![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
45 Cards in this Set
- Front
- Back
|
Primary vs. Secondary Adrenal Insufficiency
- Destruction of the adrenal cortex = Addison’s disease - Congenital adrenal hyperplasia |
Primary Adrenal Insufficiency
|
|
|
Primary vs. Secondary Adrenal Insufficiency
- Prolonged steroid use - Pituitary or hypothalamic dysfunction |
Secondary/Tertiary Adrenal Insufficiency
|
|
|
How does prolonged steroid use
cause adrenal insufficiency? A. Prolonged steroid use suppresses the hypothalamic-pituitary-adrenal (HPA) axis B. Prolonged steroid use up regulates the hypothalamic-pituitary-adrenal (HPA) axis |
A. Prolonged steroid use
suppresses the hypothalamic-pituitary-adrenal (HPA) axis |
|
|
↓CRH, ↓ACTH, Adrenal Atrophy
can be iatrogenically caused by |
Prolonged Steroid Use
|
|
|
How do you prevent/treat
adrenal insufficiency from steroid withdrawal? |
Slowly wean the patient off of steroids over time!
|
|
|
What is the major difference
between Addison’s disease and secondary adrenal insufficiency? A. Addison’s disease - decrease in cortisol, androgens and aldosterone - Secondary adrenal insufficiency - decrease in cortisol and androgens B. Addison’s disease - decrease in cortisol and androgens - Secondary adrenal insufficiency - decrease in cortisol, androgens and aldosterone |
Addison’s disease - decrease in cortisol, androgens and aldosterone
- Secondary adrenal insufficiency - decrease in cortisol and androgens |
|
|
Why do you see hyperkalemia with Addison’s disease, but not with secondary adrenal insufficiency?
|
RAAS system is still intact in Secondary Adrenal Insufficiency
(Addison's = ↓Aldosterone = ↟K+) |
|
|
Zona glomerulosa releases _____
|
mineralocorticoids
|
|
|
Zona fasiculata releases ___
|
glucocorticoids
|
|
|
Zona reticularis releases ____
|
Androgens
|
|
|
What would you most likely use to treat a patient with Addison’s disease?
|
Both mineralocorticoid and glucocorticoid
(Addison's = ↓mineralocorticoids, glucocorticoids and androgen) |
|
|
What would you most likely use to treat a patient with secondary adrenal insufficiency (eg pituitary tumor)?
|
Glucocorticoid Only!!
RAAS is still intact so you won't need a mineralocorticoid (Aldosterone) |
|
|
Primary vs. Secondary Adrenal Insufficiency
Tx: - Replacement therapy with a glucocorticoid + a mineralocorticoid |
Primary Adrenal Insufficiency
|
|
|
Primary vs. Secondary Adrenal Insufficiency
Tx: - Replacement therapy with a glucocorticoid |
Secondary Adrenal Insufficiency
|
|
|
There are many different
corticosteroids. What are the main differences between them? |
glucocorticoid potency
mineralocorticoid potency duration of action |
|
|
Short vs, Intermediate vs. Long Acting Glucocorticoids:
Hydrocortisone |
Short Acting Glucocorticoid
|
|
|
Short vs, Intermediate vs. Long Acting Glucocorticoids:
Prednisone |
Intermediate acting
(little to no mineralocorticoid activity) |
|
|
Short vs, Intermediate vs. Long Acting Glucocorticoids:
Dexamethasone |
Long acting (no mineralocorticoid activity)
|
|
|
With regards to glucocorticoids:
The longer the duration of action the ______ the potency (glucocorticoid or anti-inflammatory potency) |
more potent
|
|
|
Name the Mineralocorticoid Agent
|
Fludrocortisone
|
|
|
This is defined as:
- Acute exacerbation of chronic insufficiency, usually caused by sepsis or surgical stress - Adrenal hemorrhage - Steroid withdrawal |
Acute adrenocortical insufficiency
(Adrenal Crisis) |
|
|
What would you use to treat acute adrenal insufficiency (Adrenal Crisis) in a patient that is previously undiagnosed?
|
Dexamethasone
(Using hydrocortisone would throw off cortisol levels used for monitoring) |
|
|
What is the treament for acute adrenal insufficiency (Adrenal Crisis) in a patient that has been previously diagnosed?
|
Glucocorticoid - Hydrocortisone
|
|
|
Fludrocortisone is not used for
acute adrenal insufficiency. Why not? |
The patient will be hyponatremic and hyperkalemic!!
