When might you use a loop diuretic to treat hypercalcemia?
(select all that apply) A. When they are severely dehydrated B. If they develop edema after IV saline C. If they are asymptomatic with mildly elevated serum Ca D. In a patient with symptomatic hypercalcemia and heart failure |
B. If they develop edema after IV saline
D. In a patient with symptomatic hypercalcemia and heart failure |
|
|
You are treating a patient with severe symptomatic hypercalcemia.
What would you add if they have renal failure or heart failure? |
Loop Diuretic
|
|
|
What happens to bone with
primary hyperparathyroidism and hypercalcemia of malignancy? |
Bone Resorption
|
|
|
When bone resorption is increased, what happens to serum Ca+ and phorphorus?
|
↑ Ca+ and P
|
|
|
What hormone decreases
osteoclast activity? |
Calcitonin
|
|
|
What affect does calcitonin have on Ca+ and Phosphorus?
(Think about bone and kidneys) |
Bone: ↓ resorption = ↓ Ca+ and P
Kidney: ↓ Ca+ and P reabsorption ** Calcitonin ↓ serum Ca+ ** |
|
|
Explain tachyphylaxis and calcitonin
|
Tachyphylaxis - efficacy is limited to 1st 48 hours
|
|
|
Name the drug class:
Etidronate – oral, IV Tiludronate – oral Pamidronate – parenteral Alendronate– oral Risedronate – oral Ibandronate – oral, IV Zoledronic acid – parenteral |
Bisphosphonates
("-dronate") |
|
|
"-dronate" = ??
|
Bisphosphonates
|
|
|
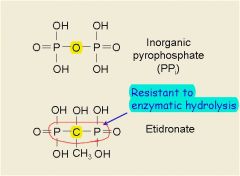
What advantage do biphosphonates have over inorganic pyrophosphate?
|
|
|
|
You are treating a patient with biphosphonates. What happens to bone resorption?
|
DECREASES
d/t slowed osteoclast activity |
|
|
MOA:
- Strong affinity for bone (hydroxyapatite crystals), targeting especially bone surfaces undergoing remodeling - Concentrate at sites of active remodeling - Taken up by osteoclasts - Inhibit osteoclast activity and cause apoptosis - Selectively inhibit osteoclast-induced bone resorption |
Biphosphonates
|
|
|
How long do biphosphonates work?
|
- The drugs are not metabolized and remain bound to bone for weeks
- Remain in the matrix until the bone is remodeled and then released |
|
|
Which agent would be most useful in preventing hypercalcemia and adverse skeletal events in a patient with metastatic cancer to bone.
A. IV normal saline B. Bisphosphonate C. Calcitonin D. Furosemide E. Hydrochlorothiazide |
B. Bisphosphonate
|
|
|
Which biphosphonate is more likely to cause osteomalacia?
Pamidronate or Etidronate |
Etidronate
(Inhibits bone mineralization) [Pamidronate does not inhibit bone mineralization as much] |
|
|
What biphosphonate would you use in a patient with osteoporosis to combat hypercalcemia?
|
Pamidronate
Will not cause osteomalacia!!! |
|
|
Which biphosphonate causes renal toxicity?
|
Zoledronic Acid
|
|
|
What drugs cause
osteonecrosis of the jaw? |
**Biphosphonates**
-trauma to the jaw along with continued stress of chewing -bone has limited capacity for healing d/t biphosphonate tx |
|
|
What drugs may cause esophagitis?
|
Biphosphonates!
|
|
|
How can PTH secretion be
reduced? |
Raise serum Ca+ levels
sensitize the Ca+ sensing receptors |
|
|
What drug sensitizes Ca+ receptors on the parathyroid gland which ↓ PTH?
|
Cinacalcet
|
|
|
MOA:
- Enhances the sensitivity of the calcium-sensing receptors in the parathyroid to Ca - Lowers the concentration of Ca at which PTH is suppressed - Decreases PTH secretion - Decreases serum calcium levels |
Cinacalcet
|
|
|
Clinical Use:
Hypercalcemia associated with parathyroid carcinoma |
Cinacalcet
|
|
|
Why would you not use Cinacalcet to treat hypercalcemia of
malignancy (not referring to parathyroid carcinoma)? |
There wouldn't be an increase in PTH levels to begin with!
