![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
|
What is Metabolic Syndrome also known as?
|
- Insulin Resistance Syndrome
- Syndrome X - Dysmetabolic Syndrome |
|
|
What is Metabolic Syndrome in general?
|
A constellation of metabolic derangements that increase the risk of developing type 2 diabetes mellitus and cardiovascular disease
|
|
|
What does insulin resistance (IR) and the resultant hyperinsulinemia lead to in Metabolic Syndrome?
|
Development of:
- Hypertension - Glucose intolerance - Dyslipidemia |
|
|
What can exacerbate insulin resistance in Metabolic Syndrome?
|
- Central obesity
- Genetics |
|
|
How do the individual disorders within metabolic syndrome affect your risk of developing cardiovascular disease?
|
Increase risk by 2-3 fold
|
|
|
How does metabolic syndrome affect your risk of developing diabetes mellitus?
|
Increases risk by 3-7 fold
|
|
|
What are the components for evaluating Metabolic Syndrome?
|
- Abdominal obesity (waist circumference)
- Triglycerides - HDL - HTN - Impaired fasting glucose / diabetes |
|
|
What are the criteria for a diagnosis of Metabolic Syndrome?
|
Need 3 or more criteria:
Abdominal Obesity (waist circumference): - Males: > 40 inches - Females: > 35 inches Hypertriglyceridemia - > 150 mg/dL Low HDL - Males: < 40 mg/dL - Females: < 50 mg/dL Hypertension - > 130 / 85 mmHg or on anti-HTN med Impaired fasting glucose or diabetes - > 100 mg/dL or taking insulin or hypoglycemic medication |
|
|
What waist circumference meets criteria for Metabolic Syndrome?
|
- Males: >40 inches
- Females: >35 inches |
|
|
What triglyceride value meets criteria for Metabolic Syndrome?
|
> 150 mg/dL
|
|
|
What HDL value meets criteria for Metabolic Syndrome?
|
- Males: < 40 mg/dL
- Females: < 50 mg/dL |
|
|
What BP value meets criteria for Metabolic Syndrome?
|
> 130 / 85 mmHg or on anti-HTN medications
|
|
|
What fasting glucose value meets criteria for Metabolic Syndrome?
|
> 100 mg/dL fasting blood sugar OR taking insulin OR hypoglycemic medication
|
|
|
What is the consensus of the reason for Metabolic Syndrome development?
|
Develops d/t insulin resistance; exact etiology of insulin resistance is subject to debate
|
|
|
How does an expanded adipose tissue mass (obesity) affect the liver (pathophysiology of metabolic syndrome)?
|
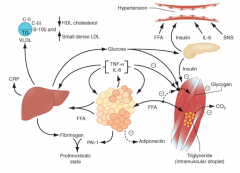
- The more adipose, the more FFAs
- FFAs result in increased production of glucose and TG - FFAs also induce secretion of VLDL - Reduced HDL and increased LDL |
|
|
How does an expanded adipose tissue mass (obesity) affect the muscles (pathophysiology of metabolic syndrome)?
|
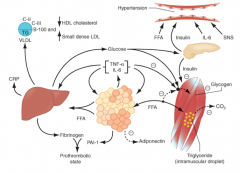
- The more adipose, the more FFAs
- FFAs reduce insulin sensitivity in muscle by inhibiting insulin-mediated glucose uptake - Leads to reduced glucose partitioning to glycogen and increased lipid accumulation in TG |
|
|
How does an expanded adipose tissue mass (obesity) affect the pancreas (pathophysiology of metabolic syndrome)?
|
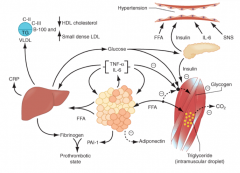
- The more adipose, the more FFAs
- FFAs increase circulating glucose - Increased FFAs and circulating glucose increase pancreatic insulin secretion, resulting in hyperinsulinemia |
|
|
How does hyperinsulinemia from the pancreas (in response to elevated circulating glucose and FFAs) affect the vascular system (pathophysiology of metabolic syndrome)?
|
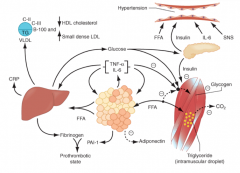
- Hyperinsulinemia may enhance sodium reabsorption and increase SNS activity
- These contribute to HTN, as might increased levels of circulating FFAs |
|
|
How does the pro-inflammatory state contribute to insulin resistance (pathophysiology of metabolic syndrome)?
