![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
53 Cards in this Set
- Front
- Back
|
What is the definition of hypoglycemia?
|
- Plasma glucose low enough to cause signs or symptoms including impairment of brain function
- Typically < 70 mg/dL AND Whipple's Triad: - Symptoms/signs consistent w/ hypoglycemia - Low measured plasma glucose concentration - Resolution of symptoms/signs with increasing plasma glucose |
|
|
What is Whipple's Traid?
|
- Symptoms/signs consistent w/ hypoglycemia
- Low measured plasma glucose concentration - Resolution of symptoms/signs with increasing plasma glucose |
|
|
What are the physiologic defenses against hypoglycemia?
|
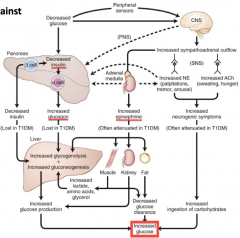
1. Reduction in insulin
2. Increase in glucagon - stimulates glycogenolysis and gluconeogenesis 3. Increase in epinephrine - increased AA substrate for gluconeogenesis 4. Decreased glucose clearance from the fat |
|
|
What hormone is regulated if glucose goes < 80-85 mg/dL? Effect?
|
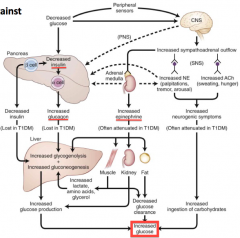
Decreased secretion of insulin from pancreas
|
|
|
What hormone is regulated if glucose goes < 65-70 mg/dL? Effect?
|
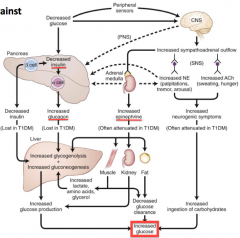
- Glucagon is released and acts on the liver to stimulate glycogenolysis and gluconeogenesis
- Epinephrine is released and acts on β2 receptors (increases substrates for gluconeogenesis) and on α2 receptors (inhibits insulin secretion) |
|
|
What hormone is regulated if glucose if hypoglycemia persists despite the action of insulin, glucagon, and epinephrine? Action?
|
- Cortisol - limits glucose utilization
- Growth hormone - enhances gluconeogenesis |
|
|
What is the effect of epinephrine release in hypoglycemia?
|
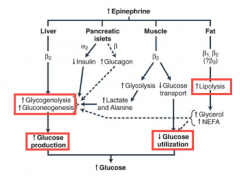
Liver
- Stimulates β2 receptors → ↑ glycogenolysis and gluconeogenesis → ↑ glucose production Pancreatic Islets: - α2 → ↓ insulin → - β → ↑ glucagon → → ↑ glycogenolysis and gluconeogenesis → glucose production Muscle - Stimulates β2 receptors → ↑ glycolysis → ↑ lactate and alanine → ↑ glycogenolysis and gluconeogenesis → glucose production - Stimulates β2 receptors → ↓ glucose transport → ↓ glucose utilization Fat - Stimulates β1 and β2 receptors → ↑ lipolysis → ↓ glucose utilization All ultimately lead to increase glucose to correct the hypoglycemia |
|
|
How does epinephrine release in response to hypoglycemia affect the LIVER to compensate for hypoglycemia?
|
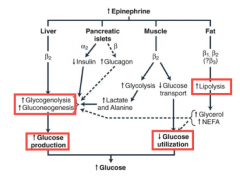
Epi stimulates β2 receptors → ↑ glycogenolysis and gluconeogenesis → ↑ glucose production
|
|
|
How does epinephrine release in response to hypoglycemia affect the PANCREATIC ISLETS to compensate for hypoglycemia?
|
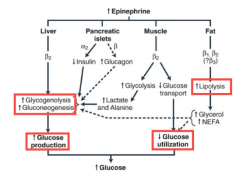
Epi stimulates α2 receptors, which ↓ insulin
Epi also stimulates β receptors, which ↑ glucagon ↓ insulin and ↑ glucagon → ↑ glycogenolysis and gluconeogenesis → glucose production |
|
|
How does epinephrine release in response to hypoglycemia affect the MUSCLE to compensate for hypoglycemia?