(This is PTH-Independent hypercalcemia) |
|
|
Name a side effect of Cinacalcet
|
HYPOcalcemia
|
|
|
What can contribute to a vitamin
D deficiency? |
Lack of Sunlight
CKD Nutritional Deficiency Malabsorption |
|
|
What does vitamin D
deficiency cause in kids? What about Adults? |
Kids = RICKETS
Adults = OSTEOMALACIA |
|
|
What is the primary cause of
hypocalcemia from a vitamin D deficiency? |
↓ GI absorption of Ca+
|
|
|
A patient has ↓ GI absorption of Ca+. What does this do to PTH, Bone, and Ca+/P in the kidneys?
|
↑ PTH
↑ Bone resorption ↑ Ca+ reabsorption ↓ Phosphate reabsorption |
|
|
Vitamin D uses UV light absorbed through the skin to become activated in the kidneys. What is the active form of Vitamin D?
|
1,25 (OH)2 D3
(active, calcitriol) |
|
|
Vitamin D Preparations:
- Cholecalciferol - Ergocalciferol - Calcitriol Which is: -pure vitamin D2? -active 1,25 dihydroxyvitamin D3? - pure vitamin D3? |
- Cholecalciferol = pure Vitamin D3
- Ergocalciferol= pure Vitamin D2 - Calcitriol= 1,25 dihydroxyvitamin D3 |
|
|
Why does chronic kidney disease
cause a vitamin D deficiency? |
You can't activate vitamin D3 into 1,25 dihydroxyvitamin
D3 |
|
|
What usually happens to
phosphorus and PTH with chronic kidney disease? |
↑ Phosphorus
(kidneys are shot) ↑ PTH (low Ca+ levels stimulate Ca+ release) |
|
|
What can happen to Ca levels if a patient with chronic kidney disease has high enough PTH levels?
|
Normal Ca+ or hypercalcemia
(d/t ↑ PTH) |
|
|
Lab results for a 58-year-old male with stage 5 CKD reveal the following. Serum total calcium 8.5 mg/dL (normal 9.0-11.0 mg/dL), serum phosphorus 5.4 mg/dL (normal 3.0-4.5 mg/dL) and intact PTH 526 pg/ml (normal 14-72 pg/ml).
What vitamin D preparation would be most useful in treating this patient? A. Cholecalciferol (vitamin D3) B. Calcitriol (Active D3) |
B. Calcitriol (Active D3)
(When a person has CKD they CAN'T ACTIVATE VIT. D) |
|
|
What are the main side effect of
calcitriol in a patient with secondary hyperparathyroidism from CKD? |
Hypercalcemia
Hyperphosphatemia ** Calcitriol increases both Ca+ and P+ absorption and will also increase bone resorption that gets rid of Ca+ and P+. BUT, calcitriol also works on the parathyroid gland and decreases PTH release) |
|
|
How can you treat the
hyperphosphatemia associated with CKD (and calcitriol use)? |
Diet
|
|
|
Name the 1,25(OH)2D3 analogues
|
Doxercalciferol - oral or IV
Paricalitol - IV |
|
|
What is the difference between
calcitriol and paricalcitol ? |
**Calcitriol**
binds really well to Vit. D receptors on both intestine AND parathyroid gland **Paricalcitol** only binds well to Vit. D receptors on parathyroid gland |
|
|
Lab results for a 58-year-old male with stage 5 CKD reveal the following. Serum total calcium 9.4 mg/dL (normal 9.0-11.0 mg/dL), serum phosphorus 5.4 mg/dL (normal 3.0-.5 mg/dL) and intact PTH 526 pg/ml (normal 14- 72 pg/ml).
What vitamin D preparation may be most useful in treating this patient? A. Vitamin D3 B. Calcitriol C. Paricalcitol |
Paracalcitol
** We want to give a drug that will not increase Ca+ and Phosphorus as much, BUT DECREASE PTH. The other drug choices would have increased Ca+ and P+ which would allow them to bind together and cause calcification of blood vessels** |
|
|
What drug can be used to
lower serum PTH levels in chronic kidney disease? A. Bisphosphonate B. Calcitonin C. Cinacalcet D. Sodium phosphate |
C. Cinacalcet
Sensitizes Ca+ receptors on PT gland which decreases PTH and Ca+ in serum |
|
|
Which agent works better in a patient with hypoparathyroidism?
Vitamin D or Calcitriol |
Calcitriol
|
|
|
How can you treat osteoporosis?
|
INHIBIT Osteoclasts
STIMULATE Osteoblasts |
|
|
Which agents will work on bone to inhibit osteoclast activity?
(select all that apply) A. Bisphosphonates B. Calcitriol C. Calcitonin D. Cinacalcet E. Paricalcitol F. Parathyroid hormone |
A. Bisphosphonates
C. Calcitonin |
|
|
What does exogenous (injected) PTH do to osteoBlast activity?
|
INCREASES OSTEOBLAST ACTIVITY
|
|
|
Which agents will work on bone to increase osteoblast activity?
(select all that apply) A. Bisphosphonates B. Calcitriol C. Calcitonin D. Cinacalcet E. Paricalcitol F. Parathyroid hormone |
F. Parathyroid hormone
** Exogenous PTH INCREASES OSTEOBLAST ACTIVITY ** |
|
|
What is the name of the recombinant PTH drug that can be given exogenously to increase osteoblast activity?
|
Teriparatide
|
|
|
MOA:
- PTH activates the PTH receptor on cells of the osteoblast lineage. - Continuous activation of the PTH receptor increases expression of M-CSF and RANK Ligand but reduces expression of osteoprotegerin (OPG) resulting in increased osteoclastogenesis and bone resorption. |
Teriparatide
(recombinant PTH) |