|
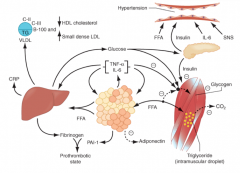
- Enhanced secretion of IL-6 and TNF- α produced by adipocytes and macrophages results in more insulin resistance
- Also increases lipolysis of adipose tissue TG stores to FFAs (exacerbating the increased FFAs) - IL-6 and other cytokines also enhance hepatic glucose production, VLDL production by liver, and insulin resistance in muscle |
|
|
Which inflammatory state mediators are involved in the pathophysiology of metabolic syndrome? What produces these mediators?
|
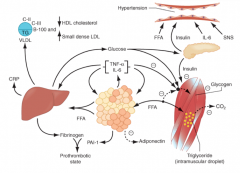
- IL-6
- TNF-α Produced by adipocytes and monocyte-derived macrophages |
|
|
What is the effect of IL-6 and TNF-α on the pathogenesis of Metabolic Syndrome?
|
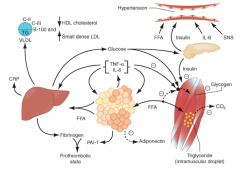
- Increases insulin resistance
- Increases lipolysis of adipose tissue TG stores to circulating FFAs - IL-6 and other cytokines also enhance hepatic glucose production, VLDL production by liver, and insulin resistance in muscle |
|
|
What do cytokines and FFAs increase production of? Source? Effect?
|
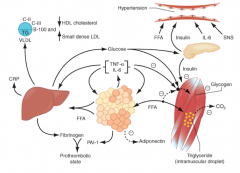
- Increase production of Fibrinogen by liver
- Increase production of Plasminogen Activator Inhibitor 1 (PAI-1) by adipocytes * Leads to a pro-thrombotic state - Cytokines also increase C-Reactive Protein (CRP) from liver |
|
|
What is the source of C-Reactive Protein? Stimulation for production?
|
- From liver
- Stimulated by high levels of circulating cytokines |
|
|
Reduced production of what is associated with metabolic syndrome?
|
Reduced production of:
- Anti-inflammatory and Insulin-Sensitizing Cytokine Adiponectin |
|
|
What are the key factors in the development of Metabolic Syndrome?
|
- Insulin resistance
- Hyperinsulinemia |
|
|
Insulin resistance in Metabolic Syndrome affects what tissues?
|
- Fat
- Muscle tissue |
|
|
How can the endocrine pancreas delay the development of diabetes (early on)?
|
By producing enough insulin to overcome the insulin resistance (hyperinsulinemia)
|
|
|
What are the affects of the compensatory hyperinsulinemia by the endocrine pancreas?
|
Adverse effects on tissues such as muscle, fat, liver, and endocrine pancreas itself
|
|
|
What distribution of fat/obesity is associated w/ Metabolic Syndrome?
|
- Abdominal obesity is associated w/ insulin resistance and hyperinsulinemia
- Upper-body obesity (visceral fat) is more strongly correlated to insulin resistance than lower-body obesity (subcutaneous fat) - This may be related to the higher level of lipid accumulation in the muscles and liver of patients with upper-body obesity |
|
|
How does obesity affect the regulation of body fat metabolism?
|
Leads to abnormal regulation of:
- Body fat metabolism - Storage by adipokines (cell to cell signaling cytokines) |
|
|
What are adipkines? What are the types?
|
Cell to cell signaling cytokines
- Leptin - Adiponectin - Resistin |
|
|
How does obesity affect Leptin (an adipokine)?
|
- Leptin from adipose cells normally controls the appetite center of the brain
- It is ineffective (leptin resistance) |
|
|
How does obesity affect Adiponectin and Resistin (adipokines)?
|
- Adiponectin and Resistin levels are lower with obesity
- This increases insulin resistance - Adiponectin decreases with insulin resistance - Resistin increases with insulin resistance |
|
|
What happens with prolonged stimulation of β-cells (compensatory mechanism to release more insulin d/t resistance)?