|
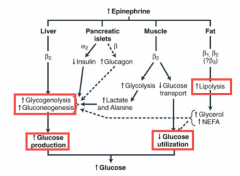
- Epi stimulates β2 receptors → ↑ glycolysis → ↑ lactate and alanine → ↑ glycogenolysis and gluconeogenesis → glucose production
- Stimulation of β2 receptors also ↓ glucose transport → ↓ glucose utilization |
|
|
How does epinephrine release in response to hypoglycemia affect the FAT to compensate for hypoglycemia?
|
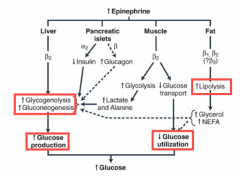
Epi stimulates β1 and β2 receptors → ↑ lipolysis → ↑ glycerol and NEFA → ↓ glucose utilization as well as ↑ glycogenolysis and gluconeogenesis which ↑ glucose production
|
|
|
What are the types of symptoms / signs of hypoglycemia?
|
- Neurogenic (autonomic)
- Neuroglycopenic |
|
|
What are the neurogenic (autonomic) signs/symptoms of hypoglycemia?
|
- Tremors
- Palpitations - Anxiety / arousal - Sweating - Hunger |
|
|
What are the neuroglycopenic signs/symptoms of hypoglycemia?
|
- Cognitive impairment
- Behavioral changes - Psychomotor abnormalities - Visual changes (tunneling, blurred vision) - Seizures - Coma |
|
|
What are the possible causes of hypoglycemia (differential)?
|
Drugs
- Insulin - Insulin secretogogue Critical illness - Liver, kidney, heart failure - Sepsis - Severe malnourishment Hormone deficiency - Cortisol Endogenous hyperinsulin - Insulinoma - Nesidioblastosis - Post-gastric bypass Insulin Auto-Immune - Ab to insulin - Ab to insulin receptor |
|
|
What drugs can cause hypoglycemia?
|
- Insulin (most common)
- Insulin secretogogues (sulfonylurea) |
|
|
What critical illnesses can cause hypoglycemia?
|
- Liver, kidney, and/or heart failure
- Sepsis - Severe malnourishment (including anorexia) |
|
|
What hormone deficiency can cause hypoglycemia?
|
Cortisol
|
|
|
What are some causes of endogenous hyperinsulin that can lead to hypoglycemia?
|
- Insulinoma
- Nesidoblastosis - Post-Gastric Bypass |
|
|
What auto-antibodies can cause hypoglycemia?
|
- Ab to insulin
- Ab to insulin receptor |
|
|
What is the term for hypoglycemia that begins < 4 hours after a meal? How do you confirm this diagnosis?
|
Reactive Hypoglycemia
- Only can diagnose if you confirm the glucose < 50 mg/dL and the presence of Whipple's Triad - Few patients w/ post-prandial symptoms truly have a low glucose Whipple's Triad - Symptoms/signs consistent w/ hypoglycemia - Low measured plasma glucose concentration - Resolution of symptoms/signs with increasing plasma glucose |
|
|
What are insulinomas?
|
Insulin-secreting tumors of pancreatic origin that cause hypoglycemia (rare)
|
|
|
How common are insulinomas?
|
- Only 1-4 people per million
- 1-2% of all pancreatic neoplasms |
|
|
What is the most common presentation of insulinomas?
|
90% are benign, solitary, intrapancreatic, and < 2 cm
|
|
|
How do you make the diagnosis of Insulinoma?
|
Hormonal studies when hypoglycemic
|
|
|
When should you use imaging for Insulinoma?
|
Only after you've made the diagnosis with hormonal studies when hypoglycemic
|
|
|
What is the function of a supervised fast? When does it end?
|
- Provoke hormone responses that maintain euglycemia
- Up to 72 hour fast that can be used to determine the presence and etiology of hypoglycemia - Stop if glucose is ≤ 45 mg/dl, or if ≤ 55 mg/dl with Whipple's triad, or if patient is showing signs/symptoms of hypoglycemia |
|
|
What is a normal response to a supervised fast? Why?
|
- Symptomatic hypoglycemia should not occur within the 72 hours because the body should be able to compensate via gluconeogenesis
- Maintain euglycemia - Insulin levels decline |
|
|
What are the abnormal responses to a supervised fast (at which point you would stop the test)?
