![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
|
Which is the most common location of a pituitary adenoma - Anterior or Posterior Pituitary? What is the result?
|
Anterior Pituitary
Excess production of hormones |
|
|
What are the most commonly produced hormones by pituitary adenomas?
|
Prolactin
Growth Hormone ACTH ** "PGA" ** |
|
|
What are the most common functional pituitary adenomas? (1st and 2nd)
|
1st -Prolactinomas
2nd -Growth hormone Secreting |
|
|
Abnormal ↑GH before closure of epiphyses
What does this cause? Age? |
Gigantism
Children |
|
|
Abnormal ↑GH after closure of epiphyses
What does this cause? Age? |
Acromegaly
Adults |
|
|
Clinical:
• Growth is most conspicuous in skin and soft tissues • Viscera (thyroid, heart, liver, and adrenals) • Bones of the face, hands, and feet - Hands and feet are enlarged with broad, sausage-like fingers |
Acromegaly
(↑GH in adults) |
|
|
Clinical:
• Bone density may be increased (hyperostosis) in both the spine and the hips • Enlargement of jaw results in protrusion (prognathism), with broadening of the lower face • Changes develop for decades before being recognized |
Acromegaly
(↑GH in adults) |
|
|
Failure to suppress GH production in response to an oral load of glucose is one of the most sensitive tests for _______
|
Acromegaly
|
|
|
Dx of Gigantism/Acromegaly:
- Persistently elevated levels of GH stimulate the hepatic secretion of ______, which causes many of the clinical manifestations*** |
IGF-1 (somatomedin C)
|
|
|
What is the "mass effect" regarding pituitary adenomas?
|
Larger lesions typically extend superiorly through the diaphragm sella into the suprasellar region, where they often compress optic chiasm and adjacent structures
|
|
|
Lateral expansion of pituitary tumor may compress CN VI (abducens n.) and lead to _______
|
lateral rectus palsy
|
|
|
Why would visual disturbances be a likely first sign of pituitary adenoma?
|
Mass effect
Compression of the optic chiasm |
|
|
What are "invasive pituitary adenomas"?
|
Infiltrate of neighboring tissues:
-Cavernous and sphenoid sinuses -dura -brain itself (Often have ↑ Intracranial Pressure) |
|
|
What is the name of a cyst on the anterior pituitary gland?
|
Craniopharyangioma - Rathke Cleft Cyst
|
|
|
- Mass effect of embryologic remnant, grows and accumulates
**Gooey material, “machine oil” = BUZZWORD** - Forms an expanding mass arising in the sella turcica -most are suprasellar |
Craniopharyangioma - Rathke Cleft Cyst
|
|
|
Name the most common lesions of the posterior pituitary gland (2)
|
**SIADH**
(Inappropriately high levels of ADH) **Diabetes insipidus** (deficiency of ADH) |
|
|
- Characterized by polyuria due to an inability of the kidney to resorb water properly
- Pts who can drink water can generally compensate for urinary losses - Pts who are obtunded, bedridden, or otherwise limited in their ability to obtain water may develop life-threatening dehydration |
**Diabetes insipidus**
(deficiency of ADH) |
|
|
Clinical:
- Causes resorption of excessive amounts of free water, resulting in hyponatremia - Clinical manifestations are dominated by hyponatremia, cerebral edema, and resultant neurologic dysfunction |
**SIADH**
(Inappropriately high levels of ADH) |
|
|
How much ischemia can the anterior pituitary tolerate before hyopituitarism develops?
|
>75% damage --> hyopituitarism
|
|
|
- Post-partum necrosis of anterior pituitary
- Most common form of clinically significant ischemic necrosis of the anterior pituitary - Result of obstetric hemorrhage or shock |
Sheenan Syndrome
|
|
|
- During pregnancy the anterior pituitary enlarges to almost twice its normal size
- This expansion is not accompanied by an increase in blood supply from the low-pressure venous system, thus-->there is relative anoxia - Further reduction in blood supply caused by obstetric hemorrhage or shock may precipitate infarction of the anterior lobe |
Sheenan Syndrome
|
|
|
You are looking at a slide of anterior pituitary tissue and see an infarcted necrotic area.
You also note ghost architecture What is going on? |
Sheenan Syndrome
|
|
|
When hyperthyroidism is secondary to hormone leakage out of a non-hyperactive gland it is called ______
|
thyrotoxicosis
|
|
|
What are the most common causes of hyperthyroidism? (4)
|
• Diffuse hyperplasia associated with Graves disease – 85% of cases
• Administration of exogenous thyroid hormone • Hyperfunctional multinodular goiter • Hyperfunctional adenoma of thyroid |
|
|
What is the earliest and most consistent sign of hyperthyroidism?
|
**Cardiac Signs**
Tachycardia, palpitations, cardiomegaly, arrythmias (a-fib) |
|
|
What is the skin like in a patient with hyperthyroidism?