|
- Initially they are able to compensate by increasing insulin synthesis and release (hyperinsulinemia)
- Prolonged stimulation leads to "β-cell failure" such that insulin levels decrease - This leads to frank hyperglycemia (T2DM) |
|
|
What can lessen insulin resistance and increase insulin secretion in patients with "β-cell failure"?
|
Exercise and weight loss
|
|
|
What happens to the levels of different adipokines and TNF-α with insulin resistance?
|
- Adiponectin and Leptin DECREASE
- TNF-α and Resistin INCREASE |
|
|
What are the possible explanations for the mechanisms of insulin resistance?
|

- Inflammation (left)
- Lipid overload (right) - Lipotoxicity |
|
|
What is the mechanism of the Inflammation hypothesis of Insulin resistance?
|

- Enlarged fat cells attract macrophages and excrete inflammatory signals that work in the muscle cell vis kinase JNK
- Inflammatory signals block an insulin receptor substrate (IRS-1) - This shuts down the insulin-signaling pathway |
|
|
What is the mechanism of the lipid-overload hypothesis of Insulin resistance?
|

- Enlarged fat cells leak FFAs
- This causes diacylglycerols (DAGs) to accumulate in muscle cells - These inhibit insulin signaling through novel protein kinase Cs (nPKCs) and then block the insulin receptor substrate (IRS-1) |
|
|
What is the theory of lipotoxicity for mediating insulin resistance?
|
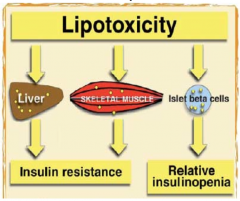
- Increased fatty acids from adipocytes leads to changes in post-insulin receptor function in muscle cells
- Decreases in IRS-1 function leads to a decrease in insulin-mediated glucose uptake, leading to hyperglycemia - Lipotoxicity is also thought to be involved in the "β-cell failure" (indirectly) |
|
|
How does abnormal / decreased Insulin Receptor Substrate (IRS-1) function affect glucose?
|
- Decreased IRS-1 function leads to a decrease in insulin-mediated glucose uptake
- Leads to hyperglycemia |
|
|
How does insulin resistance and hyperinsulinemia lead to vascular / heart disease?
|
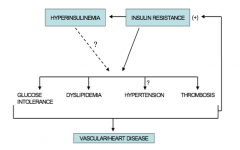
Insulin resistance leads to:
- Glucose intolerance - Dyslipidemia - Hypertension - Thrombosis These all lead to vascular / heart disease, and perpetuate the insulin resistance |
|
|
How common is Metabolic Syndrome in the US?
|
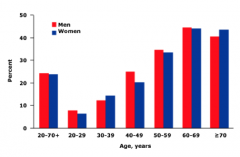
- 22% of all US adults (47 million total)
- Prevalence increases with age |
|
|
What are the gender and ethnic differences in prevalence of Metabolic Syndrome in the US?
|
African Americans:
- Women had 57% higher prevalence than men - Overal 22% prevalence Mexican Americans: - Women had 26% higher prevalence than men - Highest age-adjusted prevalence of metabolic syndrome (32%) White Americans: - Overall 24% prevalence Native Americans - Other reports suggest this is the most commonly affected group |
|
|
How does weight affect the prevalence of Metabolic Syndrome?
|
- 5% of normal weight
- 22% of over weight - 60% of obese individuals |
|
|
What is an underweight BMI?
|
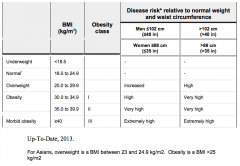
< 18.5 kg/m2
|
|
|
What is a normal BMI?
|
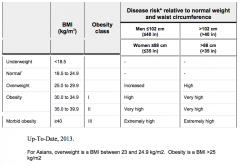
18.5 - 24.9 kg/m2
Except: Asians 18.5 - 23.0 kg/m2 |
|
|
What is an overweight BMI?
|
25.0 - 29.9 kg/m2
Except: Asians 23.0 - 24.9 kg/m2 |
|
|
What is an obese BMI?
|
Class I: 30.0 - 34.9 kg/m2
Class II: 35.0 - 39.9 kg/m2 Class III: ≥ 40.0 kg/m2 Except: Asians > 25 kg/m2 |
|
|
What are the risk factors for obesity?