|
- Glucose ≤ 45 mg/dL
- Signs / symptoms of hypoglycemia - Glucose ≤ 55 mg/dL + Whipple's Triad |
|
|
How dependent on gluconeogenesis are you after an overnight fast?
|
About 50% dependent on gluconeogenesis
|
|
|
How dependent on gluconeogenesis are you after 48 hours of fasting?
|
Completely dependent on gluconeogenesis
|
|
|
Why would you check a patient's C-peptide and proinsulin levels?
|

- If you are concerned if their hypoglycemia is caused by exogenous pharmacologic insulin
- Both proinsulin and C-peptide are secreted w/ endogenous insulin (including sulfonylurea, which stimulate insulin release) - Neither proinsulin or C-peptide will be present with exogenous pharmacologic insulin |
|
|
How would a patient with an Insulinoma present on a 72 hour fast?
|
- Plasma glucose declines to below 55 mg/dL
- Insulin levels were inappropriately elevated > 3 µU/mL |
|
|
If during a 72 hour fast your patient has a plasma glucose < 55mg/dL and insulin > 3 µU/mL, what do you think it is?
|
Insulinoma
- 90% sensitive - 70% specific |
|
|
What should you evaluate if your patient has a glucose < 55mg/dL during a 72 hour fast to determine the etiology?
|
- Insulin
- C-peptide - Sulfonylurea screen - Pro-insulin - β-hydroxybutyrate - Response to 1 mg IV glucagon |
|
|
What etiologies could cause hypoglycemia AND insulin to be elevated (>3µU/mL) during a 72 hour fast?
|
- Insulinoma
- Sulfonylurea - Insulin auto-immune - Exogenous insulin |
|
|
What can evaluating the C-peptide during a hypoglycemic reaction to a 72 hour fast tell you?
|
- Exogenous (pharmacologic) insulin will NOT contain C-peptide
- Sulfonylureas (ie, glyburide) and insulinomas will increase insulin AND C-peptide |
|
|
What can doing a Sulfonylurea screen during a hypoglycemic reaction to a 72 hour fast tell you?
|
Screen blood as sulfonylurea use and insulinoma are indistinguishable (both increase insulin and C-peptide)
|
|
|
What can evaluating the Proinsulin (< or > 5 pmol/L) during a hypoglycemic reaction to a 72 hour fast tell you?
|
Elevated (> 5 pmol/L) consistent with insulinoma
|
|
|
What can evaluating the β-hydroxybutyrate during a hypoglycemic reaction to a 72 hour fast tell you?
|
- Insulin has an anti-ketogenic effect
- Insulinoma patients have lower levels when fasting - At the end of the fast, insulinoma patients will have < 2.7 mmol/L - A progressive rise after 18 hours could also indicate a negative fast |
|
|
What can evaluating the response to 1 mg IV glucagon during a hypoglycemic reaction to a 72 hour fast tell you?
|
- Insulin is antiglycogenolytic
- Hyperinsulinemia permits the retention of glycogen within the liver - Patients with insulin mediated hypoglycemia respond to a 1 mg of IV glucagon with a subsequent increase in plasma glucose at the end of a supervised fast |
|
|
When would you screen for sulfonylurea use?
|
- After a hypoglycemic reaction to a 72 hour fast in which the patient also has elevated insulin and elevated C-peptide
- Insulinoma and sulfonylurea drug use are indistinguishable without the screen |
|
|
How can you confirm if your patient has insulin mediated hypoglycemia?
|
They should respond with increased glucose to a 1 mg IV of glucagon after a supervised fast
|
|
|
If you are on sulfonylurea or insulin, what would you consider hypoglycemic?
|
< 70 mg/dL
|
|
|
If you are not on sulfonylurea or insulin, what would you consider hypoglycemic?
|
If glucose is low and Whipple's triad
|
|
|
Case 1: 57 yo female reports multiple episodes of "not feeling right" for two months. She has episodes of heart racing, sweating, weakness, anxiety, confusion, and tunnel vision. Episodes are more often after she skips lunch. She gets relief by eating and carries juice with her. She has gain 15 pounds and has a history of anxiety and HTN.