Fludocortisone takes way too long to correct insufficiency!! Use Saline! |
|
|
Why would you use a divided dose regimen with hydrocortisone to treat chronic adrenal insufficiency?
|
Hydrocortisone:
- Has a short half life -Mimics the normal circadian secretion of ACTH and Cortisol |
|
|
ACTH and cortisol secretion follow what kind of rhythm?
|
Circadian Rhythm
|
|
|
What is the primary treatment for chronic adrenal insufficiency?
|
Hydrocortisone
2/3 in morning 1/3 in afternoon or 3 divided doses daily |
|
|
If hydrocortisone is ineffective for a patient's chronic adrenal insufficiency, what other treatment could you use?
|
Intermediate or Long Acting Glucocorticoids
**Once a day at bedtime** |
|
|
What might be the advantage of using Intermediate or long acting
glucocorticoids for replacement therapy? |
- Short acting regimen does not reproduce the peak serum cortisol level that occurs before awakening in the morning
- Smoother response |
|
|
What would you expect to see in a patient who is taking too much
dexamethasone? (Pick 3) A. Hypotension B. Hypertension C. Skeletal muscle wasting D. Skeletal muscle buildup E. Increased susceptibility to infection F. Reduced susceptibility to infection |
B. Hypertension
C. Skeletal muscle wasting E. Increased susceptibility to infection |
|
|
What is the name of the mineralocorticoid that would be used in the treatment of Addison's disease (primary adrenal insufficiency)
|
fludrocortisone
|
|
|
What would you expect to see in a patient who is taking too much
fludrocortisone? (Pick 3) A. Hypotension B. Hypertension C. Dehydration D. Edema E. Hypokalemia F. Hyperkalemia |
B. Hypertension
D. Edema E. Hypokalemia (Too much aldosterone!!) |
|
|
A defect / deletion in genes encoding
adrenal steroidogenic enzymes causes what disease? A. Addison’s disease B. Congenital adrenal hyperplasia C. Cushing’s syndrome D. Familial hypercholesterolemia E. Grave’s disease F. Hashimoto’s disease |
B. Congenital adrenal
hyperplasia |
|
|
If there is a deficiency/mutation in
CYP21A2, the synthesis of cortisol and aldosterone is impaired. How does this affect serum levels of ACTH and adrenal androgens? |
Increased ACTH
Increased Androgen - Since there is no/reduced negative feedback on the hypothalamus and pituitary, there is an increased release of ACTH from the pituitary. - This causes hyperplasia of the adrenal cortex with increased production of adrenal androgens. |
|
|
What would you use to treat a
patient with congenital adrenal hyperplasia from a mutation in CYP21A2? |
Hydrocortisone (glucocorticoid)
Fludocortisone for "salt wasters" |
|
|
What would you use to treat a
patient with congenital adrenal hyperplasia from a mutation in CYP21A2? |
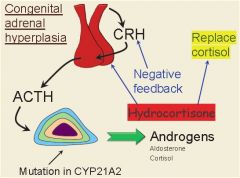
Hydrocortisone will not only treat the adrenal insufficiency, it will also feedback and inhibit the release of ACTH and reduce the production of adrenal androgens.
|
|
|
36-year-old female presents to her gynecologist with complaints of amenorrhea
and hirsutism. She has also noticed an increase in her weight (especially in the trunk region) and easy fatigability. On examination, she has a very rounded hirsute face with centripetal obesity. Her blood pressure is elevated, as is her weight compared with previous visits. On abdominal examination, she is noted to have striae and a male-like distribution of hair on the lower abdomen. A 24 hour urine test for free cortisol revealed elevated levels. A dexamethasone suppression test was performed (Low dose of dexamethasone was given at midnight and plasma cortisol levels were measured the following morning). What would the dexamethasone most likely do in this patient? (pick 2) A. Induce ACTH release B. Suppress ACTH release C. No effect on ACTH release D. Induce cortisol release E. Suppress cortisol release F. No effect on cortisol release |
**No effect on ACTH release**
(problem is with adrenal gland itself and not ACTH) ** No effect on cortisol release ** |
|
|
This is a Diagnostic test for Cushing’s syndrome
|
Dexamethasone suppression test
|
|
|
If a patient has a pituitary adenoma, what affect will a dexamethasone (low dose) suppression test show?
|
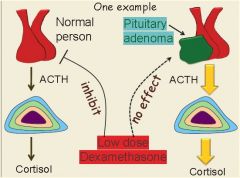
- In normal subjects, the administration of dexamethasone results in the suppression of ACTH and cortisol secretion.
- In Cushing's syndrome of whatever cause, there is a failure of this suppression when low doses of dexamethasone are given. - High doses of dexamethasone, however, may inhibit ACTH and cortisol secretion from a pituitary tumor (Cushing’s disease), but usually not from an ectopic ACTH secreting tumor. |
|
|
Main causes of Cushing’s syndrome (besides steroid use)?
|
Cushing’s Disease (pituitary tumor)
Ectopic ACTH producing tumor Adrenal Tumor/hyperplasia |
|
|
What is the main treatment
for Cushing’s syndrome? |
Surgery!!
Remove whatever is causing extra cortisol release |
|
|
if you can’t do surgery, or
it didn’t work well enough to reduce the hypercortisolism, what drug could you use to cause a medical adrenalectomy? |
Mitotane
|
|
|
This drug causes a Medical
adrenalectomy |
Mitotane
|
|
|
MOA: Cushing's
Inhibit different enzymes in corticosteroid biosynthesis |
Ketoconazole
|
|
|
What is the name of the anti-fungal drug that also acts as a steroid synthesis inhibitor?
|
Ketoconazole
|