|
- Low socioeconomic status
- Lack of physical activity / sedentary lifestyle - High carbohydrate diet - Smoking - Genetic predisposition - Use of atypical anti-psychotics |
|
|
Besides obesity, what other complications are associated with Metabolic Syndrome?
|
- Fatty liver disease (NASH)
- Polycystic ovary syndrome - Obstructive sleep apnea - Gout (hyperuricemia) - Increased risk of cancer |
|
|
What diet choices contribute to the development / risk for Metabolic Syndrome?
|
- Atherogenic diet: rich in saturated fat (>10%), cholesterol (>300mg/day), and trans-fatty acids
- A diet high in carbohydrates |
|
|
What is the typical lipid profile in a patient with Metabolic Syndrome?
|
- Low HDL
- High TGs - Mild or moderately increased LDL (smaller and more atherogenic) |
|
|
What is the mechanism of increased FFAs being sent to the liver and increased VLDL production in Metabolic Syndrome?
|
Usually Lipoprotein Lipase and VLDL are suppressed by insulin, but when there is insulin resistance it leads to increased flux of FFAs tot he liver and increased VLDL production → increases circulating TG concentrations
|
|
|
What happens to the increased circulating TGs d/t insulin resistance?
|
- TGs are transferred to LDL and HDL
- VLDL particles gain cholesterol esters by action of cholesterol ester transfer protein (CETP) - Leads to increased catabolism of HDL particles by liver and loss of Apolipoprotein A (ApoA) resulting in low HDL - TG-rich LDL is stripped of its TGs, resulting in accumulation of atherogenic small, dense LDL particles |
|
|
What happens to the liver's production of glucose with insulin and with insulin resistance?
|
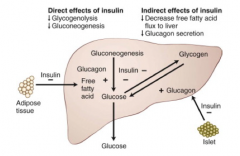
Normal insulin:
- Insulin suppresses hepatic glucose production directly and indirectly Insulin Resistance: - Inability of insulin to suppress lipolysis in adipose tissue and glucagon secretion by α cells in the Islets results in increased gluconeogenesis - Also, insulin inhibition of glycogenolysis is impaired - Both hepatic and peripheral insulin resistance results in abnormal glucose production by the liver |
|
|
What do the results of a fasting plasma glucose test tell you?
|
> 126 mg/dL = Diabetes Mellitus
100-125 mg/dL = Impaired Fasting Glucose / Pre-Diabetes < 100 mg/dL = Normal Glucose State |
|
|
What do the results of an oral glucose tolerance test tell you?
|
> 200 mg/dL = Diabetes Mellitus
140-199 mg/dL = Impaired Glucose Tolerance < 140 mg/dL = Normal Glucose State |
|
|
What are the non-pharmacologic therapies for Metabolic Syndrome?
|
- Dietary modifications aimed at weight loss
- Prevention of diabetes - Limit fats in the diet - Ingest more monounsaturated fats (e.g., olive or canola oil) - Physical activity of moderate intensity (i.e., brisk walking): 30 min daily - Smoking cessation - Consider bariatric surgery in the management of obesity |
|
|
What are the pharmacologic therapies for the treatment of the obesity component of Metabolic Syndrome? Mechanism?
|
Orlistat:
- Reversible inhibitor of gastric and pancreatic lipases - Inhibits absorption of dietary fats by 30% |
|
|
When should you consider giving your patient Orlistat for their Metabolic Syndrome? Uses?
|
- Use if they have not responded to diet and exercise
- Used for management of obesity, including weight loss and weight management (in conjunction with diet and exercise) |
|
|
What are the side effects of Orlistat?
|
- Headache
- Abdominal pain - Gas - Fecal urgency - Upper respiratory infection |
|
|
What are the pharmacologic therapies for the treatment of the hypertension component of Metabolic Syndrome?
|
First-line therapy:
- ACE-I: Angiotensin Converting Enzyme Inhibitor - ARB: AngII Receptor Blocker |
|
|
What are the pharmacologic therapies for the treatment of the dyslipidemia component of Metabolic Syndrome?
|
LDL Cholesterol:
- 1st line - Statins: HMG-CoA reductase inhibitors - 2nd line - Ezetimibe Hypertriglyceridemia: - Fibric Acid derivatives - Niacin - (Exercise and weight loss) Low HDL - Fibrates - Niacin - (Exercise and weight loss) |
|
|
What are the therapies for the treatment of the Pre-Diabetes component of Metabolic Syndrome?