Meds are alprazolam and HCTZ. Denies history of diabetes but reports her husband has T2DM and takes glyburide (sulfonylurea) and long actin insuline glargine. She appears well nourished, alert, oriented, and feeling well. No hx of liver disease and has 1-2 drinks / week. Which of her signs/symptoms is the most concerning for hypoglycemia? |
Vision changes
|
|
|
Case 1: 57 yo female reports multiple episodes of "not feeling right" for two months. She has episodes of heart racing, sweating, weakness, anxiety, confusion, and tunnel vision. Episodes are more often after she skips lunch. She gets relief by eating and carries juice with her. She has gain 15 pounds and has a history of anxiety and HTN.
Meds are alprazolam and HCTZ. Denies history of diabetes but reports her husband has T2DM and takes glyburide (sulfonylurea) and long actin insuline glargine. She appears well nourished, alert, oriented, and feeling well. No hx of liver disease and has 1-2 drinks / week. What is the next most reasonable diagnostic or treatment plan? |
Arrange for a 72 hour supervised fast
|
|
|
Case 1: 57 yo female reports multiple episodes of "not feeling right" for two months. She has episodes of heart racing, sweating, weakness, anxiety, confusion, and tunnel vision. Episodes are more often after she skips lunch. She gets relief by eating and carries juice with her. She has gain 15 pounds and has a history of anxiety and HTN.
Meds are alprazolam and HCTZ. Denies history of diabetes but reports her husband has T2DM and takes glyburide (sulfonylurea) and long actin insuline glargine. She appears well nourished, alert, oriented, and feeling well. No hx of liver disease and has 1-2 drinks / week. Has the patient fulfilled the criteria of Whipple's triad? |
No - she does not have documented hypoglycemia, but she does have signs/symptoms of hypoglycemia that resolve with eating (but we need glucose values to confirm)
|
|
|
Case 1: 57 yo female reports multiple episodes of "not feeling right" for two months. She has episodes of heart racing, sweating, weakness, anxiety, confusion, and tunnel vision. Episodes are more often after she skips lunch. She gets relief by eating and carries juice with her. She has gain 15 pounds and has a history of anxiety and HTN.
Meds are alprazolam and HCTZ. Denies history of diabetes but reports her husband has T2DM and takes glyburide (sulfonylurea) and long actin insuline glargine. She appears well nourished, alert, oriented, and feeling well. No hx of liver disease and has 1-2 drinks / week. She has a supervised fast. Her finger stick glucose decreases to 48 mg/dL after 14 hours of fasting. She is confused and diaphoretic. Insulin level >3 and C-peptide elevated. What are the possible causes? |
- Insulinoma
- Hypoglycemia secondary to glyburide (sulfonylurea) |
|
|
Case 1: 57 yo female reports multiple episodes of "not feeling right" for two months. She has episodes of heart racing, sweating, weakness, anxiety, confusion, and tunnel vision. Episodes are more often after she skips lunch. She gets relief by eating and carries juice with her. She has gain 15 pounds and has a history of anxiety and HTN.
Meds are alprazolam and HCTZ. Denies history of diabetes but reports her husband has T2DM and takes glyburide (sulfonylurea) and long actin insuline glargine. She appears well nourished, alert, oriented, and feeling well. No hx of liver disease and has 1-2 drinks / week. She has a supervised fast. Her finger stick glucose decreases to 48 mg/dL after 14 hours of fasting. She is confused and diaphoretic. Insulin level >3 and C-peptide elevated. If the patient has an insulinoma, what do you anticipate the β-hydroxybutyrate level will be at the time of the hypoglycemia? |
β-Hydroxybutyrate will be low in fasting patients with insulinoma (should be < 2.7 mmol/L) because insulin has an anti-ketogenic effect and therefore would suppress β-hydroxybutyrate formation
|
|
|
What symptoms should greatly increase your suspicion for hypoglycemia?
|
Symptoms of neuroglycopenia
* Cognitive impairment - Behavioral changes - Psychomotor abnormalities * Visual changes (tunneling, blurred vision) - Seizures - Coma |
|
|
When evaluating hypoglycemia, what must you ensure when you measure insulin, C-peptide, and glucose?
|
They should be measured simultaneously at the exact time that the patient is having hypoglycemia (doesn't help you if they are not hypoglycemic)
|
|
|
When do you use imaging for hypoglycemia?
|
Only after you've made a biochemical diagnosis (eg, insulinoma); only use imaging to localize the etiology
|