|
Warm, moist and flushed
(d/t ↑ blood flow and peripheral VD) |
|
|
A patient presents with tachycardia, a wide, staring gaze, tremors, flushed skin and weight loss with a normal diet. What are you thinking?
|
Hyperthyroidism
|
|
|
• Associated with:
- Dietary iodine deficiency and endemic goiter - Biosynthetic defect in hormone synthesis Clinical features Impaired development of the skeletal system and CNS: - Short stature - Coarse facial features - Protruding tongue - Wide set eyes - Severe MR - Umbilical hernia |
Cretinism
(Hypothyroidism) |
|
|
What is the most common manifestation of thyroid disease?
|
Goiter/Enlargement
|
|
|
Diffuse vs. Multinodular Goiters:
- Diffuse involvement of entire gland without nodularity - Enlarged follicles are filled with colloid–colloid goiter - Endemic – areas where low levels of iodine—see in mountainous areas – Alps, Andes, Himalayas - Sporadic – peak incidence in young adult women |
Diffuse (Simple) Goiter
|
|
|
Diffuse vs. Multinodular Goiters:
Causes: • Ingestion of substances that interfere with hormone synthesis (veggies & plants) • Hereditary enzymatic defects • Most related to iodine use/dietary cause |
Diffuse (Simple) Goiters
(may not be huge or noticeable) |
|
|
- Most long standing simple goiters are ______
|
multinodular
|
|
|
Diffuse vs. Multinodular Goiters:
- May be nontoxic or may induce thyrotoxicosis—HIGH TH PRODUCTION* • Produce most extreme thyroid enlargement Clinically: • Signs and symptoms of mass • Occasionally thyrotoxicosis – rarely hypothyroidism |
Multinodular Goiters
|
|
|
Diffuse vs. Multinodular Goiters:
Micro: - See VERY LARGE follicles |
Multinodular Goiters
|
|
|
- Terminal event (death)= infiltration of vessels**
—infiltration of carotids, etc - Usually not d/t mets, more so mortality is d/t local structure involvement/destruction |
Thyroid Carcinoma
|
|
|
____ is mutated in most families with multiple endocrine neoplasia type II (Men II)
|
RET gene
|
|
|
What is the major risk factor for Thyroid Carcinoma?
|
Exposure to ionizing radiation
|
|
|
What is the triad seen in multiple endocrine neoplasia type II (Men II)
|
1) medullary thyroid cancer
2) pheochromocytoma 3) hyperparathyroidism |
|
|
• May present as asymptomatic thyroid nodule, or as a mass in cervical LN
• Clinical Manifestations: - Hoarseness, dysphagia, cough, dyspnea—all suggest advanced disease |
Papillary Thyroid Carcinoma
|
|
|
What is the most common form of thyroid carcinoma?
|
Papillary
|
|
|
Which thyroid carcinoma is increased in areas with iodine deficiency?
|
Follicular
(10-20% thyroid carcinomas) |
|
|
Which two forms of thryoid carcinoma have the worst prognosis?
|
Medullary
Anaplastic |
|
|
This type of thyroid neoplasm has an awful prognosis.
• Neuroendocrine neoplasms: - Secrete calcitonin and possibly other products • May present as single or multiple thyroid nodules involving both lobes |
Medullary
(5% thyroid carcinomas) |
|
|
What is the difference between Sporadic and Familial Medullary thyroid Carcinomas?
|
Sporadic = one lobe
Familial = bilateral and multicentric |
|
|
Which thyroid carcinoma has an awful prognosis.
• Aggressive, undifferentiated tumors of follicular epithelium • Most common in elderly; peak age >60 • Lymphoma link • Poor prognosis with death usually 2° to local aggressive growth • Women >men |
Anaplastic
(<5% thyroid carcinomas) |
|
|
- Activity of glands is controlled by level of free ionized calcium in blood
↓ levels of ionized calcium stimulate synthesis and secretion of this gland's main hormone |
Parathyroid Glands --> secrete PTH
|
|
|
- Derived from pharyngeal pouches
- Usually four glands (upper and lower poles of each thyroid lobe) - 10% of population only have 2 or 3 glands - Yellow-brown, ovoid gland - Two cell types: chief cell (mostly) and oxyphil cell |
Parathyroid Glands
|
|
|
What is the most common cause of the loss of the Parathyroid Glands?