|
- Diet, exercise, and weight loss
- Nutrition counseling - Metformin in select group of patients (eg, patients with class II or III obesity who are young and those w/ a history of gestational diabetes (GDM)) |
|
|
What are the therapies for the treatment of the Diabetes component of Metabolic Syndrome? Goal?
|
Goal: HbA1C < 7%
- 1st line: Metformin to improve insulin sensitivity - Some recommend Pioglitazone (a glitazone) |
|
|
What should you consider before prescribing a patient Pioglitazone (a glitazone) for their Diabetes in Metabolic Syndrome?
|
- Expensive
- Concerning side effects such as weight gain and pedal edema - Possible increased risk for bladder cancer - Increased risk of bone loss in prolonged treatment, especially in post-menopausal women |
|
|
How should you treat cardiovascular risk factors in patients with Metabolic Syndrome?
|
Consider aspirin:
- Aspirin should be started in patients w/ metabolic syndrome and an intermediate or elevated Framingham cardiovascular risk if there are no contraindications |
|
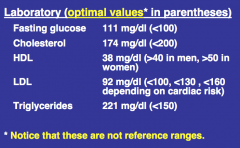
Case 1: 36 yo Latina, obese and sedentary. She has irregular menstrual periods every 4-6 weeks. She had a tubal ligation after the last pregnancy in 2011. She had gestational diabetes (GDM) in 2011 and her baby was 9 lbs 10 oz at 38 weeks. She has not retested for glucose tolerance after the pregnancy. Her parents both had diabetes.
Her BMI is 33, BP 126/82, waist circumference 34 inches (central weight distribution). She has acanthosis nigricans. Lab values shown. Does she have diabetes mellitus? Why? |
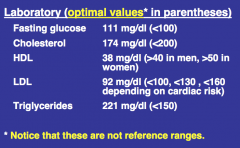
No (pre-diabetes because her fasting glucose was between 100-125 mg/dL)
|
|
|
How is the diagnosis of diabetes mellitus established?
a) 8 hour fasting glucose ≥125 mg/dl b) HbA1c ≥6.0% c) Two hour glucose >200 mg/dl with the standard 75 g oral glucose tolerance test d) Random glucose >175 mg/dl with symptoms of diabetes |
C - Two hour glucose >200 mg/dl with the standard 75 g oral glucose tolerance test
|
|
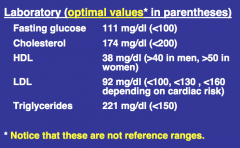
Case 1: 36 yo Latina, obese and sedentary. She has irregular menstrual periods every 4-6 weeks. She had a tubal ligation after the last pregnancy in 2011. She had gestational diabetes (GDM) in 2011 and her baby was 9 lbs 10 oz at 38 weeks. She has not retested for glucose tolerance after the pregnancy. Her parents both had diabetes.
Her BMI is 33, BP 126/82, waist circumference 34 inches (central weight distribution). She has acanthosis nigricans. Lab values shown. Does she meet criteria for Metabolic Syndrome? Which criteria does she meet / not meet? |
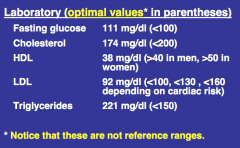
Yes (need 3 or more criteria)
Meets: - Hypertriglyceriemia: > 150 mg/dL - Low HDL: < 50 mg/dL - Impaired fasting glucose or diabetes: >100 mg/dL Does not meet: - Waist circumference: >35 inches - HTN: > 130/85 mmHg or on anti-HTN meds |
|
|
Case 1: 36 yo Latina, obese and sedentary. She has irregular menstrual periods every 4-6 weeks. She had a tubal ligation after the last pregnancy in 2011. She had gestational diabetes (GDM) in 2011 and her baby was 9 lbs 10 oz at 38 weeks. She has not retested for glucose tolerance after the pregnancy. Her parents both had diabetes.
Her BMI is 33, BP 126/82, waist circumference 34 inches (central weight distribution). She has acanthosis nigricans. Lab values shown. You establish that she has Metabolic Syndrome, what testing should be done next? |
Two hour glucose tolerance test
|