**** |
**Thyroidectomy = difficult because often also take out PT accidentally
Pt. develops HYPOcalcemia ! ! ! |
|
|
What is a congenital loss of the parathyroid glands where there is failure of development of 3rd and 4th pharyngeal pouches before the 8th week of gestation?
|
Di-George Syndrome
|
|
|
Primary Hyperparathyroidism vs. Hypoparathyroidism vs. Pseudohypoparathyroidism:
Bone disease – pain 2° to fractures due to osteoporosis Renal disease – stones & obstructive uropathy GI – constipation, nausea, peptic ulcers, pancreatitis, gallstones CNS – depression, lethargy, eventually seizures Neuromuscular – weakness, fatigue Cardiac – aortic & mitral valve calcifications |
Primary Hyperparathyroidism
|
|
|
Primary Hyperparathyroidism vs. Hypoparathyroidism vs. Pseudohypoparathyroidism
Neuromuscular – tetany, muscle cramps, convulsions Mental status – irritability, psychosis Intracranial: Parkinsonian-like movement disorders, intracranial pressure & papilledema Ocular – calcification of lens, cataract formation Cardiac – conduction defects which produce prolongation of QT interval |
Hypoparathyroidism
|
|
|
Primary Hyperparathyroidism vs. Hypoparathyroidism vs. Pseudohypoparathyroidism
- Abnormalities in the PTH receptor complex and loss of responsiveness to PTH - Causes hypocalcemia, compensatory parathyroid hyperfunction - Short stature - Round face - Short neck - Short metacarpals and metatarsals |
Pseudohypoparathyroidism
|
|
|
A patient with short stature, a round face and short neck has an x-ray that shows shortness of 4th and 5th metacarpal bones
|
Pseudohypoparathyroidism
|
|
|
hyperparathyroidism vs. non-parathyroid disease
Labs: Serum PTH levels are inappropriately ↑ for level of calcium **** |
hyperparathyroidism
|
|
|
hyperparathyroidism vs. non-parathyroid disease
Labs: Serum PTH levels are ↓ or undetectable during hypercalcemia |
non-parathyroid disease
|
|
|
Most common cause of primary hyperparathyroidism
Almost always solitary Technetium-99m-sestamibi scan–area of increased uptake Gross: - Tan fleshy tumor - Circumscribed, solitary mass - Measuring 1 -3 cm in diameter - Hemorrhagic areas are common - Cystic changes occasionally seen - Other three glands tend to be atrophic Micro: - Rim of normal parathyroid, admixed with adipose cells |
Parathyroid Adenoma
|
|
|
You are looking at a slide of a patient with hyperparathyroidism and see:
-Rim of normal parathyroid, admixed with adipose cells |
Parathyroid Adenoma
|
|
|
Primary Adrenal Neoplasms:
What shows up more in adults, Adenomas or Carcinomas? |
Adenomas and carcinomas are equally common in adults
|
|
|
Primary Adrenal Neoplasms:
What shows up more in KIDS, Adenomas or Carcinomas? |
Carcinomas > adenomas in children
|
|
|
Primary Adrenal Neoplasms:
Which has a higher level of CORTISOL, adenomas or carcinomas? |
Levels of cortisol > with carcinoma than adenoma
|
|
|
What is the most common cause of pituitary hypersecretion in young adults leading to Cushing Syndrome?
|
ACTH-producing pituitary adenoma
|
|
|
- About 10% of endogenous Cushing syndrome
- Most common in men in 40-50’s **Most commonly seen with** • Small cell carcinoma of lung • Carcinoid tumors of bronchus or pancreas • Medullary cancer of thyroid • Islet cell tumors of the pancreas - Adrenals are bilaterally hyperplastic |
Ectopic ACTH Production
|
|
|
What is the most common overall cause of Hypercortisolism (Cushing Syndrome) ?
|
Exogenous glucocorticoids (Rx)
|
|
|
Ectopic secretion of ACTH is most commonly seen with what? (4)
|
• Small cell carcinoma of lung
• Carcinoid tumors of bronchus or pancreas • Medullary cancer of thyroid • Islet cell tumors of the pancreas |
|
|
A middle-aged woman presents with hypertension, hypokalemia:
Routine Panels Show: high serum aldosterone low serum renin |
Conn Syndrome
(solitary aldosterone-secreting adenoma) |
|
|
Buzzwords:
-HTN -Hypokalemia -Middle-aged woman -HIGH serum aldosterone -LOW serum renin |
Conn Syndrome
(solitary aldosterone-secreting adenoma) |
|
|
“Rule of 10’s”
- 10% occur in children - 10% are bilateral - 10% occur outside the adrenal gland - 10% are malignant - 10% are familial (MEN II & MEN III) |
Pheochromocytoma
|
|
|
What is the “Rule of 10’s” regarding pheochromocytoma? (5)
|
- 10% occur in children
- 10% are bilateral - 10% occur outside the adrenal gland - 10% are malignant - 10% are familial (MEN II & MEN III) |
|
|
Pheochromocytoma is associated with _____ production and hypertension
|
catecholamine production and hypertension
|
|
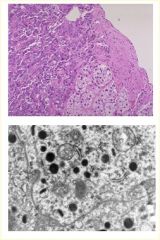
You are looking at a slides of adrenal cortical tissue and see:
**LM** - residual adrenal cortical tissue with darker cells on the left side **EM** neoplastic cells contain NEUROSECRETORY GRANULES containing CATECHOLAMINES |
Pheochromocytoma
|
|
|
How does a pheochromocytoma patient typically present?
|
Episodic HTN
|
|
|
What is a classic EM finding for pheochromocytoma?
|
**neurosecretory granules***
Granules contain catecholamines |

